🔰 IMPORTANT tips for clinical slides prep
https://youtu.be/htnim4qqmiQ?si=SbJnn5LiXAuMCBb3
Ulcer charting
🔴Why ulcer charting is done?
🟢To document morphology and size of ulcer
🟢Response to treatment
🔴 What are the causes of leg ulcers:
🟢 venous
🟢arterial
🟢mixed
🟢Hypertensive
🟢Malignancy
🟢Necrotizing vasculitis
🟢pyoderma gangrenosum
🟢Microvascular occlusive disorder
🌂Livedoid vasculopathy
🌂Connective tissue
disease
🌂cholesterol emboli
🟢Necrotizing bacterial infection( ecthyma gangrenosum,necrotizing cellulitis)
🟢deep dissecting hematoma
🟢Radiotherapy
🟢Prolidase deficiency
🟢Klinefelter syndrome
🟢Drugs:
🌂pentazocine
🌂warfarin
🌂steroids 🌂hydroxycarbamide
🔴 what are the main points for mangemnet of ulcers??
1.Wound documentation by ulcer charting and photography.
2.Microbiology
A swab from the wound base (after the removal of fibrin layers and biofilms)or a small tissue biopsy from the wound base– if feasible– yields more representative microbiology results than superficial swabs from necrotic material.
3.Histopathology of ulcer
4.Assessment of malnutrition
5.Pain assessment
6.Assessment of Quality of life
🔴 What are the Disorders associated with venous leg ulcers
🟢 Venous thromboembolism
🟢 Superficial venous thrombophlebitis
🟢 Varicose veins
🟢 Chronic venous insufficiency
🟢 Stasis dermatitis
🟢 Lipodermatosclerosis
🟢 Acroangiodermatitis
🟢 Obesity
🟢 Ankle joint ankylosis
🟢 Rheumatoid arthritis
🟢 Neuromuscular diseases with impact on venous calf pump ejection
🔴 What are the Disorders associated with mixed leg ulcers
🟢 Venous thromboembolism
🟢 Superficial venous thrombophlebitis
🟢 Varicose veins
🟢 Chronic venous insuffi ciency
🟢 Stasis dermatitis
🟢 Lipodermatosclerosis
🟢 Acroangiodermatitis
🟢 Obesity
🟢 Smoking
🟢 Diabetes
🟢 Hyperlipidaemia
🟢 Hypertension
🟢 Coronary heart disease
🟢 Stroke
🍀Pre procedure counseling
🍀What is an ulcer?
Ulcer is a break in the skin or mucous membraneswith
* associated necrosis
* Healswith scarring
🍀What is an erosion? Erosion is a break in skin or mucous membranes
without:
* associated necrosis &
* scarring
🍀What is the difference between edge and margin?
Margin is the junction between normal epithelium
and the ulcer. So it is the boundary of the ulcer.
Edge is the area between the margin and the floor of
the ulcer.
🍀 Is base and floor the same?
* Floor is the exposed surface of the ulcer which canbe both seen and felt on palpation. Floor is exposed surface within ulcer.
* base is thearea on which the ulcer rests. It cannot be seen but only felt.
🍀How often ulcer charting is done?
– For OPD patients-on every visit
– For admitted patients-once weekly
🍀 Difference between Doppler and duplex ultrasound?
* Doppler- superficial venous reflux
* Dupplex- deep venous reflux, any obstruction, architecture
🍀D/D of tender ulcers?
* Inflammatory (PG, PAN), panniculitis, hypertensive ulcers
* TB
* Malignant ulcers infiltrating pain nerve endings
🍀 Painless ulcers- DD?
– Syphilitic ulcers
– Trophic ulcers(leprosy/tabes dorsalis/Peripheralneuritis/Transverse myelitis)
– Deep fungal infections
– Cutaneous Tuberculosis
– Ulcerative DLE
– SCC, BCC
– Venous ulcers
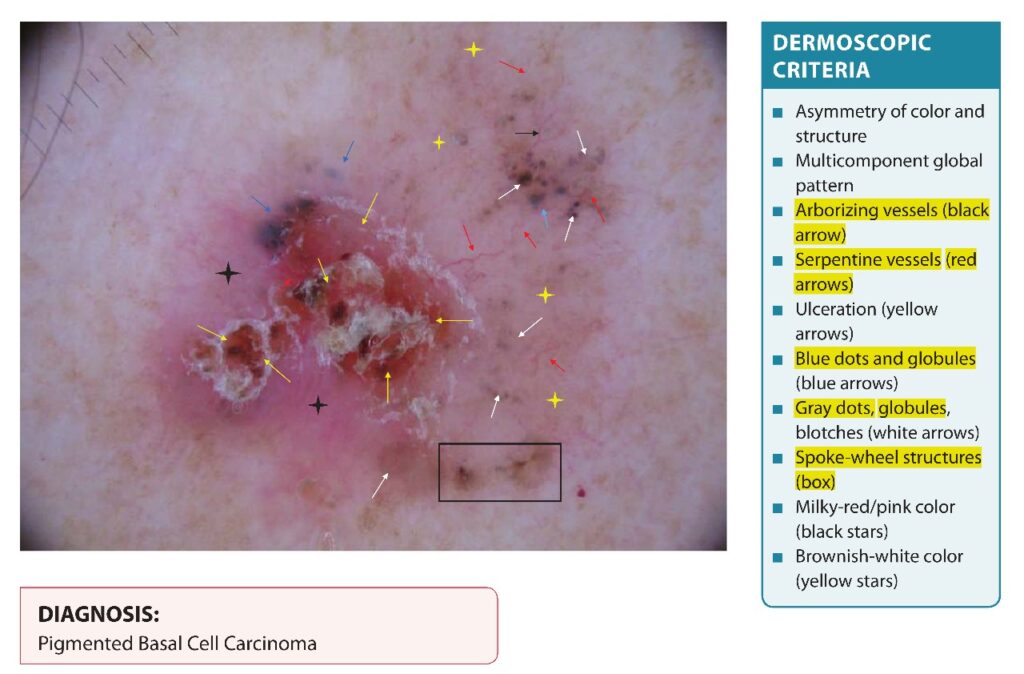
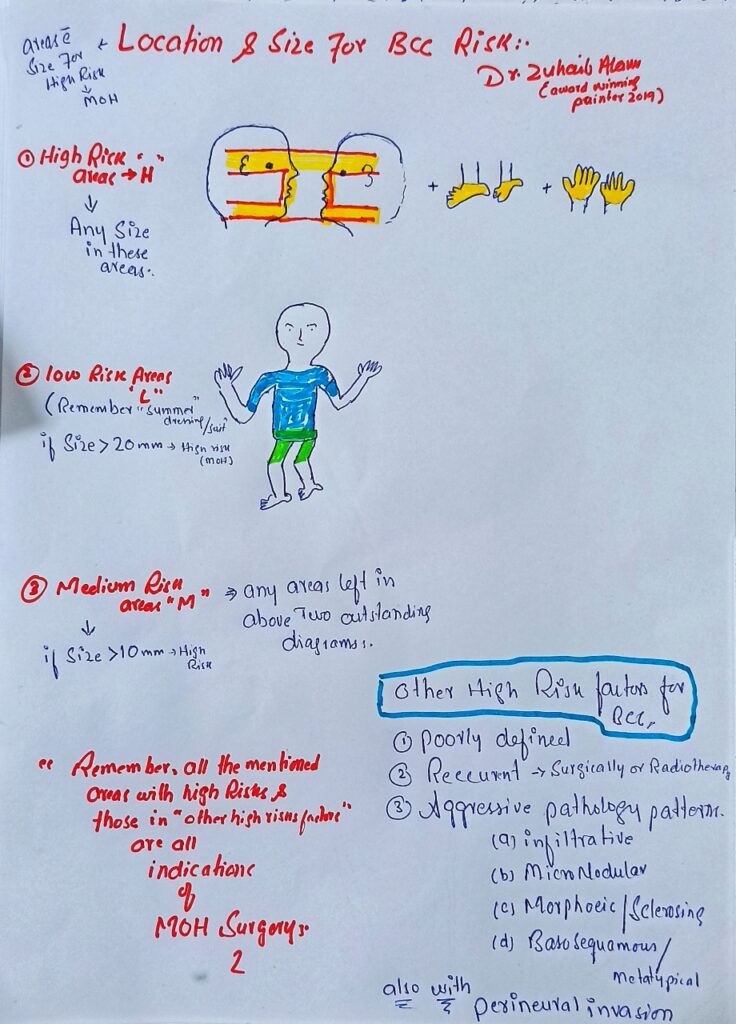
🛑 Risk factors for basal cell carcinoma??
🔹Intrinsic factors
• Fitzpatrick skin type I, II
• Iatrogenic immunosuppression
• Human immunodeficiency virus (HIV), acquired immune deficiency
syndrome (AIDS)
• Chronic lymphocytic leukaemia, non-Hodgkin lymphoma
• Previous history of basal cell carcinoma
• Photosensitising drugs, azathioprine
🔹Extrinsic factors
• High solar ultraviolet (UV) radiation
• Tanning bed, solarium use
• PUVA, narrow-band UVB phototherapy
• Ionising radiation
• Outdoor occupation
• Chronic arsenic exposure
🛑 GENETICS??
🔵 SPORODIC MUATAION IN PTCH1 GENE WHICH encodes transmembrane receptor of the diffusible morphogen protein sonic hedgehog (SHH)
🛑 TREATMENT OF ADVANCED CUTANEOUS BCC???
🔵 when tumors are neither surgically resectable nor curable by radiotherapy or when metastases have developed.
▪*Hedgehog signaling pathway inhibition
* ®Vismodegib
®Sonidegib
▪️, Immunotherapy with immune checkpoint inhibitors
anti-PD-1 antibodies->. Pembrolizumab, nivolumab, and cemiplimab.
CEMIPLIMAB is currently FDA-approved for locally advanced or metastatic BCC in patients previously treated with a hedgehog pathway inhibitor or for whom a hedgehog pathway inhibitor is inappropriate.

You don’t have to tell the risk factors to the patient.
You can ask them the risk factors such that you rule out them one by one in the given patient.
Like
Kia apkay kisi azaa ki pewandkari hui Hy , qowat mudafoat Kam krna wali dawa istemal KR rahay Hain? And so on
After this how do you proceed for investigations and staging .
If it’s a high risk area so you chose mohs. The examiner might ask have you ever managed bcc with Mohs . Be prepared what you ll say then.
And counselling for mohs should include that microscope s check krte Hain k cancer mukammal khtm ho Jaye ta k dobra na Phelay. (Recurrence)
6steps protocol for any bad news breaking (SPIKES):
S- setting up the interview.
P- patient’s perception.
I- invite patient to tell about his disease.
K- knowledge and information handed over to patient.
E- empathise.
S- strategy and summary.
🔴Setup:
- Arrange quite comfortable environment with a glass of water and some tissue papers.
- Introduction of doctor and patient.
- Match patient name with that of report.
- Ask the patient if he wants someone to be there with him while delivering the information.
🔴 Patient’s perception:
Take patient’s insight about his disease.
🔴Invitation:
Ask patient if he wants to have full information. Don’t bombarde him with all the information if he is not willing.
🔴Knowledge and information:
Break the bad news with empathy and pause.
🔴Empathise:
Use words like ap pareshan na hon, ye mushkil waqat hai, ap himmat se kam lyn, mujhe apki halat ka andaza hai etc.
🔴Strategy and summary:
Explain to patient what is melanoma.
Risk factors.
How to diagnose.
Workup for metastasis and staging.
Treatment options+sun avoidance.
Prognosis.
Follow up+self assessment.
Possible referral to oncologist.
Examination of family members.
Thanks.
🔴What type of reaction is Anaphylaxis ?
📍Anaphylaxis is an IgE mediated (type 1) hypersensitivity reaction that involves the release of numerous chemical mediators from the degranulation of basophils and mast cells after reexposure to a specific antigen.
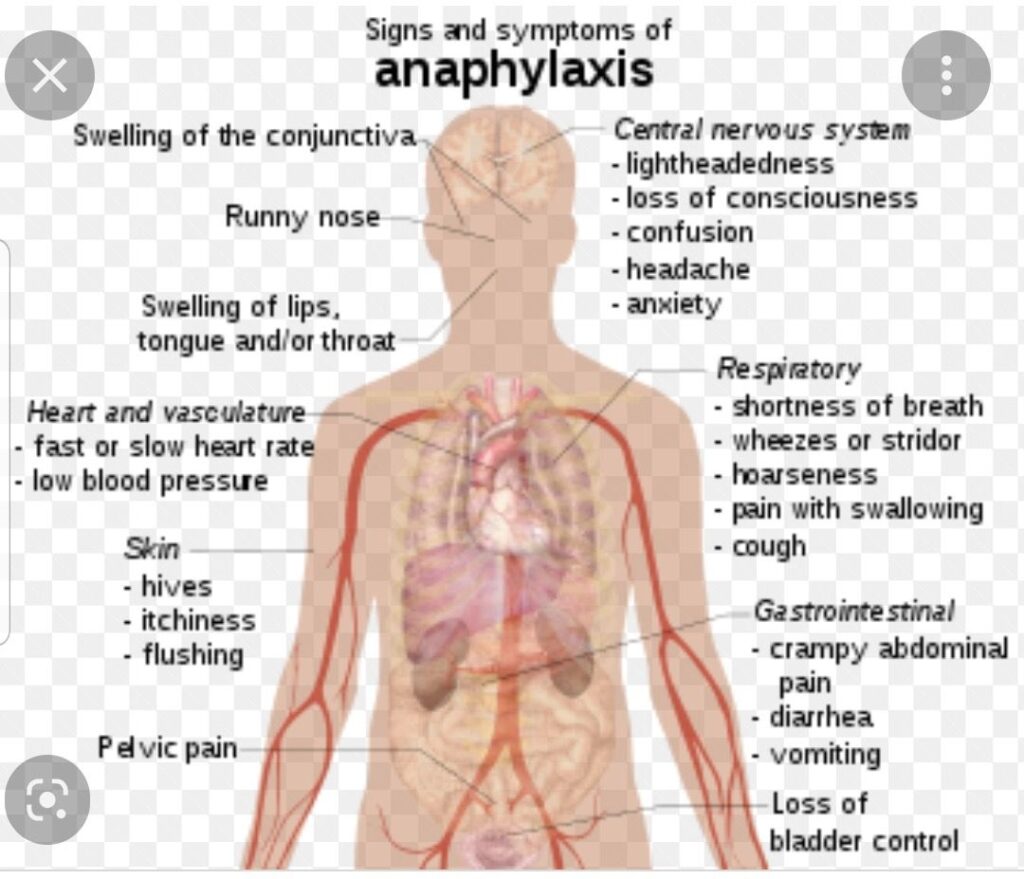
🛑Signs and symptoms of anaphylaxis ?
📍Respiratory symptoms (dyspnea, wheezing, stridor, hypoxemia, inability to maintain patency; persistent cough and/or throat clearing can be heralding symptoms)
📍Hypotension (systolic less than 90 mm Hg or a decrease of greater than 30% from baseline)
📍Signs or symptoms of end-organ dysfunction, for example, hypotonia, syncope, incontinence
📍Integumentary symptoms: Skin or mucosal layer (rash, pruritus, erythema, hives, swelling of the face, lips, tongue, or uvula).
📍Gastrointestinal symptoms: Persistent painful cramps or vomiting
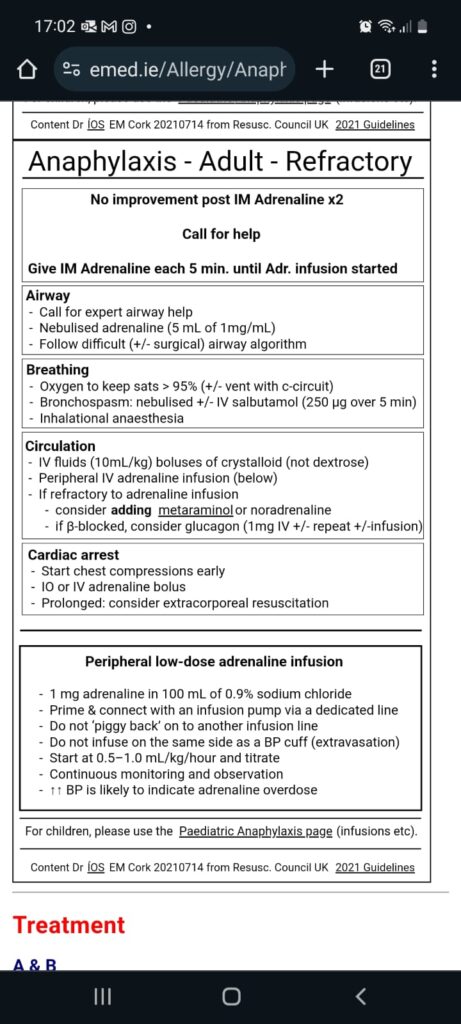
🛑Management of Anaphylaxis ?
📍Airway
Thoroughly examine the patient for airway patency or any indications of an impending loss of airway. Perioral edema, stridor, and angioedema are very high risk, and obtaining a definitive airway is imperative. Delay may reduce the chances of successful intubation as continued swelling occurs, increasing the risk for a surgical airway.
📍Decontamination
After the airway is secured, the decontamination of offending agents (if known) is the next priority to prevent continued exposure and clinical worsening.
Remove any stingers, if present.
🛑Epinephrine
Epinephrine is given through intramuscular injection and at a dose of 0.3 to 0.5 mL of 1:1,000 concentration of epinephrine. Pediatric dosing is 0.01 mg/kg or 0.15 mg intramuscularly (IM) (epinephrine injection for pediatric dosage). Intramuscular delivery has proven to provide more rapid delivery and produce better outcomes than subcutaneous or intravascular. Note if intravenous (IV) epinephrine is to be given, the concentration required is 1:10,000; see the next paragraph. The thigh is preferred to the deltoid when possible.While most patients require only a single dose, repeat doses may be given every 5 to 10 minutes as needed until symptoms improve.
📍If patients require multiple doses, a continuous infusion of epinephrine may be considered; start an initial IV infusion of 0.1 mg of 1:10,000, given over 5 to 10 minutes.
📍If more is required, begin infusion at 1 microgram per minute and titrate to effect.
📍Stop IV infusion if arrhythmia or chest pain develops. The risk of cardiovascular complications is much greater for IV epinephrine.
🛑IV Fluid Resuscitation
Anaphylaxis induces a distributive shock that typically is responsive to fluid resuscitation and the above epinephrine. One to 2 L or 10 to 20 mL/kg isotonic crystalloid bolus should be given for observed hypotension.

So you have started off with a known risk factor ‘bee sting’. However in practical life this is not the case .
Patients will land in anaphylaxis and you ll have to dig out the cause so you should know all possible triggers and rule them out one by one.
Please ‘ask not tell’ the signs symptoms of anaphylaxis like Kia alamat hui thein. Hont ankhain soj gai thein ,ask about hoarseness and dyspnea.
Should emphasize a lot to tell that it’s life threatening condition and should be avoided at all costs
Prophylaxis includes points like
JB restaurant SE Kuch khaein to khanay order krne s pehle tasalli KR len k fish ya nuts ya koi esi cheez shamil na ho jis s ye masala Hota hy (this point is mentioned in British association PIL and I have myself managed a patient with anaphylaxis after having food from restaurant)
Emergency services number is 1122 in Punjab. If your exam is in Karachi then you must know the emergency services available there.
EpiPen k use k Kuch points aur hain

🔰Paediatric anaphylaxis management

🔰 Adult anaphýlaxis management
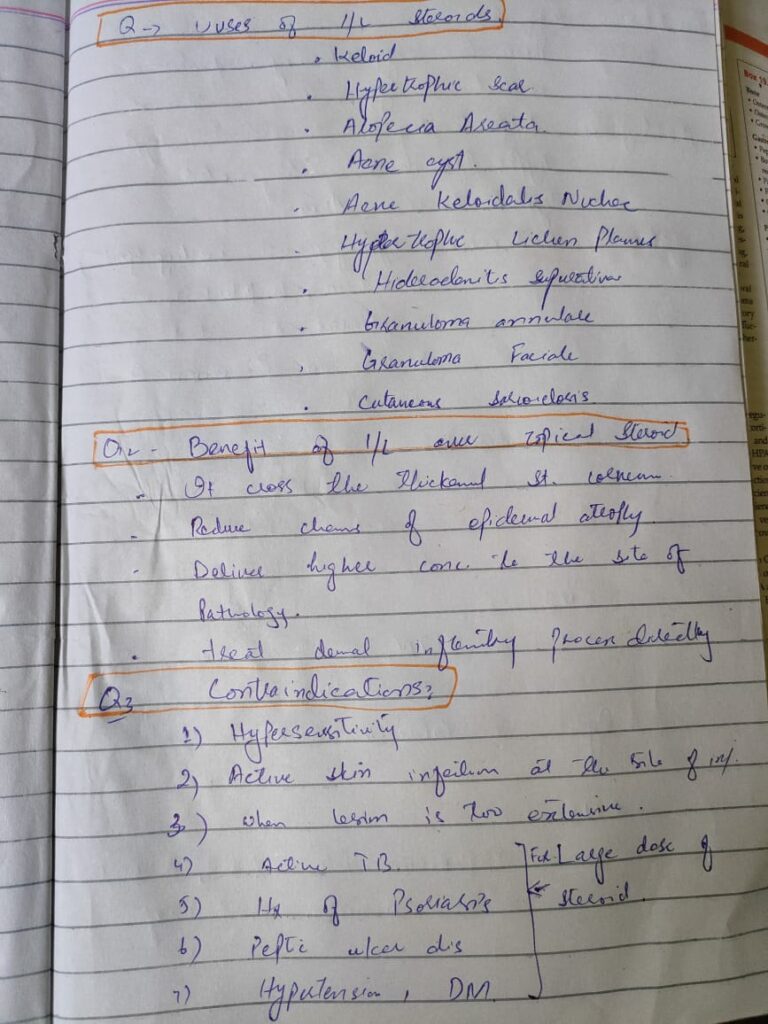
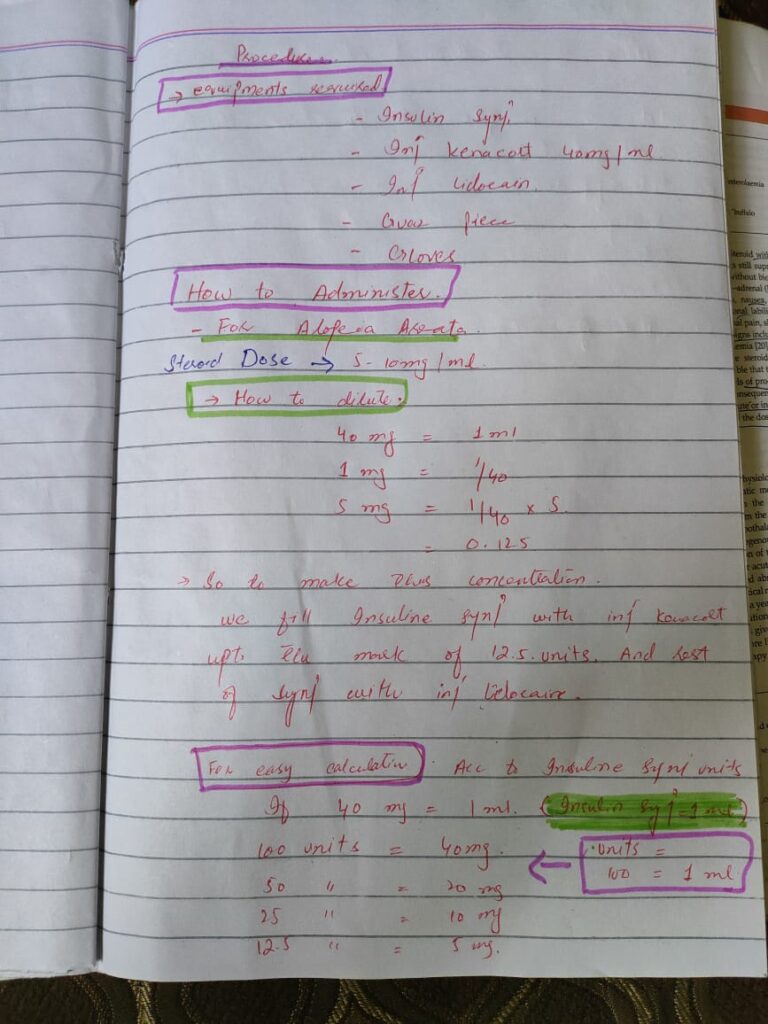
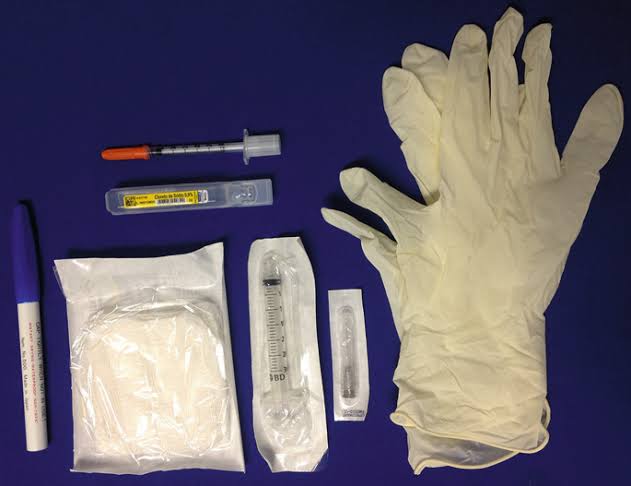
- which steroid is preferred for intralesional injection?
Ans- Steroids with low solubility should be used because of low systemic side effects. Triamcinolone acetonide, hydrocortisone acetate and Triamcinolone hexacetonide can be used . Triamcinolone acetonide is the preferred steroid because it is least atrophogenic.
2- Which diluents should be used?
Ans- Normal saline, distilled water or 1-2% lidocaine can be used. Problem with lidocaine is that it stings , so saline should be preferred.
3- how long the treatment should be continued?
Ans- treatment is repeated at 4-6 weekly intervals . It may take 2-3 months for the regrowth to be seen. But if there is no effect seen after 6 months , treatment should be stopped .
4- what should be the maximum dose of steroid given?
Ans- if we are injecting 10mg/ml concentration then dose should not exceed 2ml in one session. If we are giving 5mg/ml concentration then 4ml is the limit.
Always check/examine for any infection before injecting.
Ask for acid peptic disease, depression or psychosis.
Preparation of intralesional steroid:
Triamcinolone acetonide
10mg. And 40 mg
For scalp..5-10 mg / ml
For face….2.5- 5 mg/ ml
For 10mg/ml
10mg= 1ml
1mg= 0.1 ml
5mg= 0.1× 5= 0.5 ml
So fill halfof the insulin syringe.
For 2.5mg/ ml…fill syringe between 20 and 30 units.
For 10mg/ ml, use full syringe.
For 40mg/ ml
Take 5cc syringe
Fill 1ml steroid and 3ml distilled water to make
4ml = 40mg
1ml = 10 mg
Patient should be councelled that if there is any swelling, persistant pain and diacharge at the site of injection then he should consult the doctor.
what are the poor prognostic factors in alopecia areata?
Ans- early age of onset, extensive disease including alopecia totalis, universalis and oophiasis, family history, nail changes, duration more than 2 years , association with atopy (controversial)
Source: Rooks 89.34
As command was to give I/L steroid in 1*1cm patch. So we hv to give only one injection in this area.

🔰Important👇🏻
For 40 mg/ml in insulin syringe
1 mg is in 2.5 unit of syringe
So if you fill the syringe till 10 unit . You have 4 mg on syringe and you can dilute it to make 1 ml
12.5 unit TAC makes 5mg/ml
25 unit makes 10 mg/ml
50 unit make 20 mg/ml
METHOD OF ADMINISTRATION
🔹Introduce yourself
🔹Explain procedure, its risks, benefits, and alternatives to the patient
🔹Rule out contraindications to intralesional steroid
🔹Obtain informed consent and document it on chart
🔹Check for the necessary equipment
🔹Dilute the steroid according to required concentration
🔹Take the diluted drug in 1cc syringe with appropriate gauge of needle (according to the disease)
🔹Clean the area with alcohol swab
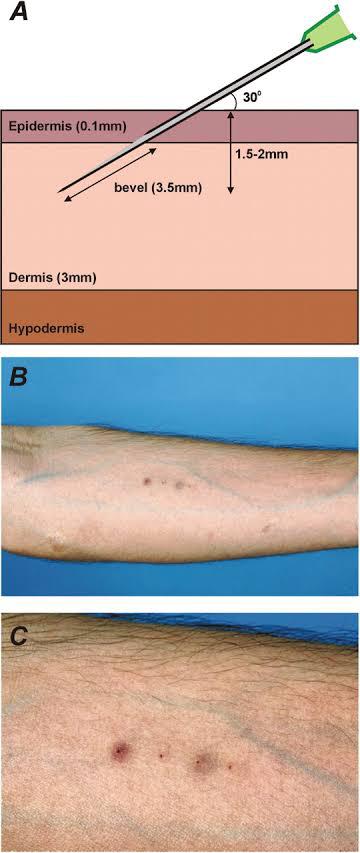
🔹Inject the drug, keep the bevelled edge of needle toward epidermis, needle is introduced at 45 angle and Drug is injected into the papillary dermis close to DEJ to raise a wheal.
🔹Multiple injections are given starting from periphery of the lesion then going to the centre with adjacent entry sites being 1 cm apart
🔹Generally, 0.1-0.2 mL is injected per square centimetre of involved skin.
🔹The total dose per sessions varies from 15 to 40mg.
🔹It can be repeated every 4-8 weeks.
🔹Pay thanks to patient.
How to formulate 5mg/ml from 10mg triamcinolone
10mg triamcinolone=1ml
1mg = 1/10= 0.1
5mg= 5×0.1 = 0.5ml
50 units of 1cc insulin syringe and add 50 units of normal saline/2% lidocaine
How to formulate 5mg/ml from 40mg triamcinolone
40mg triamcinolone=1ml
1mg = 1/40= 0.025ml
5mg= 5×0.025 = 0.12ml
(10 units of 1cc insulin syringe) and add 90 units of normal saline/2% lidocaine
♦️Enlist indications of IL steroids?
🔹KELOIDS
🔹HYPERTROPHIC SCAR
🔹ALOPECIAABEATA
🔹ACNECYSI
🔹ACNE KELOIDALIS NUCHAE
🔹HIDRADENITIS SUPPURATIVA
🔹PRURIGO NODULARIS
🔹HYPERTROPHIC LICHEN PLANUS
🔹LICHEN SIMPLEX CHRONICUS (NEURODERMATITIS)
🔹DISCOID LUPUS ERYTHEMATOSUS
🔹GRANULOMA ANNULARE
🔹CUTANEOUS SARCOIDOSIS
🔹GRANULOMA FACIALE
🔹LOCALISED THICK PSORIATIC PLAQUE
🔹NECROBIOSIS LIPOIDICA
🔹NODULOCYSTIC ACNE
🔹INFANTILE HAEMANGIOMAS
♦️ What are contraindications of IL steroids?
🔹Known hypersensitivity to triamcinolone
🔹Avoid at the site of active skin infection
🔹When lesions are too extensive
🔹Active tuberculosis or systemic fungal infection
🔹Extensive plaque psoriasis, pustular psoriasis,or erythrodermic psoriasis
🔹Active peptic ulcer disease
🔹Uncontrolled diabetes, heart failure, or severe hypertension
🔹Severe depression or psychosis
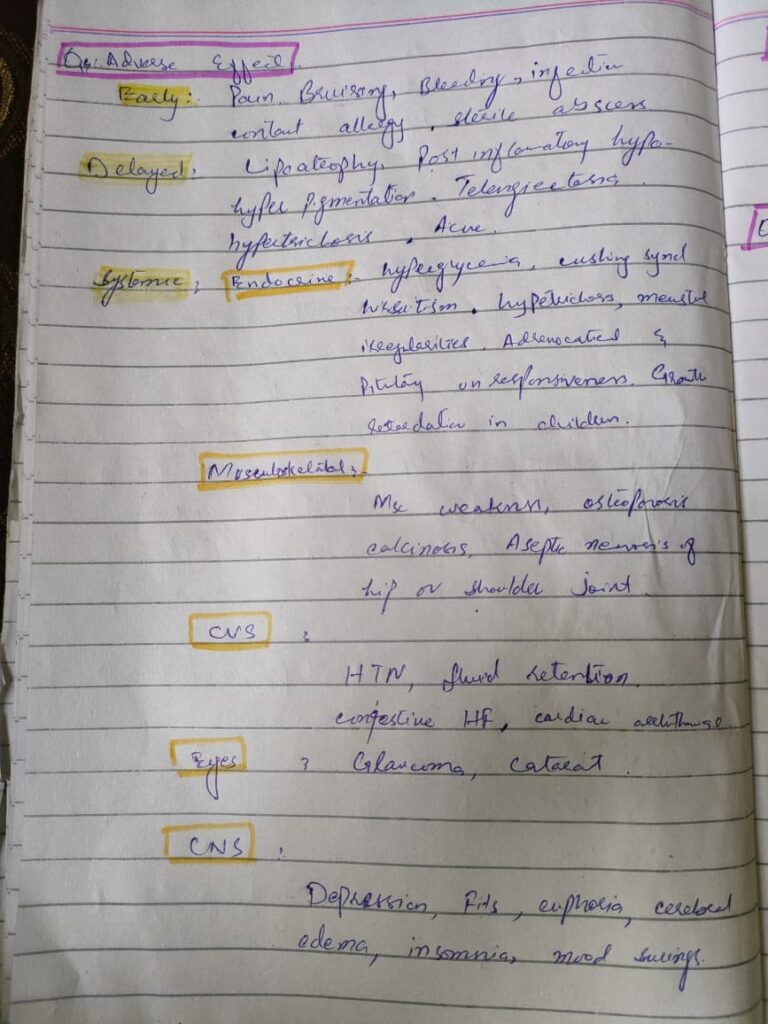
♦️Enlist few side effects ?
🔹Pain
🔹Bruising
🔹Bleeding
🔹Infection
🔹Contact allergic dermatitis
🔹Impaired wound healing
🔹Sterile abscess
🔹Lipoatrophy
🔹Postinflammatory hypo or hyperpigmentation
🔹Telangiectasia
🔹Localised hypertrichosis
🔹Localised or distant steroid acne
♦️What is its dosage ?
🔹40 mg/ml for thick keloid scar
🔹10 mg/ml for a moderate thickness hypertrophic scar
annulare,
🔹10 mg/ml into discoid lupus erythematosus or granuloma annulare
🔹5 mg/ml into the skin of normal thickness associated with alopecia areata
🔹2mg/ml for acne cyst
♦️What are recommendations for Alopecia areata?
🔹It is recommended using 5-10mg/ml of triamcinolone for the scalp,
2.5-5mg eyebrows and the beard.
🔹Treatment is repeated every 4 to 6 weeks, and the total amount injected per session varies from 15-40 mg.
🔹An initial response is after 4-8 weeks.
🔹If regrowth can not be seen after 4 months of treatment, other treatment options should be considered
✍🏻Triamcinolone acetonide is the preferred intralesional product because it is less atrophogenic than triamcinolone hexacetonide✍🏻ILCs preferably triamcinolone acetonide is the first-line therapy for adult patients with less than 50% of scalp involvement.[2,4,12] Concentrations of 2.5 to 10 mg/mL may be used, but 5 mg/mL (maximum volume of 3 mL per session) is the preferred concentration for scalp.[2–4,12] For the eyebrows and face, 2.5 mg/mL can be used (0.5 mL to each eyebrow).[12] A concentration of 10 mg/mL with a maximum total of 2 mL, or 5 mg/mL for a maximum total of 4 mL, has also been reported for use on the scalp, at one visit✍🏻✍🏻Triamicinolone acetinoide is injected intradermally with a 0.5-inch long, 30-gauge needle, as multiple 0.1-mL injections at 1-cm intervals.✍🏻Sterile saline is preferred over Xylocaine as a dilutent, because the latter stings more✍🏻Optional topical anesthetic can be applied 30Optional topical anesthetic can be applied 30 to 60 minutes before treatment to minimize pain from the injections, this will be useful when treating eyebrows.
✍🏻other treatment options for alopecia areata should be known too
https://pmc.ncbi.nlm.nih.gov/articles/PMC3002419/
-total of 50 to 100units of botox can be used on each palm.
-photographs should be taken before and after.
Mechanism of action
Cleaves a protein SNAP25 and thus blocks the release of acetylcholine at NMJ causing flaccid paralysis.
*Cumulative dose 360 units in 3months
Side effects
-pain
-burning
-bruising
-hand weakness
-muscle weakness
Duration of onset : after 2 weeks but stays for 3 to 4 months
Storage 2 to 8°c
I vial =100units
-For best result, use within4hours of reconstitution.
Contraindication
Avoid concomitant use with
– antimalarial
– d penicillamine
– aminoglycosides
– cyclosporine
– oral zinc

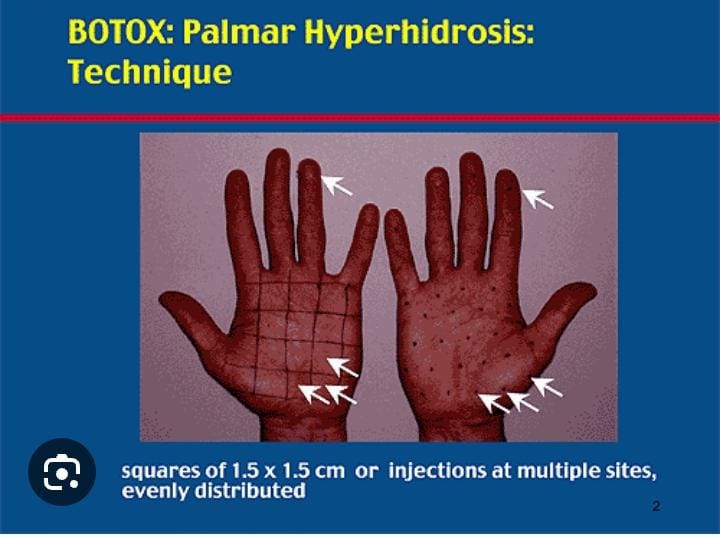
Rule out all contraindications for Botox
Examiner may ask k kitne pese lagein ge and when do you repeat the procedure.
Palmar hyperhidrosis can be particularly distressing and embarrassing for the patients
I have had a patient who was about to drop a grenade because of the sweat in his hands and had a narrow escape 😯
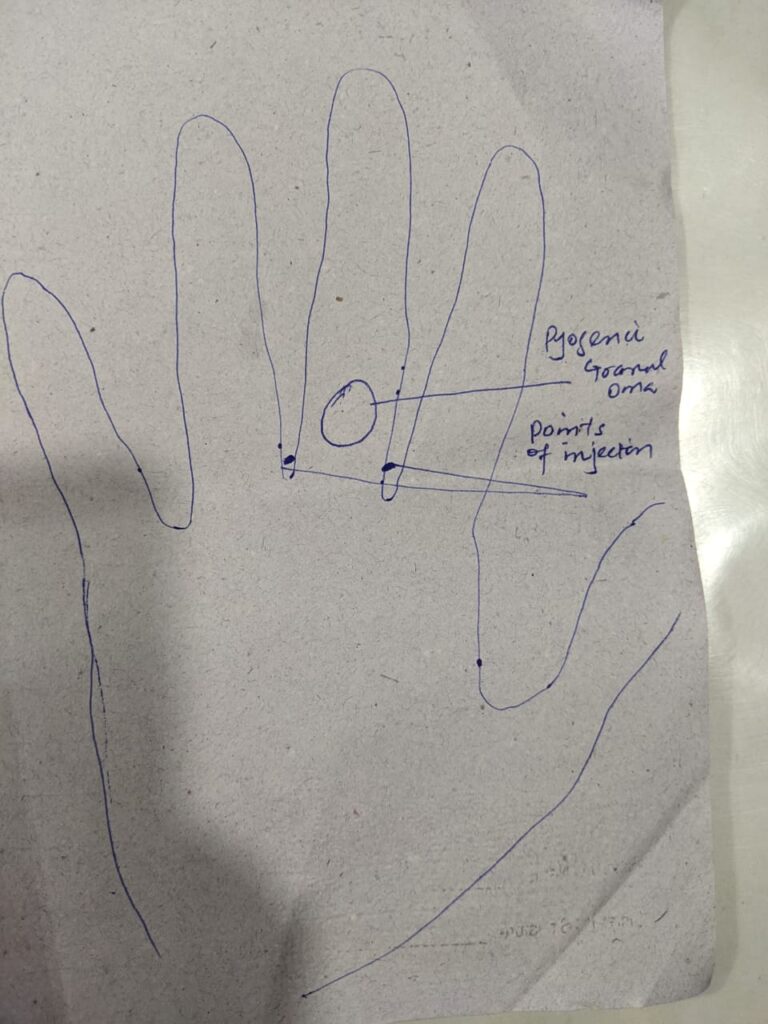
🌓A 55 years old man presented with 6 months history of broad linear black to brown discolouration of right thumb nail plate with extension beyond proximal nail fold .You have decided to do nail biopsy under digital block to confirm diagnosis of melanoma.
Distal Digital Block
🌓Preliminary steps
🌓Introduction
🌓To rule out contraindication
🌓Explanation of procedure and
Side effects
🌓Consent
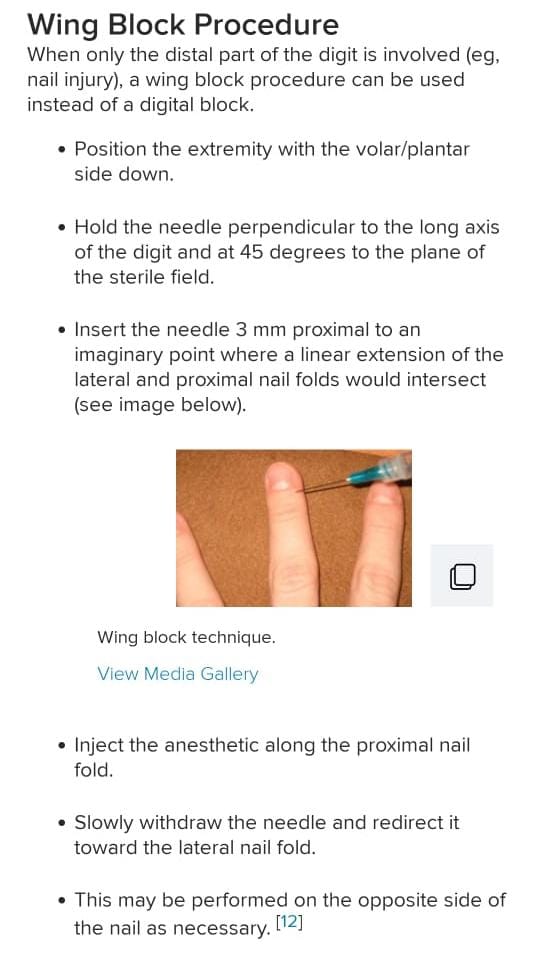
Technique
🌗 Injection site :
“1cm” proximal and lateral to the junction of the proximal nail fold and the lateral nail fold
🌓 Angle of Needle insertion:
“45°”
🌓 Amount of anaesthetic agent
“0.5ml ” each for dorsal and palmar nerves.
🌓Direction of Injection
🌓 For dorsal nerve :
Push distally down to the bone
🌓 For palmar nerve :
Partially withdrawn and pushed down vertically towards the finger pulp
🌓 For full anaesthesia: Repeat the procedure on the opposite side of digit
🌓 Pay Thanks guide about follow up and Monitoring for side effects
https://youtu.be/f_YihInlmrI?si=JF98_C_sRr8RySSh
Questions with Answers
🌓 What measures can be taken to minimize patient discomfort during providing aneasthesia?
1:Slow injection
2:Small needle size
3:Small amount of anaesthetic agent
4:Prior alkalinization or warming at 37°c of anaesthetic agent.
🌓What conditions are unsafe to combine epinephrine with lignocaine for digital block?
1.Vasospasm
2.Thrombosis
3.Severe medical conditions
🌓 What are different approaches of digital block?
1.Webspace block
2.Transthecal /flexor tendon sheath block
3.Ring block
- Three sided digital block
5.Wing block
🌓Which approach is most effective for great toe anaesthesia ?
3 sided block
🌓What are the benefits of adding bupivacaine to lidocaine?
1.lengthens the postoperative analgesia
2.Acts as volumetric tourniquet to prevent bleeding .
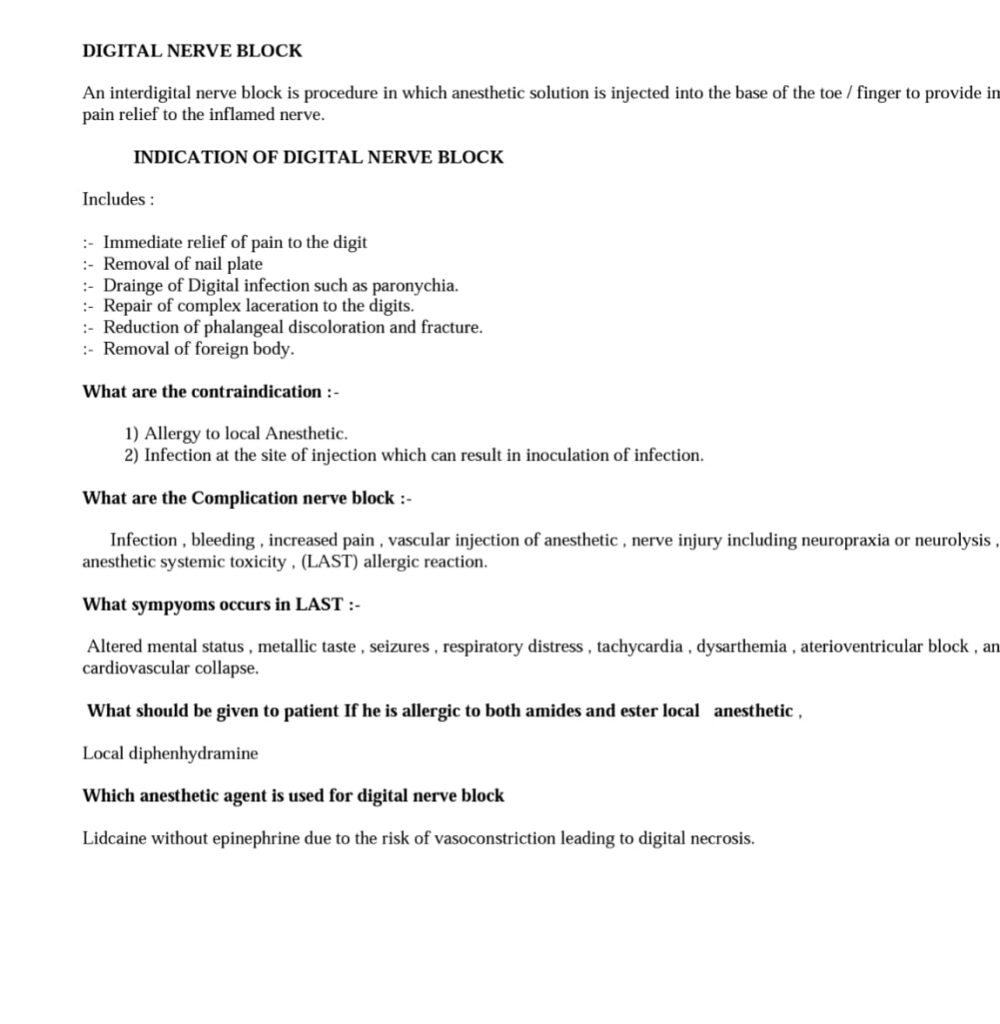
♦️Digital blocks is a simple procedure that provides immediate anesthesia indicated for any minor surgery or procedure of the digits.
These include:
💉Large irregular lacerations.
💉Lacerations involving the nail or the nail bed
💉Ingrown nails
💉Felon or paronychia
💉Trephination of subungual hematoma
💉Digit dislocations or fractures
♦️Absolute contraindications:
-allergy to local anesthetics.
-infection at the injection site
-compromised circulation in the digit.
♦️Relative contraindications
-coagulopathy
-systemic infections.
♦️Complications:
-infection
-hematoma
-nerve injury
-allergic reactions.
-avoid epinephrine in the local anesthetic to prevent ischemia.
The names of ester ( procaine, tetracaine, cocaine)
amides ( lidocaine, mepivacaine, bupivacaine, prilocaine).
The difference between onset of action of various anesthetics and the duration of action with epinephrine (average 180 mins) and without epinephrine (average 90mins) should be known.
Anesthetics safe in pregnancy include bupivacaine and chloroprocaine.
👉 Also ask for raynaud, pain, and prior history of discoloration of fingers
👉 Take informed consent in written form before performing
👉 Use 27 guage needle to minimize pain , 2 percent lignocine shoud be used without adrenaline.


🔰 Important tip👇🏻
For toacs mainly focus on procedure and performance.
Watch as many videos as possible coz in the end they mostly do the markings on how u perform
Most commonly they ask can you use local anaesthetic with epinephrine here
Aspiration is important
Viva will be mainly on lignocain toxicity.
https://youtu.be/nhL0Y_xOJI8?si=4XYce3xMJPw5aLF8
💡bp cuff need to be wrapped 2-3 cm above antecubital fossa crease


https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10102405/

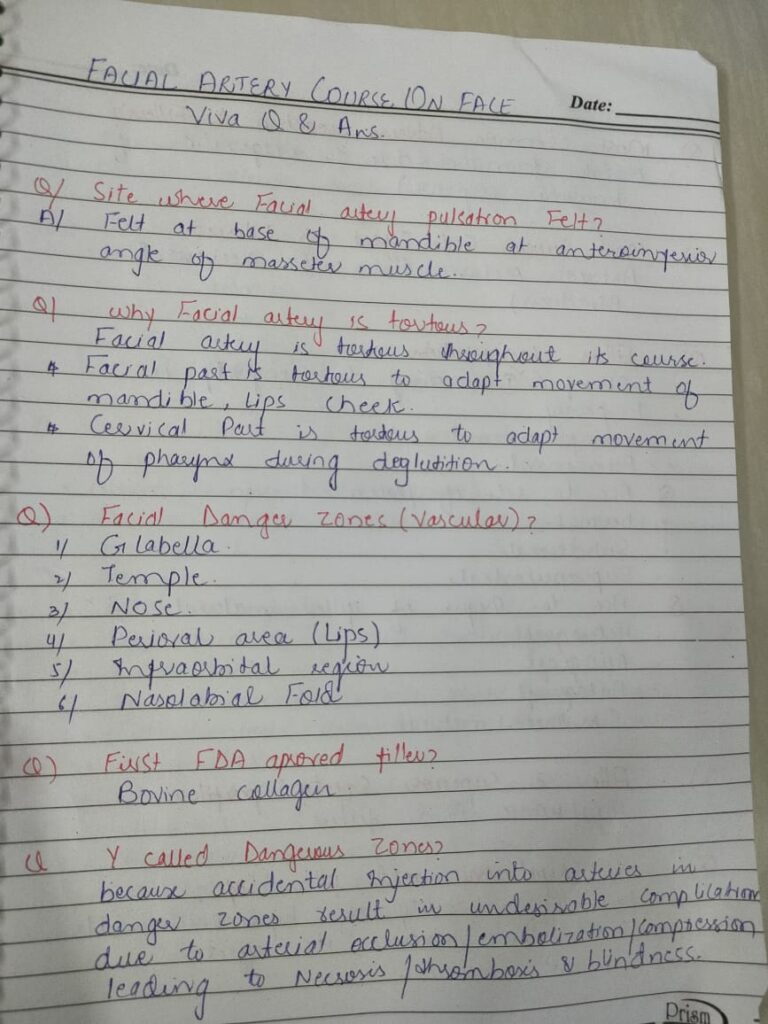
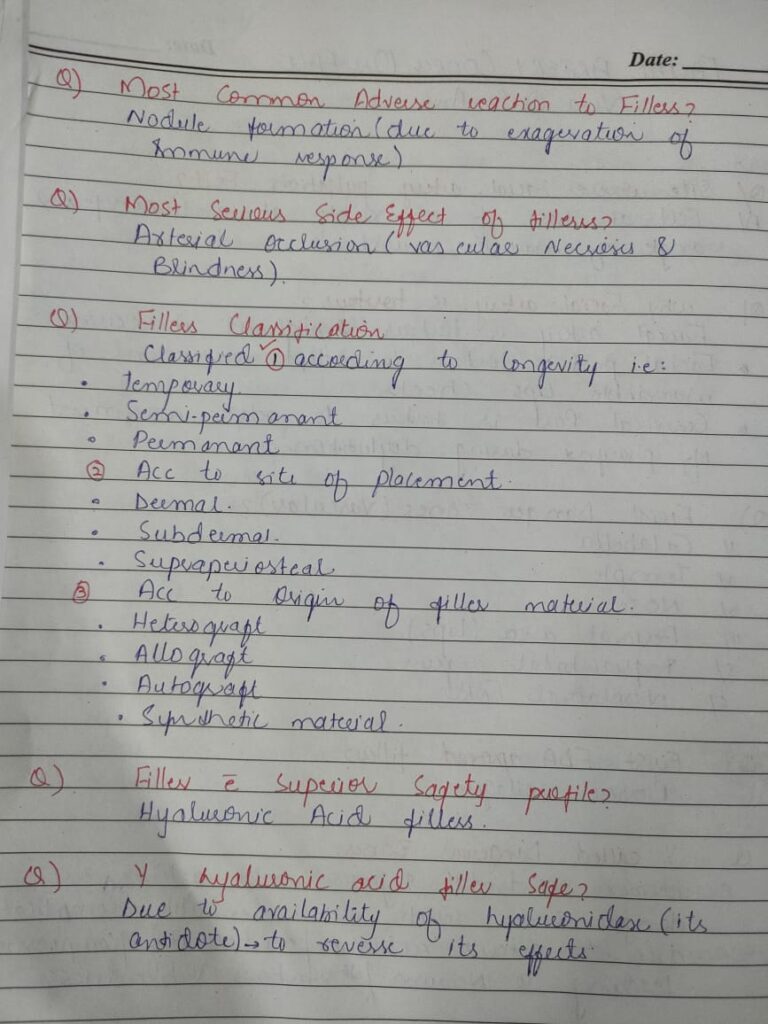
What are marionette lines?
lines that originate at the corners of the mouth and can continue down to the chin and jaw line. These lines can cause the corners of the mouth to droop and make patients look sad and/or angry.
Name the First FDA approved filler?
Bovine collagen
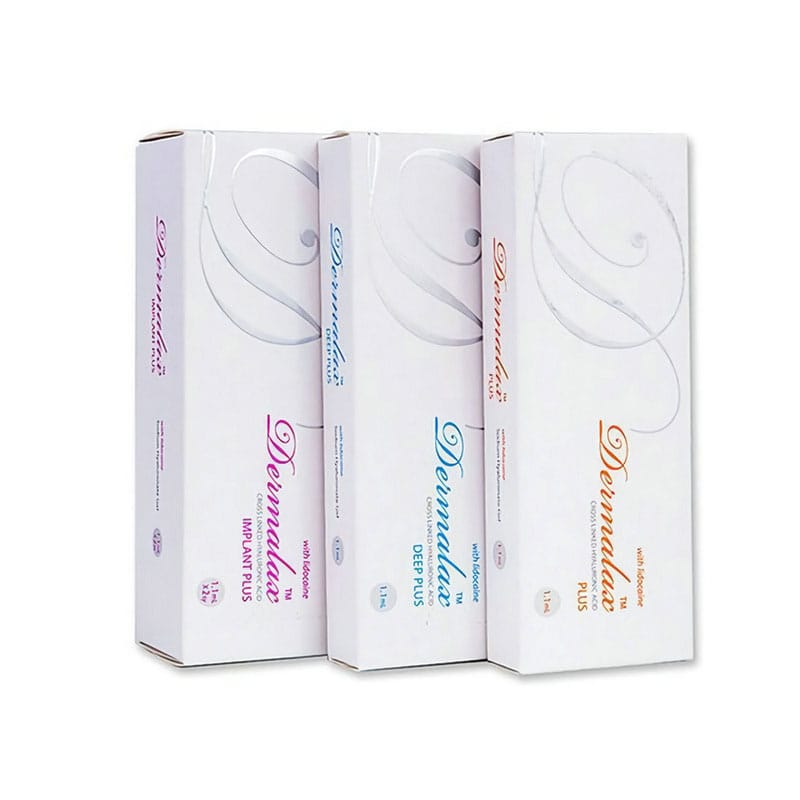
How will u classify fillers?
Fillers can be classify
acc to longevity
(temporary, semi permanent nd permanent )
Acc to site of placement
(dermal ,subdermal,supraperiosetal )
Acc to origin of filler material
(hetrograft,allograft,autograft,synthetic material)
What is the most common adverse reaction to fillers?
Nodule formation (due to exaggeration of immune response)
what is the most serious side effect of fillers
Arterial occlusion either due to direct embolization or due to external compression.
Why Hyaluronic acid fillers have superior safety profile as compared to non-HA fillers?
Due to ability to reverse effects with use of hyaluronidase
Which fillers require intradermt Pretesting?
Bovine collagen
What are the side effects of hyaluronidase
Pain,pruritis, Erythema,edema immediate and delayed allergic reaction.
what are the tell-tale signs of venous occulsion?
* Skin blanching
*Dusky (i.e., grayish blue) skin
* Ecchymosis
* Reticulated erythema
*Intense pain in the treated area
What are marionette lines?
lines that originate at the corners of the mouth and can continue down to the chin and jaw line. These lines can cause the corners of the mouth to droop and make patients look sad and/or angry.
Name the First FDA approved filler?
Bovine collagen
How will u classify fillers?
Fillers can be classify
acc to longevity
(temporary, semi permanent nd permanent )
Acc to site of placement
(dermal ,subdermal,supraperiosetal )
Acc to origin of filler material
(hetrograft,allograft,autograft,synthetic material)
What is the most common adverse reaction to fillers?
Nodule formation (due to exaggeration of immune response)
what is the most serious side effect of fillers
Arterial occlusion either due to direct embolization or due to external compression.
Why Hyaluronic acid fillers have superior safety profile as compared to non-HA fillers?
Due to ability to reverse effects with use of hyaluronidase
Which fillers require intradermt Pretesting?
Bovine collagen
What are the side effects of hyaluronidase
Pain,pruritis, Erythema,edema immediate and delayed allergic reaction.
what are the tell-tale signs of venous occulsion?
* Skin blanching
*Dusky (i.e., grayish blue) skin
* Ecchymosis
* Reticulated erythema
*Intense pain in the treated area
WHAT TO DO IN THE EVENT OF ARTERIAL/VENOUS OCCLUSION AND IMPENDING NECROSIS ?
* Warm compresses immediately
* Massage othe area to facilitate vasodilation and dispersion of material
* Aspirin
* Topical nitro paste
* Hyaluronidase (if using HA)
* Corticosteroids
* If ischemia is not reversed and necrosis is unresponsive, contact a plastic or reconstructive surgeon
*Subcutaneous injections of low-molecular-weight heparin may be helpful
* Antibiotics
* Antivirals (if impending necrosis is around the mouth)
* Hyperbaric oxygen for 1 month
*Multiple laser treatments at 3-month postinjection intervals may be necessary
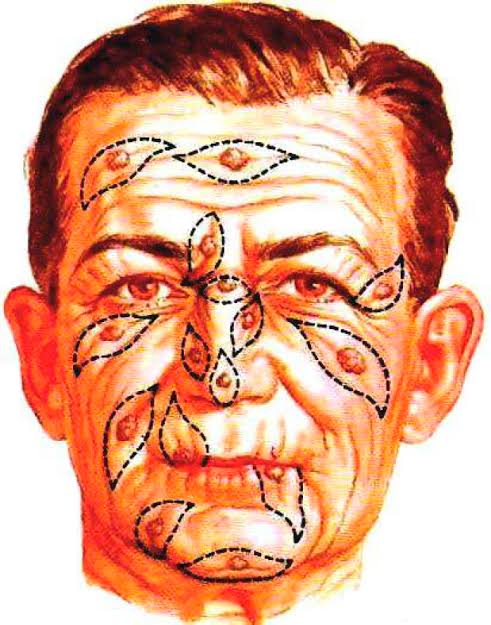
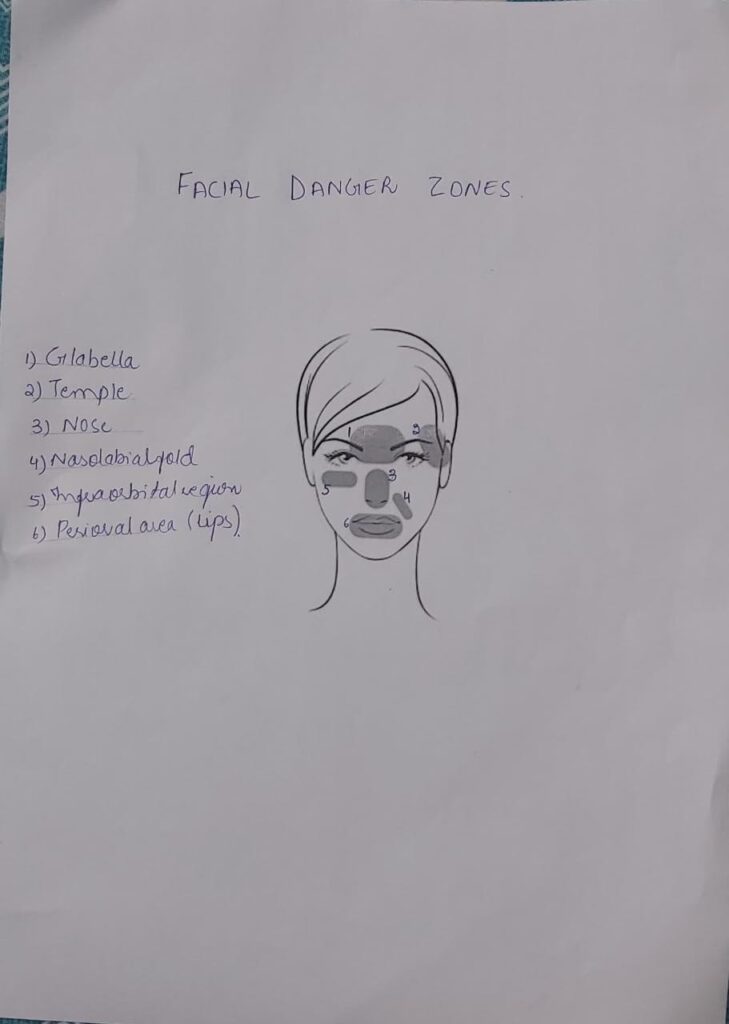
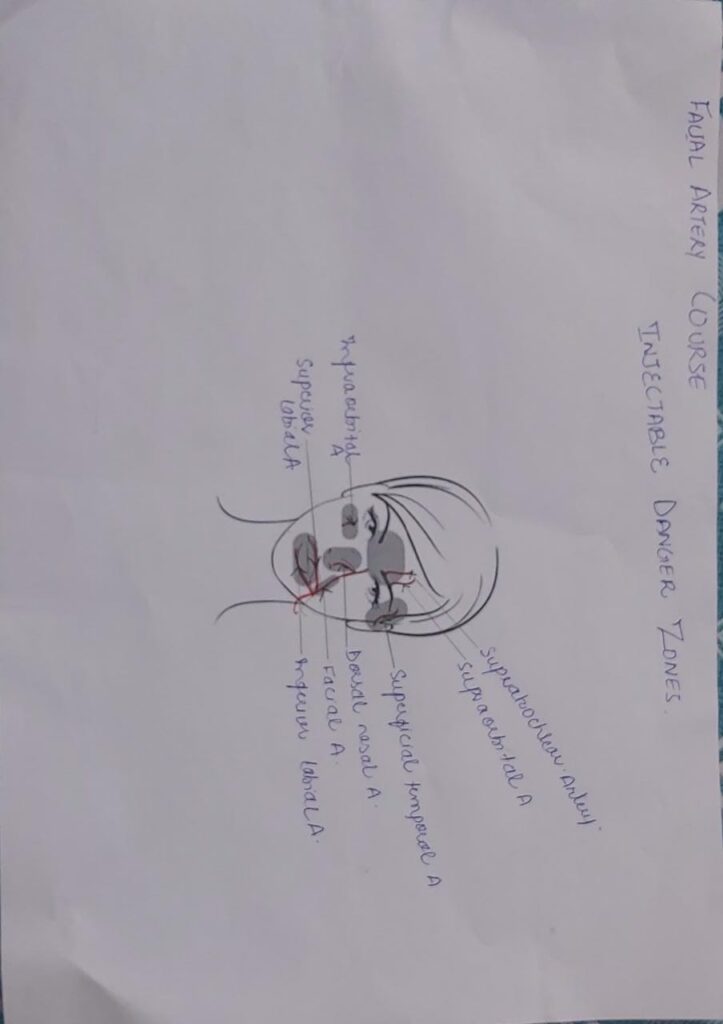
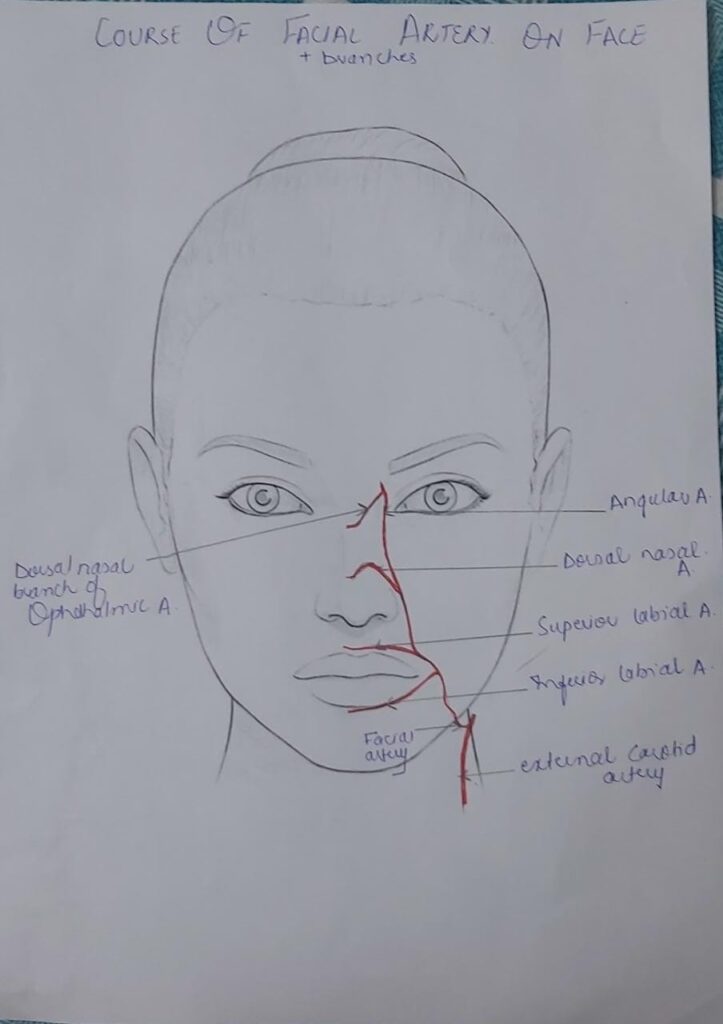
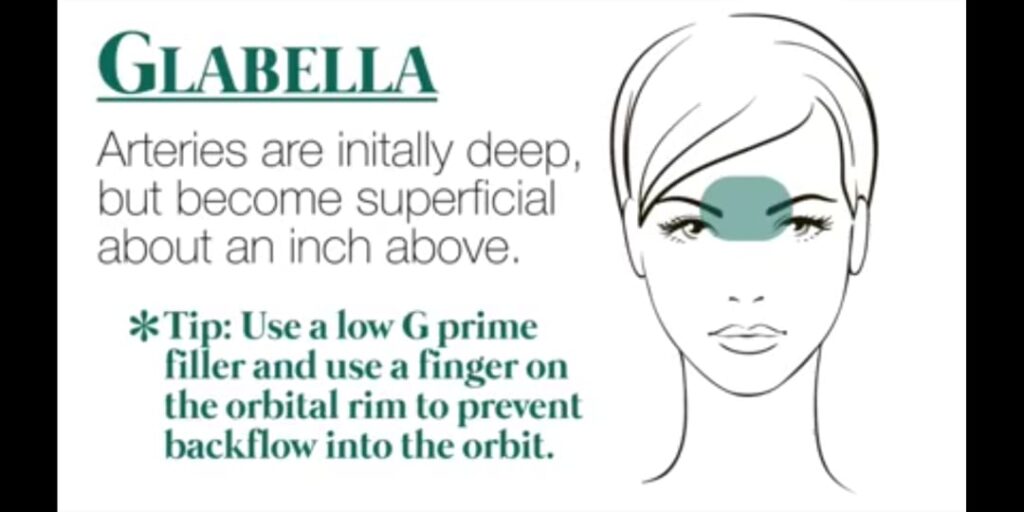
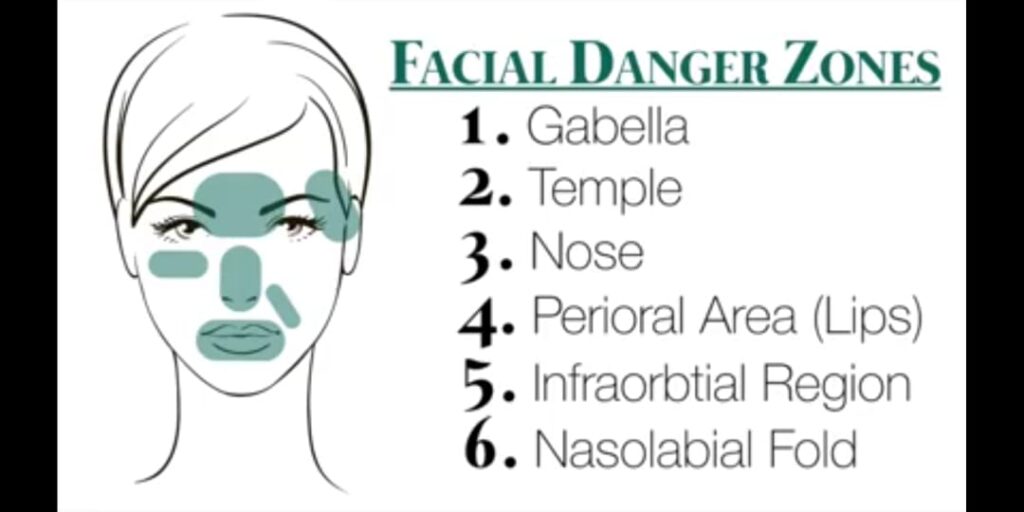
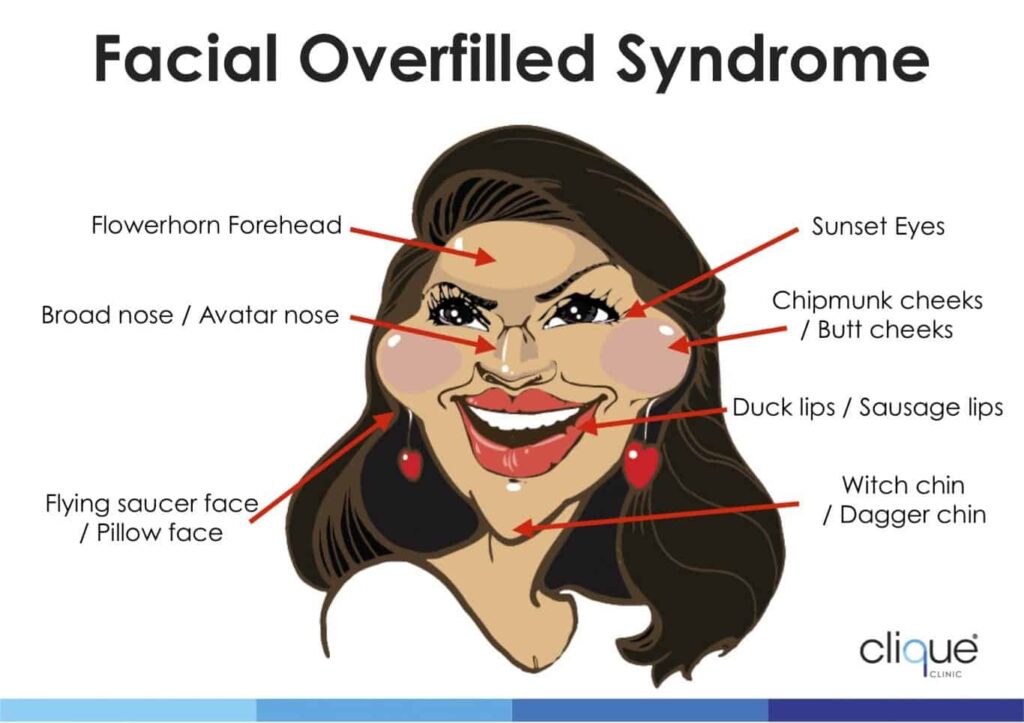
Danger Zones on the Face
🔴1st… Supraorbital and supratrochlear arteries in Glabella
Tips to avoid…
🔹avoid 1 finger breadth from the medial canthus
🔹occlude the arteries during injection
🔴2nd.. medial canthus
🔹 Anastomosis b/w ophthalmic branch of internal carotid artery and the angular artery
🔹 Anastomosis b/w the angular artery and the dorsal nasal artery
Tips to avoid
🔹 Avoid 1 finger breadth from the medial canthus
🔹Approach from inferior direction and go deeper because vessels are superficial
🔴3rd.. Nasolabial fold and the nasal alar groove
Tips to avoid…
🔹 Completely avoid 1 finger breadth posterior to the nasal alar and inject perpendicularly to the vessel.. The nasal ala is a NO-GO ZONE
🔴4th… Lips/Oral commissure
Tips to avoid…
🔹Give injection within 1 finger breadth amd superficial
🔴5th… Mandible and jaw
🔹Facial artery enters the face at the mandibular notch anterior inferior portion of the masseter muscle
Tips to avoid..
🔹Inject perpendicular to the vessel.parallel to the base of the mandible, aspirate and use vessel mapping
🔴6th.. Anterior medial length of Ear
Tips to avoid..
🔹Avoid 1 finger breadth the entire length of the anterior border of the ear from the base of mandible to superior temporal fossa
🔴7th… Temporal fossa
Superficial temporal artery and middle temporal vein
Tips to avoid..
🔹Inject 1 finger breadth above the superior border of zygomatic arch with your finger posterior to the tail of eyebrow to avoid the middle temporal vein
🔴What are the symptoms associated with impending necrosis?
🔹Skin balanching
🔹Dusky( greyish blue) skin
🔹Echymosis
🔹Reticulated erythema
🔹Intense pain in the treated area
🔴What are the symptoms associated with impending vision loss?
🔹Occular pain in the affected eye immediately after the injection
🔹Diminished vision
🔹Headache
🔹Dizziness
🔹Ptosis
🔹 Ophthalmoplegia
🔴What will you do in the event of arterial/ venous occlusion and impending necrosis?
🔹Warm compresses immediately
🔹No ice
🔹 Massage the area to facilitate vasodilation and dispersion of material
🔹Topical nitro paste (vasodilator)
🔹Hyaluronidase (only if using HA)
🔹Corticosteroids (anti-infl ammatory/immunomodulator
🔹If ischemia is not reversed and necrosis is unresponsive, contact a plastic or reconstructive
surgeon—subcutaneous injections of low molecular-weight heparin may be helpful
🔹Antibiotics
🔹Antivirals (if impending necrosis is around the
mouth)
🔹Hyperbaric oxygen for 1 month may be required
🔹Multiple laser treatments at 3-month postinjection
intervals may be necessary
🔴What to do in the event of impending visual loss
🔹The best strategy for prevention is avoiding the
“danger zones” especially in the glabellar, forehead, and
upper nasal labial fold areas
🔹If vision loss is suspected
the client must make an emergency visit to an ophthalmologist
🔹Maintain area as if vascular compromise is the issue until an ophthalmologist is available
🔴Practical tips when injecting near danger zones?
🔹Aspirate before injecting
🔹Inject in a retrograde fashion
🔹Inject small aliquots of filler/volumizer at a time.. a
good rate to consider is less than 0.3 ml/min
🔹Avoid using anesthesia near a vascular bundle that may induce vascular spasm, such as those containing epinephrine, also avoid using epinephrine so that the cause of blanching can be determined quickly
🔹Use the smallest gauge needle possible to slow
the flow of product
🔹Pinch/tent the skin to provide more space between superficial branches of main arteries and
to move away from underlying vasculature
🔹Use a reversible product for example in case of HA… hyaluronidase will quickly break down HA fillers
🔹Manually occlude the origin of important vessels with the nondominant finger
🔹If using a nonreversible product (e.g. calcium
hydroxylapatite, poly- L-lactic acid, and polymethyl
methacrylate)use smaller aliquots of nonreversible product, and the viscosity can be lowered by
premixing with lidocaine solution or extruding through a small-gauge needle
🔹Inject in a more medial and superficial plane
🔹Assess pain during the injection
🔹Keep a watchful eye on the area of injection (i.e.
look for blanching

Paradoxical emboli for fillers👇🏻
Chk capillary refill first
Hyalurunidase
1500 units dilute in 5ml
Inject 500 to 1500 units for reversal every 45 mins untill reversal
Immediately warm compress
Oral aspirin
Iv antibiotic bolus and then continue for 3 to 5 days
LMWH
Iv steroid
1 3rd of the cannula shud be injected at the site of inj
Midway btw mid pupillary line and lateral canthus of eye
Depth of filler


🔰 Above given material is more than enough for this toacs station. Is se bahar in sha Allah kuch b nai puchainge
🔰 IMPORTANT👇🏻
Here are few files of clinical slides
They have the keys with them which can be seen with the right format.
Viva questions
Occipital block
*Course of Occipital Nerve*
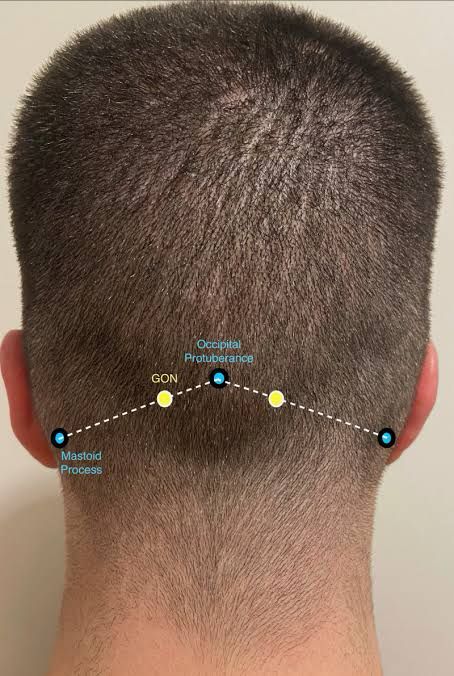
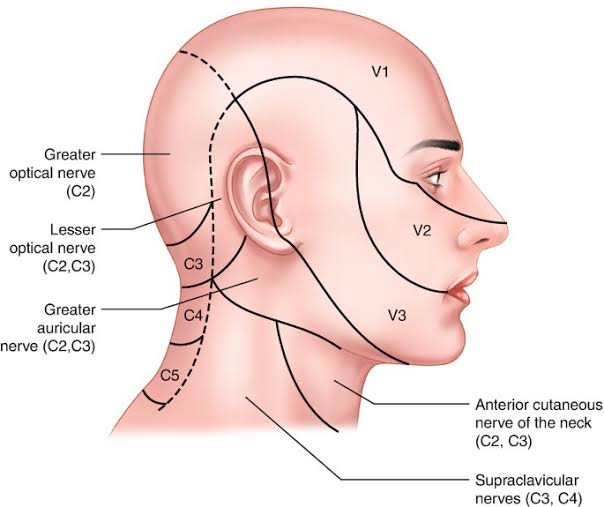
✅The greater occipital nerve: this originates from the posterior ramus of the spinal nerve, C2. It pierces the fascia under the superior nuchal ridge and emerges on the superior nuchal line along with the occipital artery. It can be located about one-third of the dis- tance along a line drawn from the occipital protuberance to the mastoid process.
✅The lesser occipital nerve: this arises from the sec- ond and third cervical nerves. It courses superiorly at the posterior region of the sternocleidomastoid
✅Indications of Occipital nerve block?
– Cervicogenic headache
– Occipital headache
– Anesthesia for posterior scalp procedure
✅Contraindications of occipital nerve block?
– Posterior fossa intracranial surgery
– Recent trauma
– Allergy to lidocaine/Bupivacaine
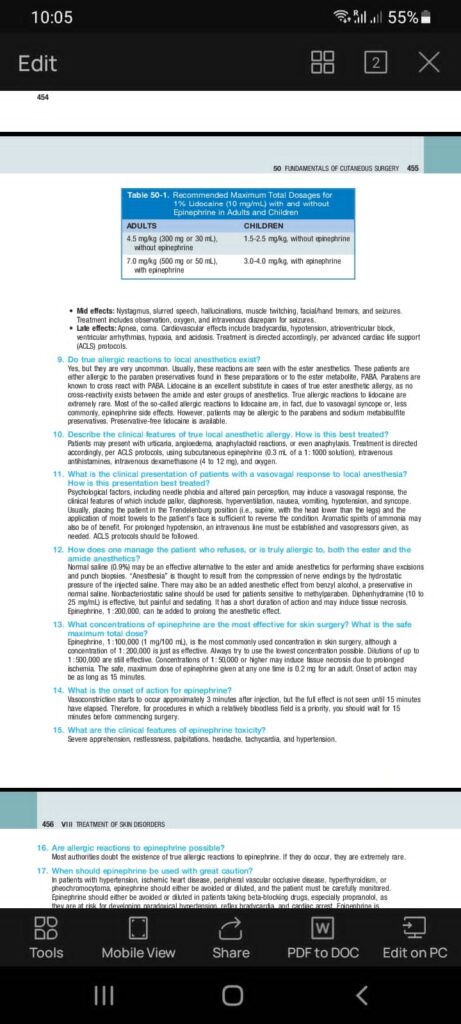
✅what is the safe dose of lidocaine for an individual?
Ans: adult=4.5mg/kg plain…7mg/kg mixed with adrenaline
Paediatric and old age dose is half the adult dose.
✅what are 2 groups of local anesthetic?
ester and amide
✅which one is better?
Amide,lesser side effects and hypersensitivity
✅What is absolute contraindication to local anesthesia
history of hypersensitivity reaction or local infection at the site of infection
✅What is lidocaine toxicity?
Early: diplopia,tinnitus, lightheadedness, nausea, circumoral pallor, vomiting
mid: slurred speech, muscle twitching, tremors, seizures
late: apnea, coma, bradycardia, AV block, hypotension, arrythmia, hypoxia
✅How do u treat?
Early: recognize and observe
Mid: observe, oxygen, diazepam for seizures
Late: ACLS protocol
✅Alternative to local anesthetic?
normal saline or 10-25 mg/ml diphenhydramine
🔶Needle size gauge can be asked in exam too 23 to 25 gauge needle used mostly for occiptal nerve block
🔶Amount of anesthesia per nerve should be known 2 to 4cc can be given
🔶Direction of needle should be known ..
It should be perpendicular to skull
🔶Post procedure care should be told as it is important
▪️After procedure patient should stay in procedure room for 20 to 30 min
▪️Its better not to drive home by himself as dizziness can occur
▪️Should not rub treated are or apply any irritant oil etc to treated area.
you all should have fine knowledge about landmarks and how to draw a line and points of nerve block


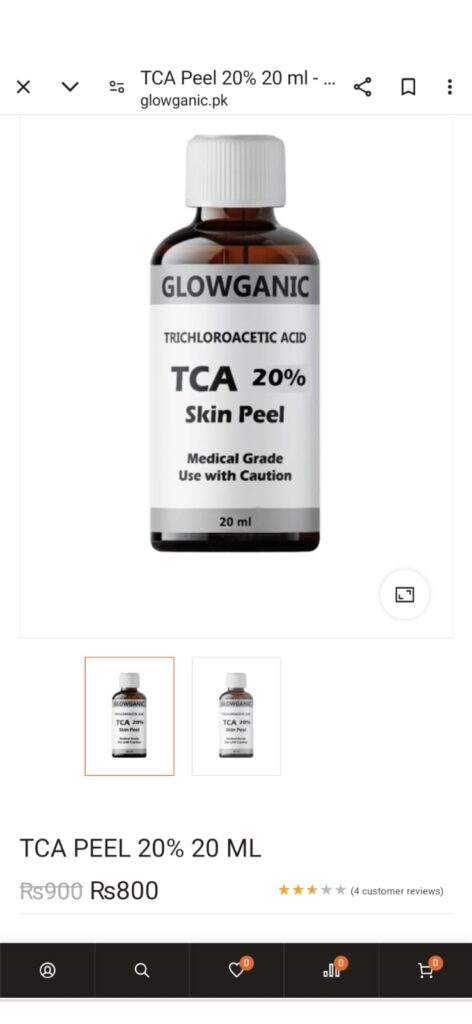
🔥Procedure
🔅Clean the area using alcohol swab
🔅Apply Vaseline around the lesion
🔅Dip cotton tip applicator in tca solution and dap to remove extra solution
🔅Aplly gently on the lesion in circular pattern from inward out
🔅Wait for white frosting to appear
🔅Wash face
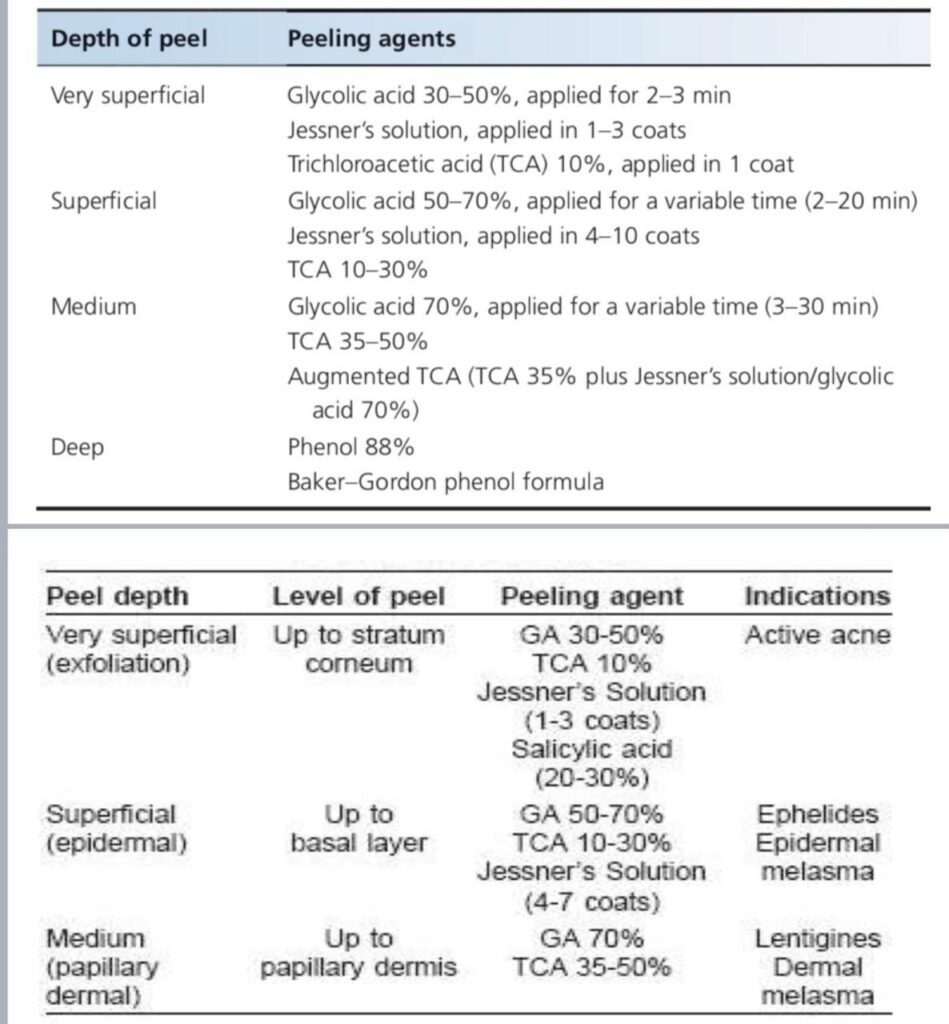
🔥Most common peels used
🔅Glycolic acid peel 20 to 70 percent
🔅TCA peel
🔅Jessners peel
🔥Composition of Jessners peel
🔅14% lactic acid,14% salicylic acid , 14% resorcinol in ethanol
🔥Which peel requires neutralization with water or weak buffer..
🔅 Glycolic acid peels ..
🔥 Mechanism of action of tca peel
🔅TCA is a caustic which causes coagulation of proteins and necrosis of tissue. The depth depends upon the concentration
of TCA used, hence has a predictable result.
🔅Necrosis of pigmented layer also occurs which is reepithelialized with normal
epithelium.
🔥what is skin priming FOR PEELS
Done for 2-4 wks before peeling for uniform penetration of peel,shortening of wound healing time and to reduce PIHP
🔅Materials used for priming
Topical retinoids
..stopped 1 to 2 days before peel n resume postpeel
🔅If peeling is for pigmentation stop 1 to 2 weeks before peel
🔥Complications of peel
🔅Erythema ..fades over a week
🔅Infections
🔅Chemical burns
🔅Premature peeling
🔅Milias
🔅Acneform eruption
🔅Allergic contact dermatitis ..to resorcinol in Jessners peel
🔅Systemic toxicity ..phenol cardiotoxic
🔅PIHP
🔥Post peel care:
🔅For MDCP, bland emolient dabbed not rubbed.
🔅No picking, rubbing and scratching.
🔅Acetic acid compress for exudative areas along with antibiotic ointment
🔅re epithelization in 5-7 days
🔅strict sun avoidance for 14 days
🔥 Contraindication of peeling:
🔅hypersensitivity to peel
🔅working outdoor
🔅keloidal tendency
🔅active herpes labialis
🔅pregnancy and lactation
🔅immunosuppresion





A young lady is sitting infront of you .she is known case of Systemic sclerosis. You are supposed to calculate Modified Rodnan score.
The thickening of skin on upper arms anterior chest abdomen back thighs and legs are same ie mild thickening.
🔰 Scores are an imp part of toacs.
Practice all scores mentioned in khurram shahzad and repeat them several times since they are ao volatile tht its easy to understand yet easier to forget.


A young child presented with multiple warts on dorsal surface of hands and arm, increasing day by day .
*What are the causative organisms*
Common warts (excluding plantar warts) are due mainly to HPV‐2, but also to the closely related types 27, 57 and types 1 and 3, 4 and 10 .
**What is the mechanism of salicylic acid for viral warts ?*
The keratolytic effect of salicylic acid helps to reduce the thickness of warts and may stimulate an inflammatory response.
It peels the skin away in layers by decreasing cohesiveness of of cells and stimulates immune system. Due to peeling virus cannot proliferate.
*What are the formulations available?*
A preparation containing 12–26% salicylic acid in a quick drying collodion and acrylate base
Adhesive plaster containing 40% salicylic acid is useful for plantar warts.
*What are the hazards of using salicylic acid for warts ?*
use of salicylic acid on feet with neuropathy or impaired circulation, as in diabetics, must be cautious due to the risk of producing ulceration which may not heal.
Salicylic acid in the usual concentrations is best avoided on facial warts, but less irritant concentrations in cream formulations can be helpful, especially for plane warts.
Before using salicylic acid, tell your doctor or pharmacist if you are allergic to it or to nonsteroidal anti-inflammatory drugs-NSAIDs (such as aspirin, ibuprofen, naproxen)or if you have any other allergies.
*Post treatment precautions?*
Do not touch rub or scratch the lesions .
Do not share towels .
Try to avoid frequent contacts with other children or family members for sometime.
*What are the side effects of salicylic acid preparations?*
Irritation, burning sensation, dryness, erythema , peeling of skin .tingling , itching Propagation to ulcer formation in case of neuropathy .
*What are the other treatment options of viral warts .*
Topical …
10% glutaraldehyde in aqueous ethanol or in a gel form.
Formalin 2 3 %soaks .
Occlusion,
topical 5% 5fU , retinoic acid .
2nd line .
cryotherapy , laser , PDT , hyperthermia , surgery,.
3rd line ….podophylootoxin ,imiquimod,
Dinitrochlorobenzin as topical immunotherapy , candida albicans antigens. Interferon , oral cimetidine.zinc , cidofovir , intralesional bleomycin .
*
*Salicylic acid toxicity???**
Salicylic acid toxicity is rare, but it can occur from topical application of salicylic acid. To reduce your risk, follow these recommendations:
- do not apply salicylic acid products to large areas of your body
- do not use it for long periods of time
- do not use it under air-tight dressings, such as plastic wrap
Immediately stop using salicylic acid and see your doctor if you experience any of these symptoms or signs:
- lethargy
- headache
- confusion
- ringing or buzzing in the ears (tinnitus)
- hearing loss
- nausea
- vomiting
- diarrhea
- increase in breathing depth (hyperpnea
*Contraindications* .
Skin is already damage , will lead to irritation and ulcers.
Neuropathy due DM
American College of Obstetricians and Gynecologists (ACOG) notes that topical salicylic acid is generally safe to use while pregnant.
salicylic acid during breastfeeding noted that while salicylic acid is unlikely to be absorbed into breast milk, you should not apply it to any areas of your body that might come into contact with an infant’s skin or mouth.
For which areas of the body the salicylic acid for wart should be avoided?
☆ Face, genitalia and mucosae
- How would you treat warts during pregnancy?
☆ Cryotherapy
- What are other treatment options for planter warts?
☆ Electrocautry, cryotherapy, topical 5 FU, IL Vitamin D analogs, retinoic acid, imiquimod laser, surgery, photodynamic therapy
- What are treatment options for the genital warts?
☆ Podophyllotoxin, imiquimod, cryotherapy, surgery, laser, photodynamic therapy
conc of salicylic normally we give to patients for plantar warts is 16%
before starting the procedure and also gloves should be weared while performing the dressing
🔰Start with explaining what viral wart is
🔸ye virus se hta hy Jo elaaj na krane ki Surat mn mazeed phel skta hy or Apne shoes or towel share na krn
Ye tareeq elaaj krne se pehle apse chand sawal krn g
Ask about any hx of disprin allergy, hx of skin disease, hx of neuropathy, hx of diabetes, previous reaction to same treatment if done before,
Then counsel about the method u will perform and post procedure care not explained i.e
Don’t wet your dressing
Don’t remove it by yourself
Come back after 48 hrs for removal
In case of severe irritation pt can remove the dressing and come back to the treating doctor
Tell pt that multiple sessions may be required n after removal of dressing the hyperkeratotic skin that would be soften will be removed and further dressing if required will be done.


Viva question and answers
👇🏻👇🏻👇🏻
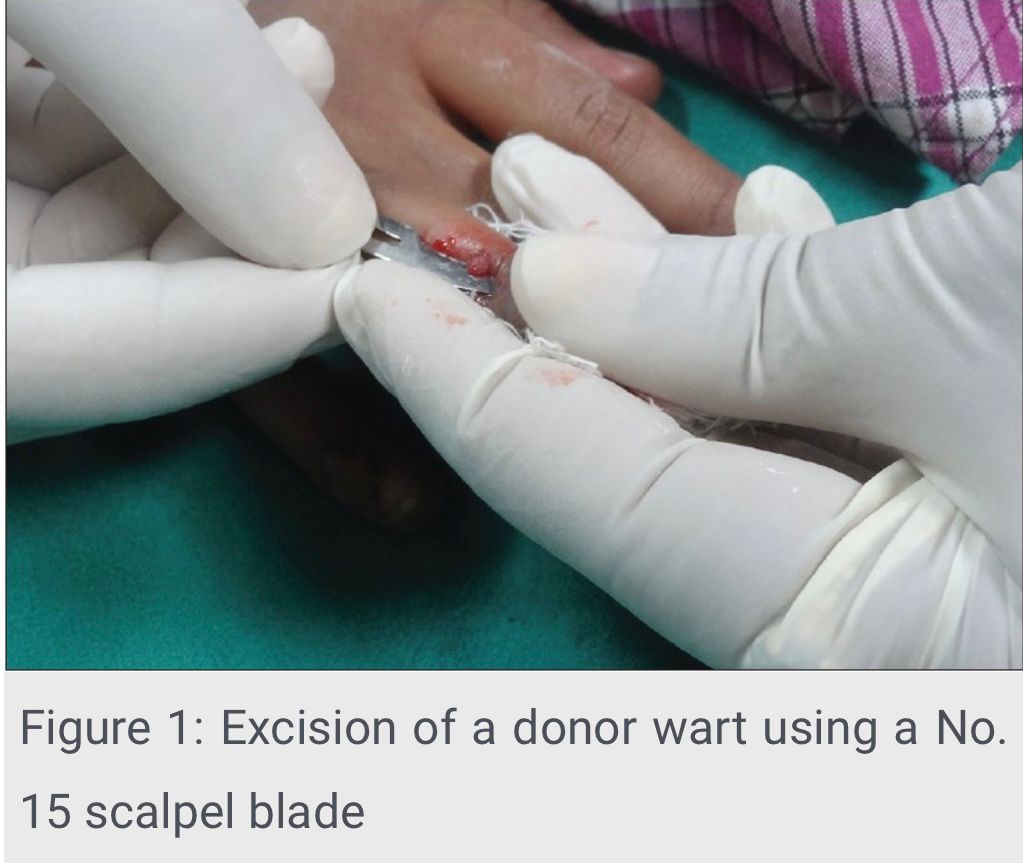
🟥What is Autoinoculation of warts? Explain its significance.
This is a latest modality for the treatment of refractory warts, in which a wart from a patient is removed with a 15 number blade, minced into a thin film like material on a glass slide or a petri dish. Then a deep dermal pocket is created 5cm in front of the antecubital fossa extending up to the subcutis and the wart tissue is placed in this pocket. Wart from an infected patient is inoculated in the same person but at a different site. Response is assessed every 4 weeks by follow up.
🟥Explain how autoinoculation of viral warts works for clearance of recalcitrant warts.
It works by activating delayed hypersensitivity reaction to wart tissue antigens placed in the dermis.
Intralesional antigen therapy has been shown to alternate the cytokine profile to a predominant Th1 subtype inducing strong cell mediated immunity. The Th1 cytokines TNF-alpha and IL-1 downregulate HPV genes and IL-2 stimulates cytotoxic T cells to eradicate HPV infected cells.
🟥Which patients are candidates for autoinoculation therapy?
It can be a useful treatment modality for patients with
⭕Recalcitrant warts
⭕Those with multiple warts
⭕Patients with genital warts, subungual and periungual warts that are otherwise hard to manage
🟥 Contraindications?
Pregnancy, lactation.
Immunosuppressed patients
Patients with keloidal tendency.
Patients with known hypersensitivity to local anaesthetic agents.
🟥What is the effectiveness of this method?
Studies shows response rates of 60-97%.
🟥 What makes this procedure suitable to be used in our setting?
It’s effectiveness, cost effectiveness and simplicity of procedure which can be easily performed in a minor OT without needing any expensive, or specialized material make it particularly suitable for resource poor countries such as ours.
🟥Which type of warts respond best to autoinoculation?
⭕Verruca vulgaris 》 verruca plana and filliform warts.
⭕Warts lasting less than one year responded better.


🔰 Preparation of LASSAR paste with viva Questions and Answers*
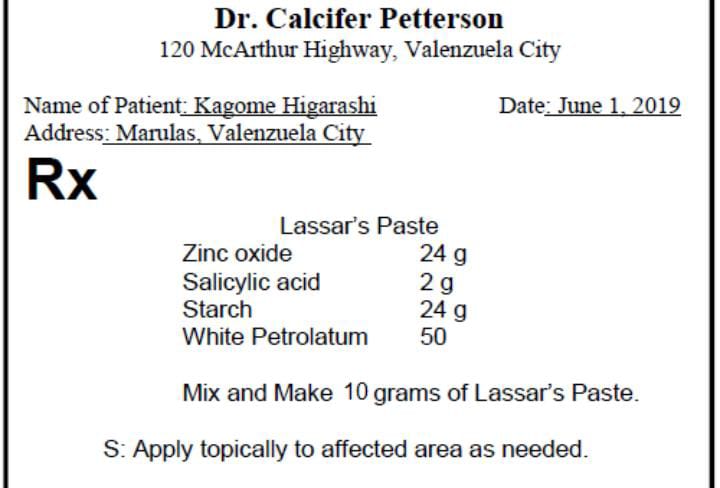
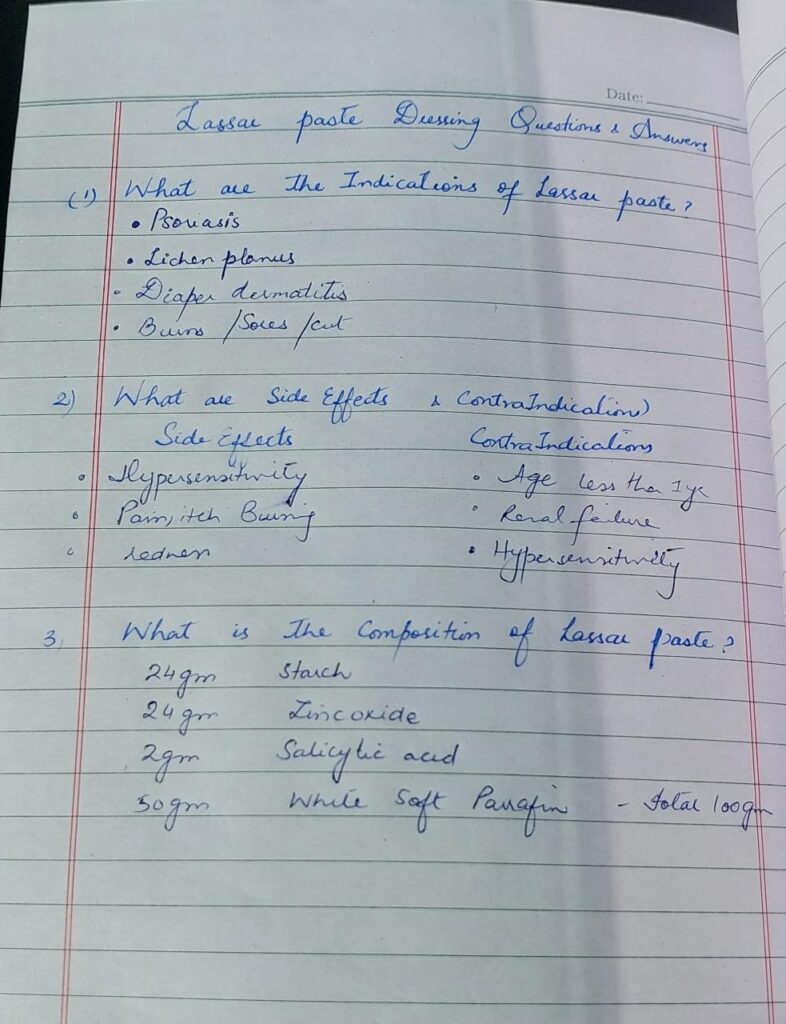
inquire about pregnancy as its safety is not well established during pregnancy.
If a bottle of lassars paste is given in exam then look for its expiry date. Its shelf life is 3 years/ if u prepare it lable the bottle for date and appropriate storage temperature 25°c / only for external use
🔰 Nail NAPSI with viva Questions and Answers*
https://youtu.be/HjuZlMzfU68
MODIFIED NAPSI SCORE ;
Three features (putting , onycholysis, oil drop dyschromia, and crumbling) of each fingernail will be graded on a scale from zero to 3.
Four features (leukonychia, splinter hemorrhages, hyperkeratosis, and red spots in the lunula) will be graded as either present or absent for each fingernail.
*1. What are nail changes in psoriasis*
🔴Changes of nail matrix pitting, ridges, grooves, leukonychia, red spot in lunula, nail plate crumbling
🔴Changes of nail bed Onycholysis, splinter haemorrhages, oil drop sign (salmon patch), subungual hyperkeratosis
*2. What is significance of NAPSI score?*
🔴significance of NAPSI score is to see the improvement or aggravation of nail disease in each visit of pt
*4. Name some other nail scores for psoriasis?*
🔴BARAN’s nail severity index
🔴NAPPA (Nail assessment in psoriasis and psoriatic arthritis)
onycholysis or oil-drop dyschromia
0 No onycholysis or oil drop dyschromia present
1–10%
2 11–30%
3 > 30%
Pitting
0 0
1 1–10
2 11–49
3 > 50
Score Percent of nail with crumbling present
0 No crumbling
1 1–25%
2 26–50%
3 > 50%
Following findings can be graded as
0 absent
1 present
Leukonychia:
Splinter hemorrhages:
Red spots in the lunula:
Modified napsi score 👆🏻
Marking and dosage of botox injection on palm of a patient with hyperhidrosis with viva Questions and Answers.
Viva questions n answer
1) what are the non cutaneous indications of Botox
Ans: muscle spasitcity
Squint
Tremor
Migraine
Bowel outlet obstruction
Urethrism
Parkinsonism
Nystagmus
Hypertonic bladder
Blepharospasm
Chorea
Q2 what is the mechanism of action of Botox?
Ans: it cleaves protein SNAP 25 and inhibit exocytosis of ACH into neuromuscular junction
Q3 in which muscle to
inject Botox for gummy smile
Ans levator labbi superior alq
Aeque nasi
Q4 what is Spock brow
Ans imbalance between muscle that lift brow and muscle that cause brow to drop
It can b fixed by adding small amount of additional botulinum to frontalis muscle
botox is injected at 15-20 sites on palm almost 1 cm apart.
ask the patient about any contraindications to botox i-e myasthenia gravis
hypersensitivity to botox
lambert eaton syndrome
multiple sclerosis
pregnancy
lactation
and relative contraindications
About zinc supplements,dipenicillamine,aminoglycoside
Perform iodine starch test for hyperhydrosis along with viva Questions and answers
Viva ques n ans
How much iodine solution ?
2%
What is mechanism
Sweat dissolve iodine and starch resulting in polypeptide chain due to chemical reaction
What are alternatives if person is allergic to iodine
Allazurin or ponceau red dye
Causes of false +
If skin not dried properly
False -ve
If starch too heavily applied
What is gold standard test to check hyperhidrosis ?
Gravimetery
How to do check on gravimetry ?
Filter paper is weighed before n after exposure to axillary skin for 60sec to 5 min
Weight difference quantify amount of sweat produced
How much units of Botox in one axilla
50 units






🔰Marking and dosage of botox injection on palm of a patient with hyperhidrosis , with viva Questions and Answers
https://youtu.be/7DQtB2YUfng
Botox reconstitution technique
botox also comes in 50 units vial not just 100 units. You should also know how to dilute a 50 units vial as in came in one of the preparatory toacs last year.
Preparation of Botox:
2.5ml normal saline is added in vial having 100 units of botox to obtain a concentration of 4units /0.1 ml.Gently mix the solution.
- MECHANISM OF ACTION
ANS. Bind presynaptically to high affinity cholinergic nerve terminals and decrease the release of acetylcholine.
- No. Of units per vial
ANS. 100u
- Expiry after preparing
Ans. expiry after preparing is 4 hours if not refrigerated .
Once refrigerated it can be used for 4 weeks if no chance of contamination
- Follow up
Ans. After 2 weeks
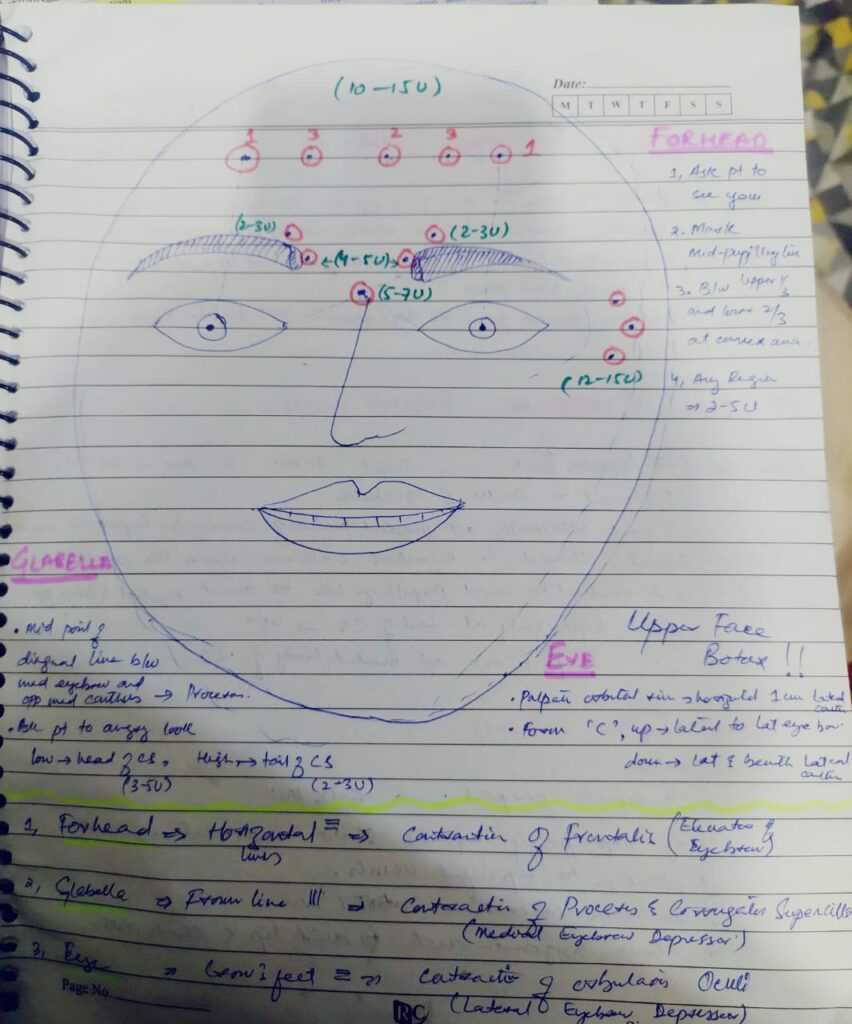
BOTOX for upper face with viva Questions and Answers*
Viva Notes
*1.What is Mephisto lines and how it is corrected ?*
Frontalis muscles can extend
laterally and if not treated this can induce a
‘Mephisto look’. This peaked brow can be
brought down by the injection of 1–2 MU onabotulinum in the lateral temporal part of the
frontalis muscle.
*2.How botox is diluted?*
BTX powder 100U diluted in 1ml-4ml of 0.9% Normal saline…
When 100U Of BTX diluted in 2.5 ml NS means
2.5= 100U btx
1ml (100u of Insulin syringe) contain 40U of BTX means
0.1ml(10u of insulin syringe have ) 4U of BTX
*3.What is cumulative toxic dose of Botox?*
360U in 3months
*4.Why blepharoptosis occur , how it prevented and treated ?*
Due to deep migration of BTX to levator palpebral superioris
Prevented by placing BTX 1 cm.above supraorbital ridges at MPL
Treated by 0.5% apraclonidine (alpha adrenergic effect)
*5. How u treat eyebrow ptosis*
Injection BTX at Procerus and Corrugator ( Natural eye brow depressor).
explain the pt that its a temporary procedure so its effect will last for about 6 months and it takes 7-10 days for complete effect of procedure so call the pt for follow up after 1 week. Also while doing procedure pt should be at 45 degrees and ask the pt to remain upright in sitting or standing position
🔰 Important tip for Botox station👇🏻
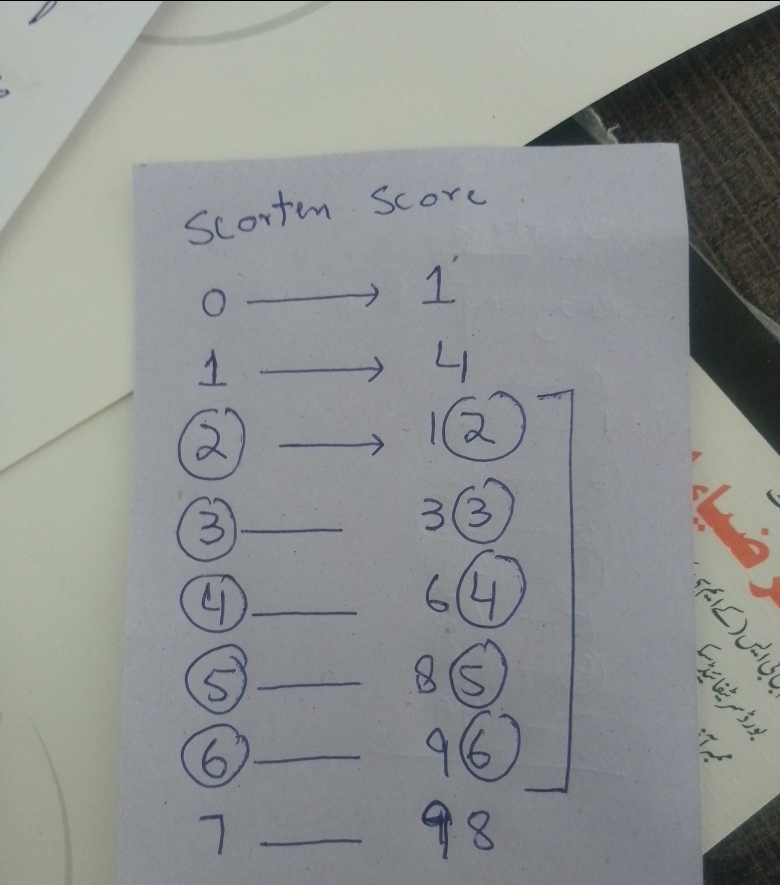
For Scorten easiest way to remember is with pic given above 👆🏻
Practice these score calculations with various scenarios and pic and it will be easy in exam
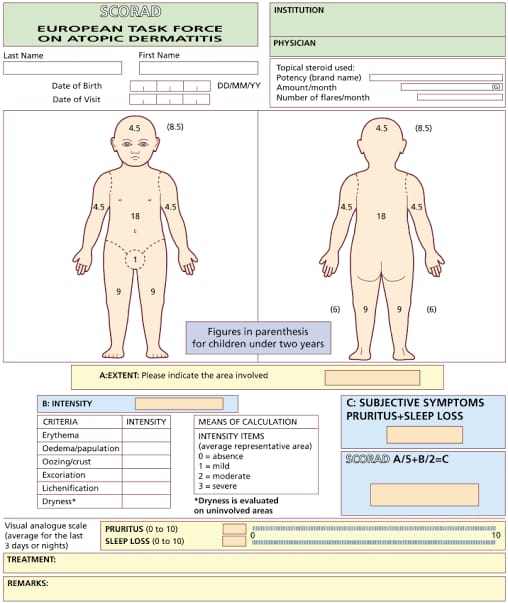
Important Scores to Remember for clinical exam
- SCORTEN (Severe Cutaneous Adverse Reactions)
- PASI (Psoriasis Area Severity Index)
- NAPSI (Nail Psoriasis Severity Index)
- MASI (Melasma Area Severity Index) & modified MASI
- Modified Rodnan Score (Systemic Sclerosis)
- DLQI (Dermatology Life Quality Index)
- RegiSCAR Dress Score (Severe Cutaneous Adverse Reactions)
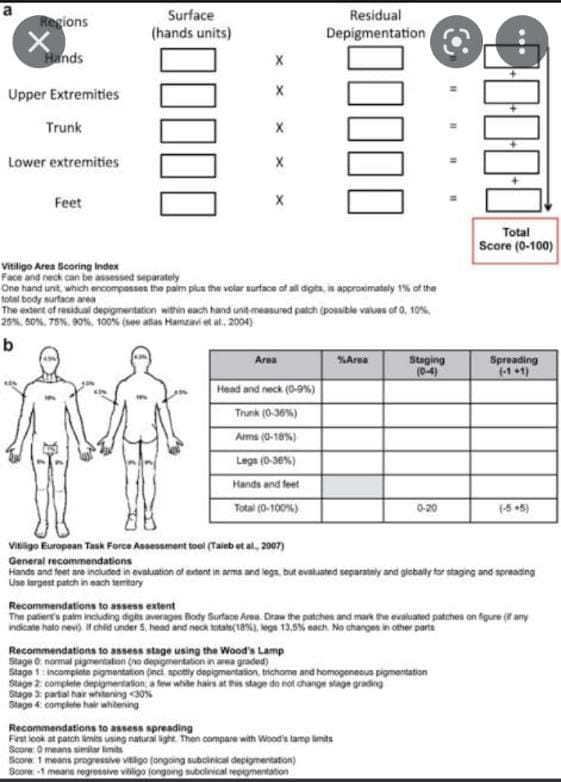
- VASI (Vitiligo Area Scoring Index)
- SALT Score (Severity of Alopecia Tool)
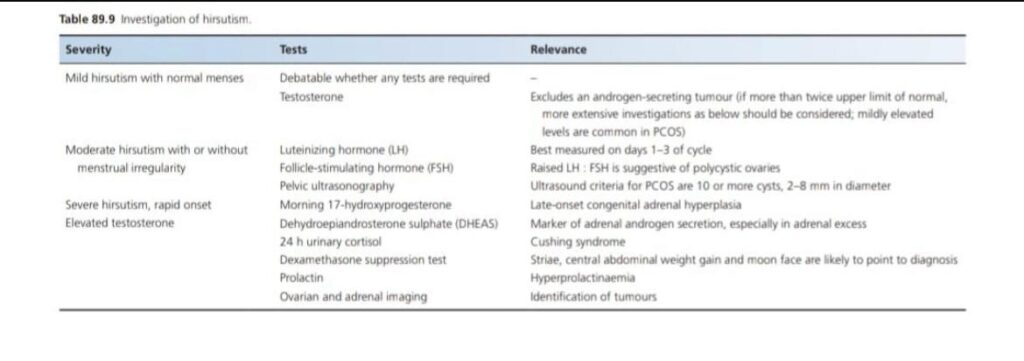
- Ferriman-Gallwey Score (Hirsutism)
- Hidradenitis suppartiva severity score
In exam there is often one station of score which you have calculate it and answers the question asked by exmainer
*Wrist Block (For botox for palmar hyperhyhydrosis)*
*Q1: what are the dermatological indications for wrist block?*
Ans: a. To perform botox for palmar hyperhydrosis
- To perform biopsy for any benign, malignant lesion on palm
- To repair any palmar laceration or injury in emergency
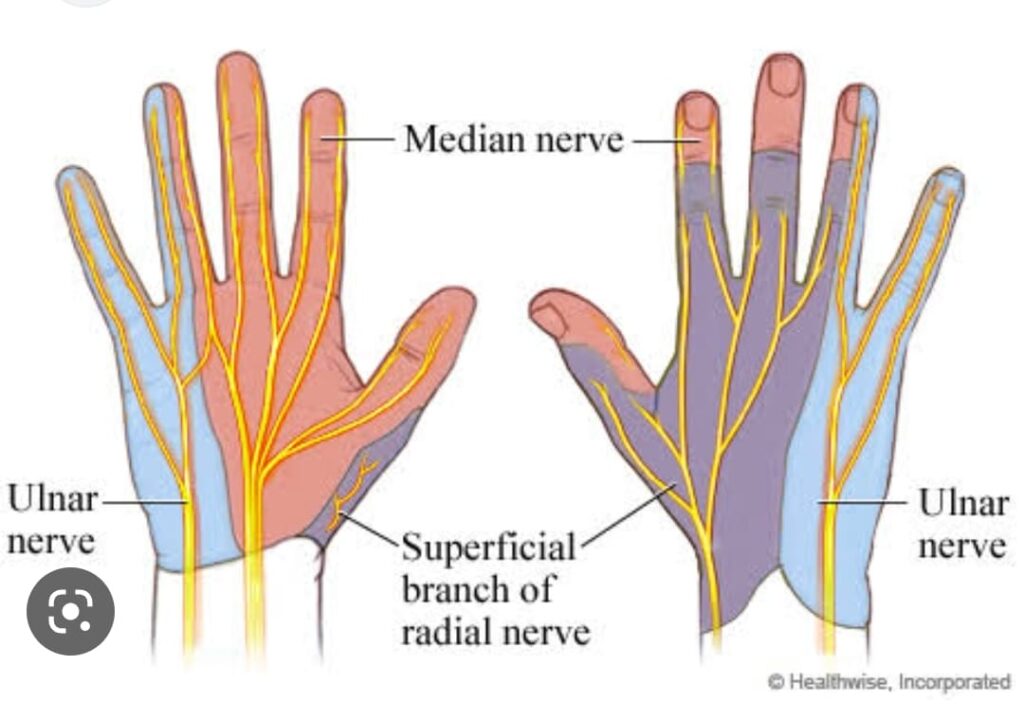
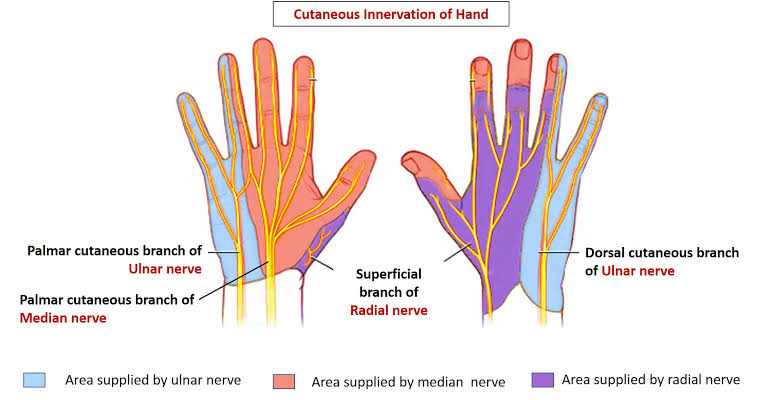
*Q2: what is the sensory nerve supply of hand?*
Ans: picture attached
*Q3: what is the safe dose of lidocaine for an individual?*
Ans: adult=4.5mg/kg plain & 7mg/kg mixed with adrenaline
paediatric and old age dose is half the adult dose.
*Q4: what are 2 groups of local anesthetic?*
Ans: ester and amide
*Q5: which one is better?*
Ans: Amide,lesser side effects and hupersensitivity
*Q6: What is absolute contraindication to local anesthesia?*
Ans: •history of hypersensitivity reaction
- infection on wrist
*Q5: What is lidocaine toxicity?*
Ans: The effects on CNS
Early: diplopia,tinnitus, lightheadedness, nausea, circumoral pallor, vomiting
mid: slurred speech, muscle twitching, tremors, seizures
late: apnea, coma, bradycardia, AV block, hypotension, arrythmia, hypoxia
*Q6: How do u treat lignocaine toxicity?*
Ans: Early: recognize and observe
Mid: observe, oxygen, diazepam for seizures
Late: ACLS protocol
*Q7: Alternative to local anesthesia?*
Ans: normal saline or 10-25 mg/ml diphenhydramine
*Q8: how to treat vasovagal shock?*
Ans: Trendelenburg position, feet raised head down , wet cloth over face, save IV LINE for fluid if needed
In history these points are imp to ask 👇🏻
. history of peripheral arterial disease
. Diabetes mellitus
.profession of patient as treatment modality was Botox
In advising Botox to patient it’ very important to ask about profession of patient
.hx of previous Botox use
.any history of neuromuscular disease
.any recent history of medication like amingolycoside and zinc
For local anesthesia of hand there are multiple block so kindly read scenario carefully what you are ask to do
. wrist block
. interdigital block
Distal digital block
In one of mock exam in the question was to do nail matrix biopsy by doing distal digital block
And many candidate were doing interdigital block instead of distal digital block
Also you should know about different approach of distal digital block
One important point is to give local anesthesia without adrenaline
One important question to know about cross reactivity btwn local anesthetic with other allergens
For intralesional Glucantime injection anesthesic button and saturation of lesion is very important
Further question which can ask exmainer
.Indication of systemic treatment in leishmaniasis
. second line treatment for cutaneous leishmaniasis
. indication of intraleseional in cutaneous leishmaniasis
.how to calculate intramuscular injection dose per day
. price of one vial of inj Glucantime
. duration of treatment of intramuscular Glucantime
For Facial and mucosal lesion and where there is risk of scarring, I/L glucantime would be disfiguring and hence its an indication for systemic treatment
Mesotherapy in a patient of melasma
- What Is Mesotherapy and its indications?
Ans. Mesotherapy is a procedure in which vitamins, enzymes, hormones, and plant extracts are injected into the skin( Mesoderm)to rejuvenate and tighten it. It is also used for removing excess fat and for the treatment of alopecia, wrinkles, cellulite and melasma.
- How frequently the mesotherapy sessions are done?
Ans. In the beginning applications are carried out every other week for 2 months with following treatments once a month for another 2 months. To maintain the result it is advisable to have an application twice a year.
- Which agent gives best results used for mesotherapy in Melasma?
Ans. Mesotherapy injected with tranexamic acid proved to be an effective and safe procedure for treating melasma. It provides faster results to the people undergoing this treatment.
- What is EMLA cream?
Ans. Its is topical anesthetic cream which contains lidocaine 25 mg and prilocaine 25 mg and is available in 5% cream.
- How long EMLA cream takes to start its effect?
Ans. It takes 30 to 60 minutes and its maximal effect is achieved in 2 hours.
- What are side effects of mesotherapy?
Ans. nausea
pain
sensitivity
swelling
itching
redness
bruising
bumps at the injection site
dark patches of skin
rash
infection
scars
- What are contraindications of Mesotherapy?
Ans.The contraindications to mesotherapy include a body mass index greater than 30, known hypersensitivity to any of the components, less than 18 years of age, pregnancy, lactation, patients on anticoagulants, cardiac drugs (like amiodarone, hydralazine, calcium channel blocker, beta blocker), disease conditions like insulin dependent diabetes, liver and kidney disorders, AIDS, seizure disorders and lupus. Those who have used Accutane (isotretinoin) within the last three months. Have open wounds, cuts or abrasions on the skin. Have had radiation treatment to the skin within the last year.
- The injections of Mesotherapy are given at which level of skin?
Ans. Intradermal and subcutaneous (Mesoderm)
- What is recovery time after Mesotherapy?
Ans. Because mesotherapy is noninvasive, there usually isn’t any downtime. Many people are able to return to their regular activities right away. Others may need to take a day off due to swelling and pain at the injection sites.
- Which substances can be injected in Mesotherapy?
Ans. Vasodilators and antibiotics
hormones such as calcitonin and thyroxin
enzymes like collagenase and hyaluronidase
herbal extracts
vitamins and minerals
- How to prepare for Mesotherapy?
Ans. You might have to avoid aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) for one week before the procedure. These pain relievers can increase your risk of bleeding and bruising during mesotherapy.
- How deep the injections are given?
Ans. The injections can be given at different depths — from 1 to 4 millimeters into your skin — depending on what condition you’re having treated.
- What is post procedure care after Mesotherapy?
Ans. Clean your face with a gentle cleanser and warm water
Try not to wear makeup.
Use creams with antioxidants and hyaluronic acid to reduce irritation and hydrate the skin.
Avoid active skincare products which contain: Alpha Hydroxy Acids, Beta Hydroxy Acids, Retinol (Vitamin A), and Vitamin C (in low pH formula). Continue to do so for 3 days post treatment.
Avoid strenuous exercise for 24 hours.
Avoid sun , Steam rooms or heat for 72 hours.
Avoid consuming excess amounts of salts to avoid excess swelling.
If you have swelling you may apply a cool compress for 15 minutes each hour.
Use Paracetamol for discomfort. Do not takeu Ibuporfen for two weeks after the treatment.
- Advantages : more economical , easy to perform , less down time.
15.can be used for post acne pigmentation, post inflammatory hyperpigmentation.
Try to sleep face up and slightly elevated if you experience swelling.
. *What is the mechanism of action of tranexamic acid in treating melasma?*
Ans.Tranexamic acid is a plasmin inhibitor, with the synthetic derivative of amino acid lysine that works by reversibly blocking lysine binding sites on plasminogen molecules to inhibit the plasminogen activator from converting plasminogen to plasmin.
The main mechanism of the hypopigmentation effects of TA is due to its antiplasmin activity, with a structural similarity relative to tyrosine that can inhibit tyrosinase competitively.
👀 _Tips and tricks To avoid hematomas/bleeding:_
✍️• Do not perform mesotherapy during a patient’s menstrual period.
✍️• Do not let the patient take aspirin or a nonsteridal anti-inflammatory drug (NSAID) for a few days before and a few days after the procedure.
✍️• Inject the product slowly, to avoid the high pressure breaking vessel walls.
✍️• Apply antibiotic cream after each session.
To avoid pain, in sensitive patients: • Pinch or stretch the skin during the injections.
✍️• Perform the injections precisely. • Change the needle several times during each treatment.
✍️• Choose products containing lidocaine or apply Emla cream 1 hour before treatment.
✍️• Talk with the patient a lot during the session!
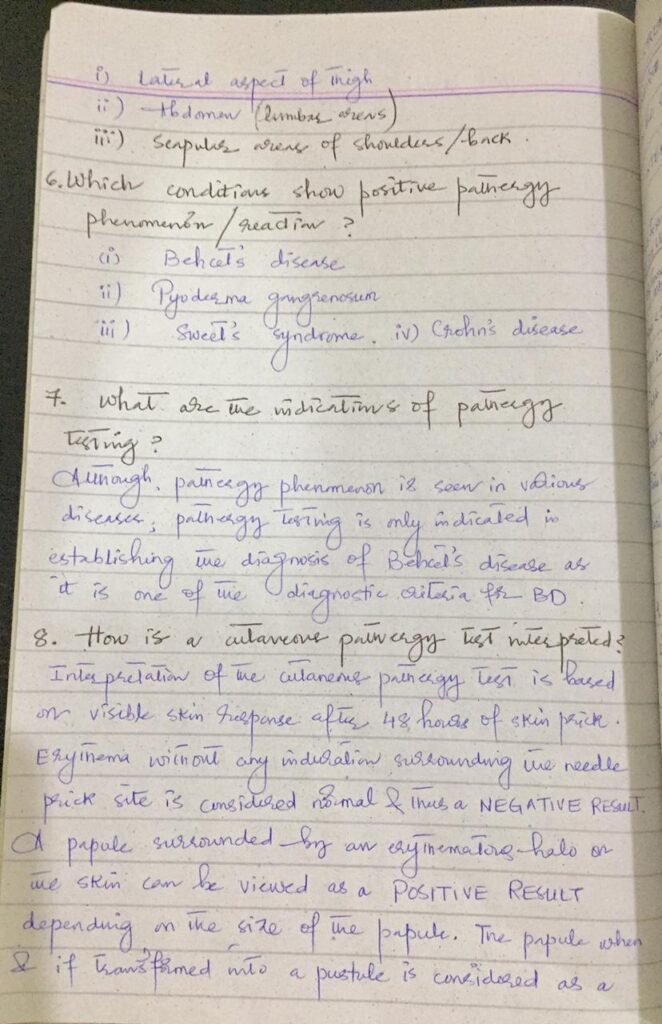
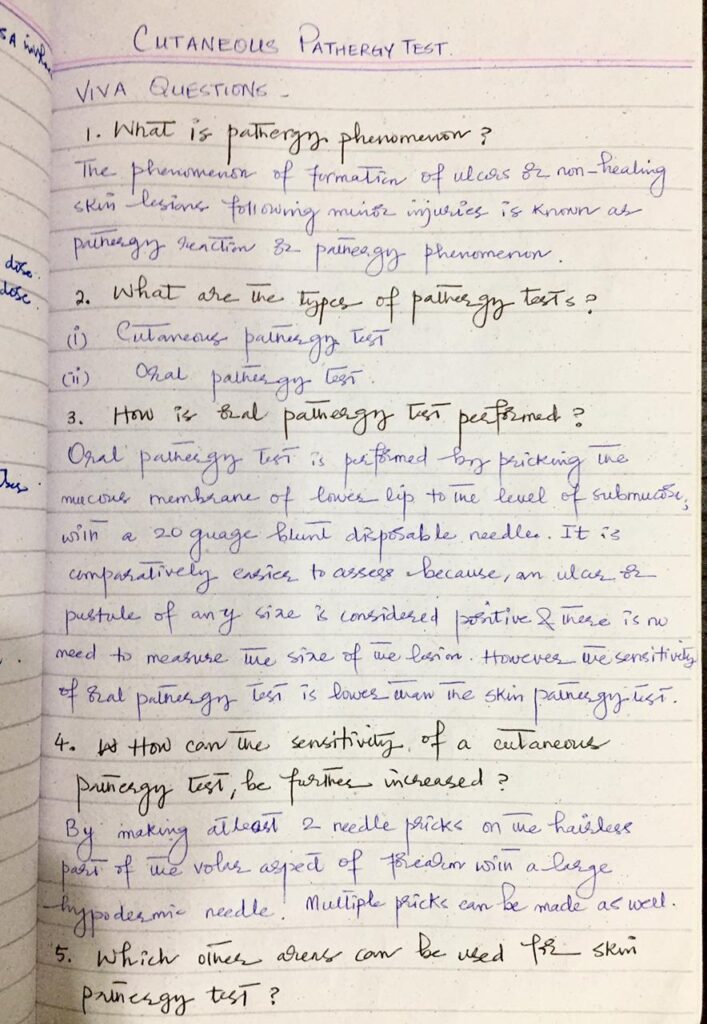
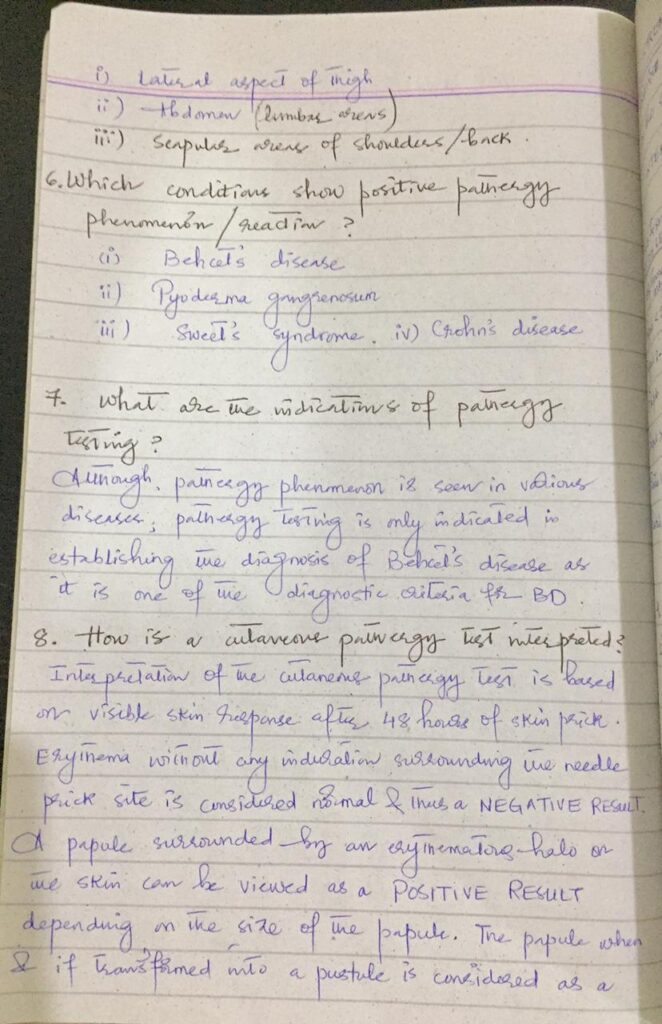
A 32 year old female patient has presented to the Dermatology OPD for recurrent oral and genital ulcers since last few years.You are suspecting Behcet disease and plan to do a pathergy test.How will you proceed?
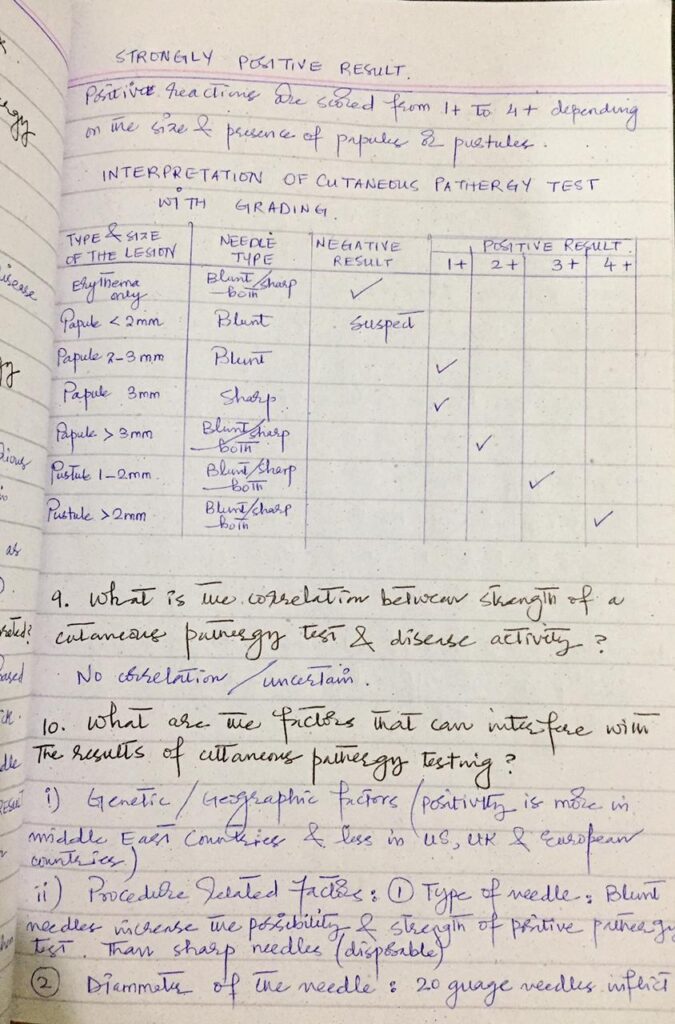
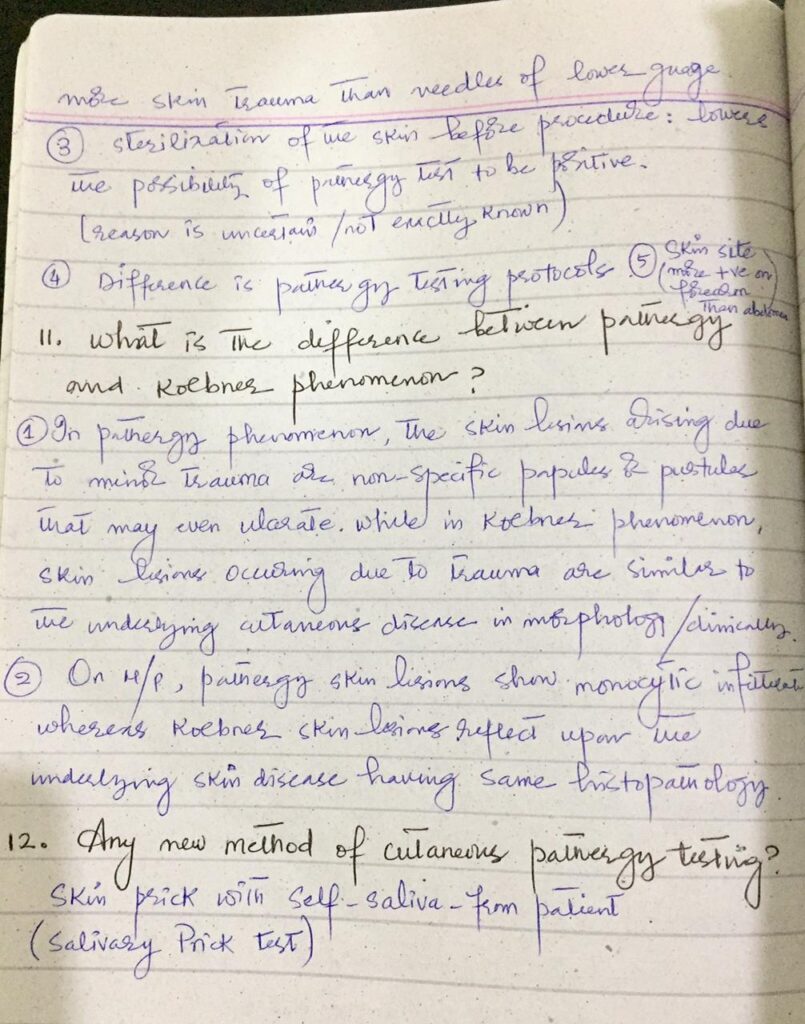
💥What is Pathergy phenomena and pathergy test?
Ans: Pathergy phenomenon is a state of altered tissue reactivity that occurs in response to minor trauma. Pathergy test is an easy to perform skin test to look for the pathergy phenomenon. This test is used as a criteria for Behcet′s disease.
💥Which type of hypersensitivity is pathergy test?
Ans: Type 4 hypersensitivity delayed type cell mediated reaction.
💥What are other sites in which pathergy phenomena occur?
Ans: Any disruption of tissue integrity is potentially associated with an exaggerated inflammatory response in Behcet′s disease.
1.Posttraumatic arterial thrombus and/or aneurysm formation following conventional angiographic interventions
2.superficial thrombophlebitis induced by venipuncture
3.eye inflammation after intraocular corticosteroid injections
4.And anastomotic ulcers following surgical treatment of intestinal ulcerare well known examples of pathergy reactions triggered at different tissue sites.
💥What is Pathogenesis of pathergy phenomenon?
Ans: Although the exact mechanisms underlying pathergy phenomenon are unknown, skin injury caused by needle prick apparently triggers a cutaneous inflammatory response which is much more prominent and extensive than that seen in normal skin and suggests an increased or aberrant release of cytokines from keratinocytes or other cells in the epidermis or dermis resulting in a perivascular infiltration observed on skin biopsy.
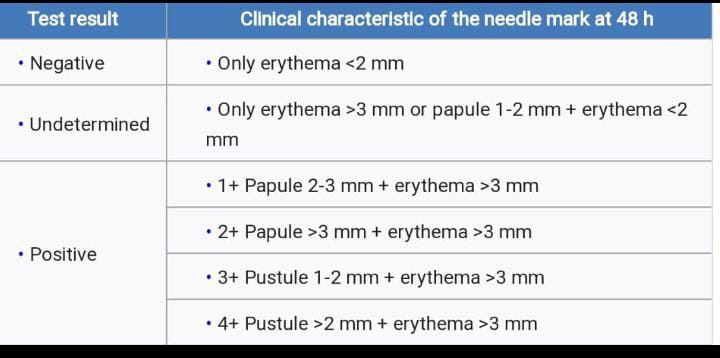
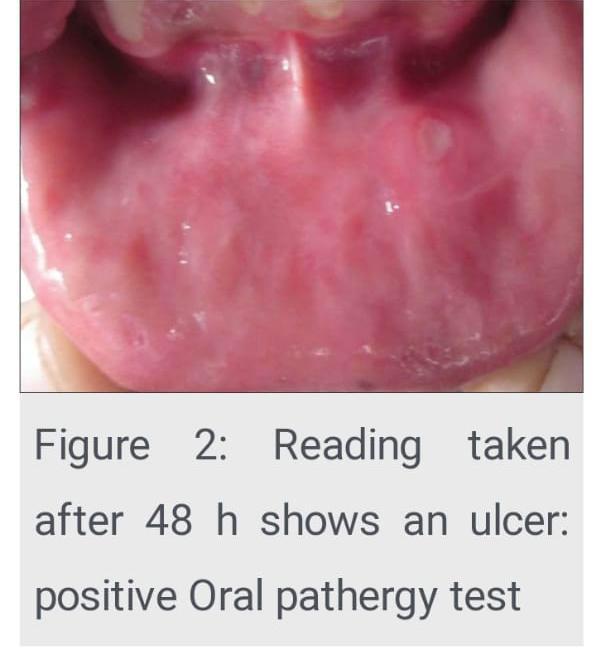
💥What are Types of pathergy tests? And how to perform and their advantage and disadvantages?
Two types
Oral pathergy test
Site: lower lip.
Procedure of oral pathergy test : prick the mucous membrane of the lower lip to the submucosa using a 20 gauge blunt disposable needle
Assessment: Readings are taken after 48 h, and the test is considered positive if a pustule or ulcer is seen.
Disadvantage
Sensitivity: The sensitivity of the oral PT is lower than that of the ordinary skin pathergy test.
Advantage over the skin pathergy test: The oral PT is easier to assess than the skin PT as there is no need to measure the size of the lesion: a pustule or ulcer of any size is considered positive.
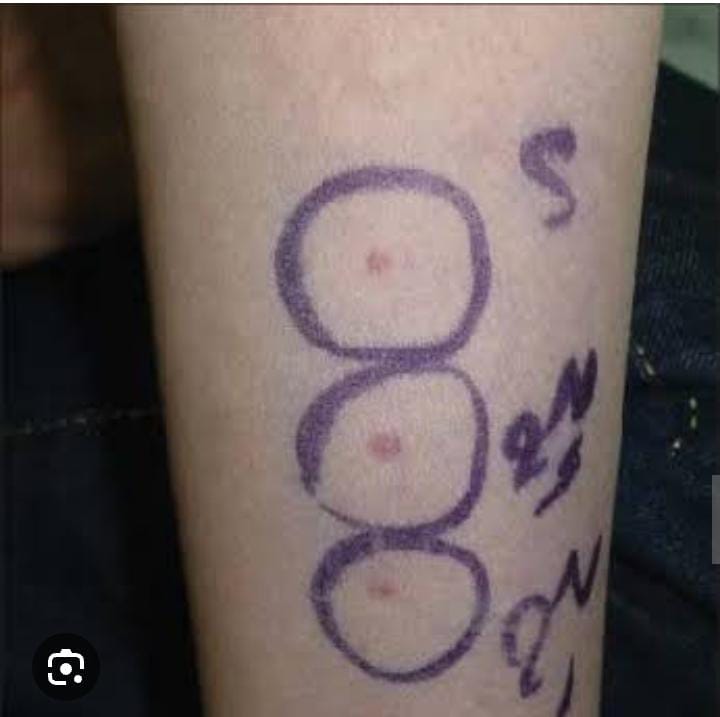
Skin pathergy test
Site: A hairless area on the flexor aspect of the forearms is usually chosen as the test site.
💥What are other routes for pathergy test?
Various routes for skin pathergy testing:
Intradermal (ID)
intravenous (IV)
and subcutaneous methods have been used.
In a study the positivity rate yielded by intradermal needles was statistically higher than that by IV application in Behcet′s patients during both the active and remission periods.
What are Conditions with positive pathergy phenomenon?
Ans:
Behcet′s disease
Pyoderma Gangrenosum
Sweets syndrome
Eosinophilic pustular folliculitis
Inflammatory bowel disease
Healthy individuals
💥What are sites for skin pathergy test?
Ans:
The flexor surfaces of the forearms The lateral aspect of the tibial area
The scapular areas of the back
And the lumbar areas of the abdominal region
A hairless area on the flexor aspect of the forearms is usually chosen as the test site.
Inform the patient that they may feel a sharp prick or a brief sting when the needle is inserted. Also inform about bleeding and bruising (some patients are phobic from the blood and some have to attend an event)
Recommend avoiding the application of any creams, lotions, or other products to the test site ( to prevent allegic contact dermatitis)
Advise the patient to report any signs of infection, excessive redness, swelling, or other unusual symptoms.
U used 5 cc syringe which has 23 guage needle? It should be 20 Guage needle.
I would also like to add
Q: What are the limitations of the pathergy test?
A: The pathergy test has a number of limitations, including its lack of specificity for Behcet’s disease, variation in test performance and interpretation, and the influence of external factors such as the technique used and the patient’s geographic origin.The size of the needle, the depth of the needle insertion, and the site of the test can all affect whether a pathergy test result is positive or negative.



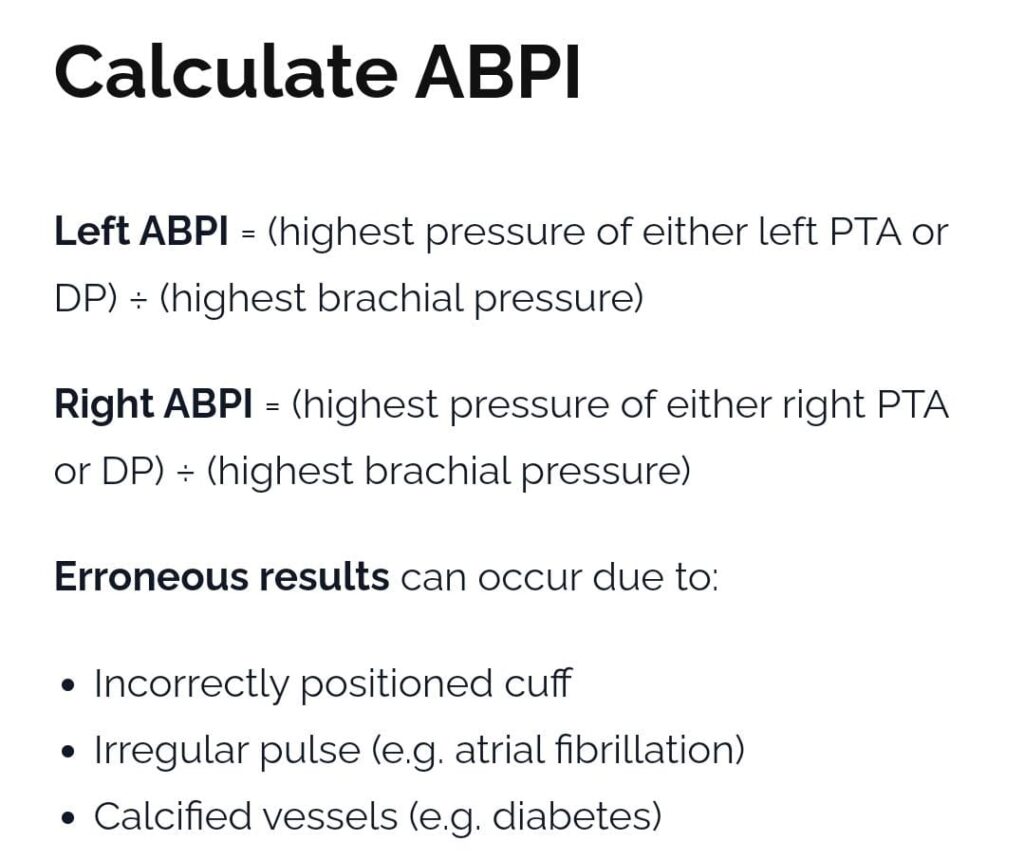
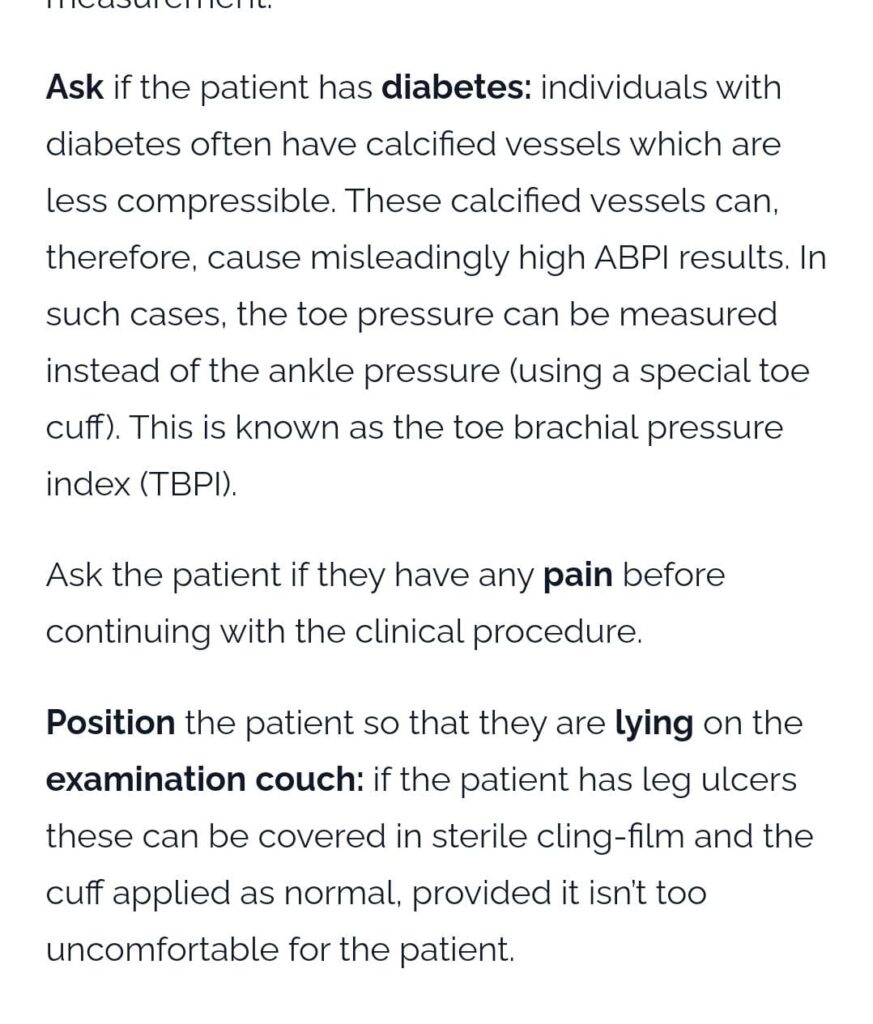
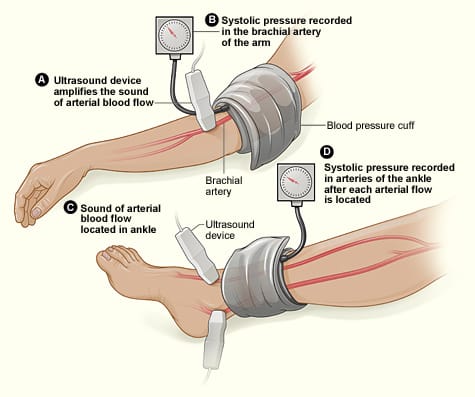
Patient having a leg ulcer just above right ankle. Calculate ABPI with an example.
- Before going for procedure , first always inspect and examine the ulcer , also look for lymphedema, skin changes like cold shiny hairless skin etc
- Also ask some personal history questions like hypertension, DM etc
- Also rule out contraindications like intermittent claudication, DVT, any infection on the site, difficulty in lying supine.

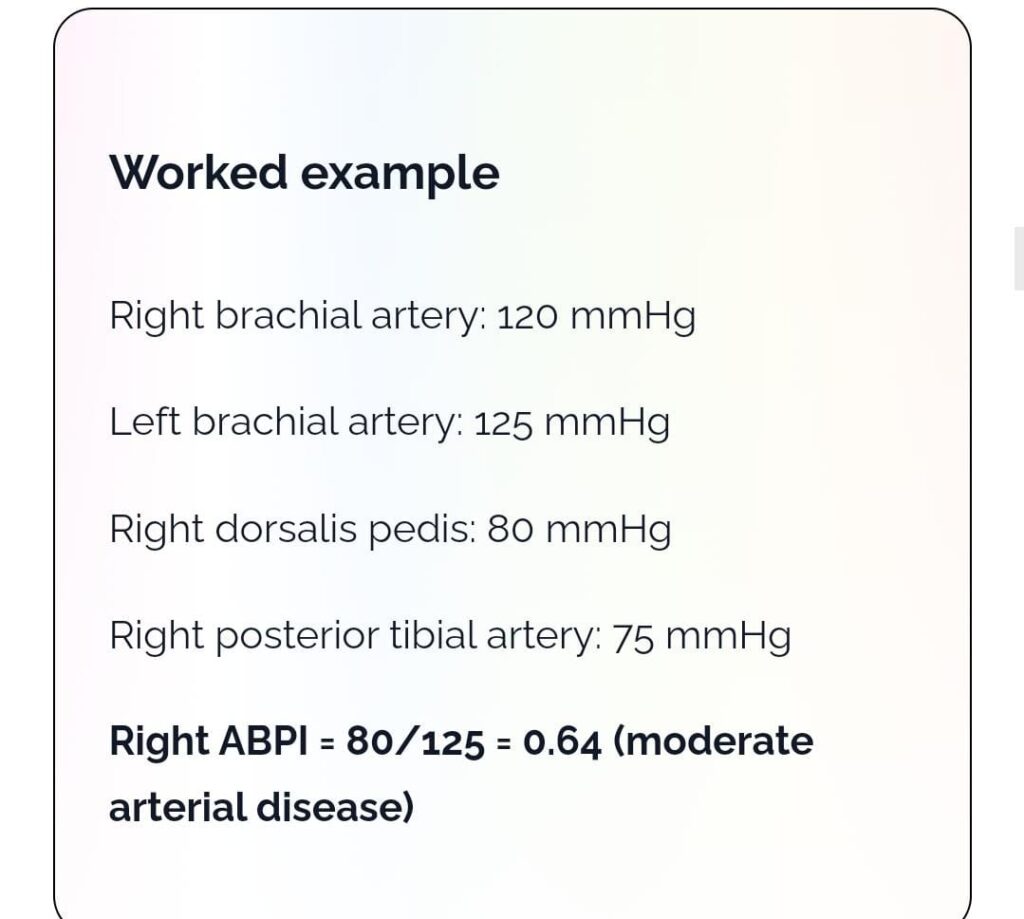

https://youtu.be/gUgIcOhYNH8
Best videos for toacs👆🏻
But Also memorise it’s inclusion and exclusion criteria
🛑Inclusion Criteria for SALT scoring ?
🟢localized scalp AA ( 2 patches and ≤50% scalp involvement
🟢 Duration more than 6 months
🟢patients who did not receive any medication for at least 2 months
🛑Exclusion Criteria for SALT scoring ?
pregnant, and lactating females
🔸Alopecia totalis or universalis or ophiasis or cicatritial alopecia
🔸Usage of systemic treatment of alopecia areata 2 months prior
🔸Any scalp lesion within the treated area
🔸Bleeding diathesis, severe anemia or platelet disorders
🔸Medical conditions such as autoimmune diseases.
We had calculation of topical steroid application.
Questions were very straightforward and to the point .
Iontophoresis with viva Questions and answers
👉What is iontophoresis?
Iontophoresis is a procedure in which an electrical current is passed through skin soaked in tap water (not distilled water), normal saline (0.9%), or a solution containing an anticholinergic medication, which allows ionised (charged) particles to cross the normal skin barrier.
It reduces sweating and enhances the delivery of drugs and macromolecules into and through the skin. It is safe, effective and inexpensive
👉What is iontophoresis used for?
The main use of iontophoresis is to treat focal areas of excessive sweating (hyperhidrosis), particularly on the palms or soles
Iontophoresis has also been successfully used to deliver drugs to the skin in order to:
>Reduce sweating further using an anticholinergic agent such as glycopyrronium or botulinum toxin A.
>Anaesthetise an area of skin with lignocaine.
>Treat fungal infection of the nail plate (onychomycosis).
>Eradicate infection due to resistant micro-organisms using silver ions
>Treat bursitis or tendonitis with anti-inflammatory drugs
👉How does iontophoresis work in hyperhidrosis?
>Ions produced by iontophoresis may physically block the sweat ducts in the stratum corneum.
>The external electrical current may disrupt normal sympathetic nerve transmission.
>The pH drops in the sweat gland due to an accumulation of hydrogen ions.
>Iontophoresis for hyperhidrosis is usually carried out with ordinary tap water, however, sodium chloride electrolyte solution or an anticholinergic agent such as glycopyrronium bromide) can be added if the water alone is not effective.
👉Session frequency?
treatment is undertaken for 20–30 minutes every 1–3 days until the desired effect is achieved, and then reduced to once per week to maintain the result
👉Contraindications to iontophoresis?
>A patient who is epileptic or has a history of seizures
>A patient with a heart condition or a pacemaker
>A patient with a metal implant
>A pregnant woman.
recent wound, skin graft, or scar in the area requiring treatment
Also note few questions that can be asked .
🛑drugs can be delivered through iontophoresis?*
📍Reduce sweating further using an anticholinergic agent such as glycopyrronium or botulinum toxin A.
📍Anaesthetise an area of skin with lignocaine.
📍Treat fungal infection of the nail plate (onychomycosis).
📍Eradicate infection due to resistant micro-organisms using silver ions
📍Treat bursitis or tendonitis with anti-inflammatory drugs.
🛑advantages of iontophoresis over botox?*
📍It is a simple and painless treatment
📍A cheaper alternative to continuous injection treatments
📍Avoids muscle weakness as a side effect of botox
📍 Good for those having a fear of needles and surgery and who dont want to travel often for treatment
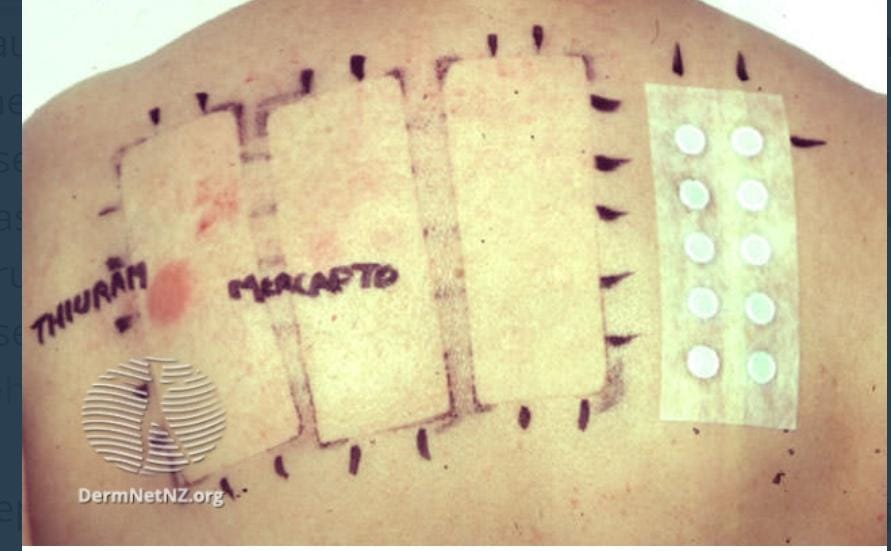
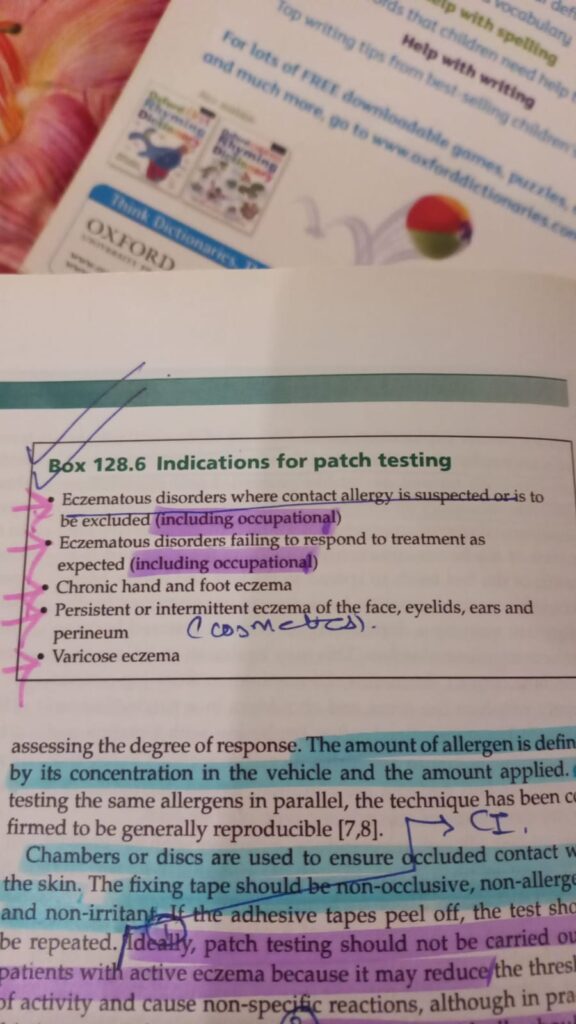
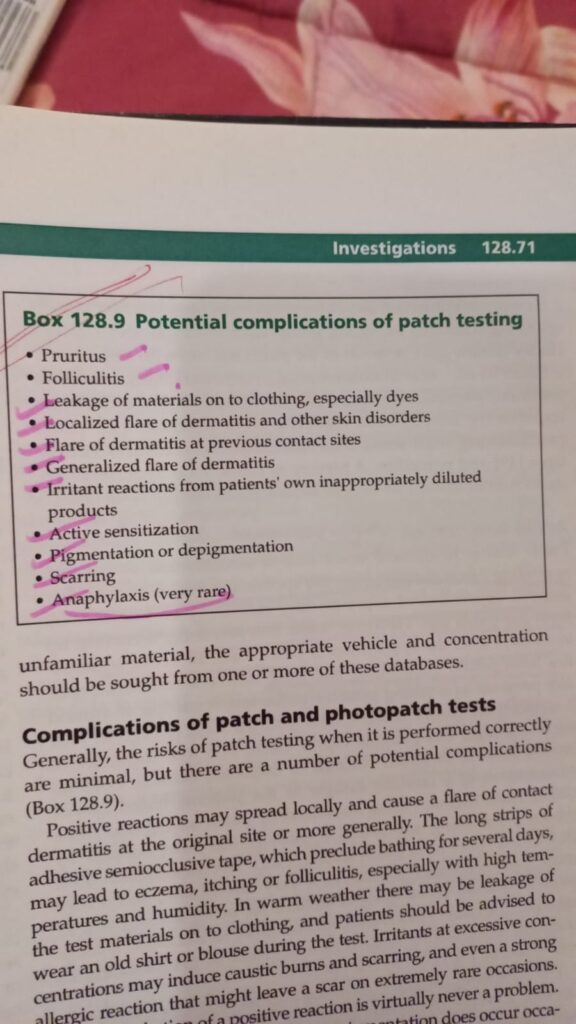
Perform _patch test_ with viva questions and answers
Viva Questions..
Q1) For how much time Sun-exposure should be avoided before patch testing ?
Ans: 4 weeks
Q2) Which allergen develop skin reaction later than 4 days after patch test?
Ans: Neomycin , tixocortol-pivalate, nickel.
Q3) What other sites of the body can be used to perform patch testing ?
Ans: Arms , fire arms , thighs and abdomen.
Q4) what are different types of chambers used for patch testing ?
Ans: Most commonly used is traditional round aluminium Finn chambers ( Epitest )
Others are squaric IQ ultra chambers made of soft polyethylene foam and T. R.U. E test.
Q5) Diffrent types of vehicles used for patch testing
Ans: white petrolatum , water are most commonly used, others are olive oil , rape oil , acetone , alcohol.
Q6) Withdrawal of patch test duration
Ans : 48 hours
Q7) What is angry back phenomenon?
Ans: Two or more positive results which are not reproduced when patient is retested also known as excited skin syndrome.
Q8) What is compound allergy ?
Ans : The condition in which patient is tested using a finished product generally cosmetics and topical drugs , obtaining positive results
However , when applied individually test results are negative.
Q9) what is quenching ?
Ans : It occurs due to potentiation of combination of allergic and irritant response e.g fragrances.
Q10) Strong positive result in patch testing is interpreted as?
Ans : Formation of papulovesicles , blisters or ulcers on allergen site..
U should give the pt time and date to cm and should ask them to wear loose clothes preferably front sided buttoned, dark coloured clothes. U should ask them to stop so n so drugs this much time before the test explaining when to stop oral or topicals as u mentioned, and to avoid exposure to sunlight. U should tell them that if the chamber falls off at home and u cannot cm atf that time, note the timings and cm to the hospital next morning.








PATCH TESTING
PHOTOPATCH TESTING👇🏻

🔰 IMPORTANT NOTE
The above given station is very imp and has come in toacs twice or thrice. So prepare it really well
Procedure
- The skin is cleansed with 70% alcohol and air-dried or wiped dry with cotton.
- A fold of skin is made relatively avascular by pinching or mild clamping. If the skin cannot be grasped by pinching, it can be compressed.
- An incision 3-5 mm long and 2-3 mm deep is made with a alcohol cleansed, single-edged razor blade. A scalpel with a #15 Bard-Parker blade may also be used. Mild pressure to maintain relative avascularity is continuously applied to the area until an adequate smear has been obtained.
- A small amount of blood does not interfere with the reading, but large amounts should be avoided and can usually be controlled by the amount of pressure of the pinch. If excessive bleeding occurs, it can be wiped away with a cotton swab.
- After the incision is made, and before the blade is withdrawn, the inner surface of the wound is scraped with the blade held at a right angle to the incision. Upon scraping, tissue fluid and dermal tissue are obtained.
- The material is transferred to the cleaned microscope slide. A moderately thick smear, with a visible uniform opacity is made. The smear is made in a circular manner on the slide, no larger than a pencil eraser (5-7 mm) , beginning peripherally and ending in the center, leaving a central “button” (2-4 mm) which can be easily focused upon with the microscope. Slides should be properly labeled as shown below in the sample diagram for 3 routine sites.
- A Band-Aid is generally sufficient to protect the smear site.
Staining of Skin Smears
- Dry the slide with smear at room temperature. DO NOT HEAT FIX.
- Place slides on a staining rack and flood with 10% formalin for 15 minutes for fixation.
- Gently rinse well with tap water. All formalin must be removed to prevent the formation of precipitates.
- Flood slides with Ziehl-Neelsen carbol-fuchsin for twenty minutes. The carbol-fuchsin must be filtered before each use.
- gently rinse slides well with tap water to remove excess stain.
- Decolorize with 2% acid alcohol for 1 minute.
- Gently rinse slides thoroughly with tap water.
- Counterstain with alkaline methylene blue for 30 seconds to 1 minute.
- Gently rinse well with tap water and air dry.
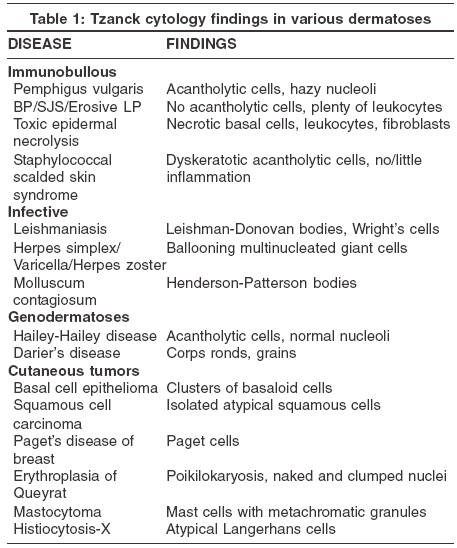
🛑🛑🛑viva questions
💥Other than leprosy slit skin smear can be used in which condition?
Cutaneous Leishmaniasis
💥Which stain is used in slit skin smear?
Ziehl-Neelsen method. Stain with 1% carbol fuchsin, which colours everything red. Wash out the stain with 1% acid-alcohol, which removes the stain from everything except M. leprae.
💥 What is bacteriological index?
It is quantification of Lepra bacilli in the patient
1+ 1-10 bacilli in 100 fields
2+ 1-10 bacilli in 10 fields
3+ 1-10 bacilli in 1 field
4+ 10-100 bacilli in 1 field
5+ 100-1000 bacilli in 1 field
6+ > 1000 bacilli in 1 field
💥What is Morphological index?
It is measure of solid staining M. Leprae that are viable. Fragmented and Granular bacteria are non viable.
💥which index is used to assess response to treatment?
Morphological index
💥What will be the bacteriological index in a case of tuberculoid leprosy?
it will be zero.
💥What is other name for Modified ZN stain?
Fite Stain
Rule out any contraindications like antiplatetes
Sites sampled in our step up are: Both ears lobules, both eye brows, left middle finger and active lesion
Slide should be labelled after making smear..
*Viva questions & Answers*
Occipital block
*Course of Occipital Nerve*
✅The greater occipital nerve: this originates from the posterior ramus of the spinal nerve, C2. It pierces the fascia under the superior nuchal ridge and emerges on the superior nuchal line along with the occipital artery. It can be located about one-third of the dis- tance along a line drawn from the occipital protuberance to the mastoid process.
✅The lesser occipital nerve: this arises from the sec- ond and third cervical nerves. It courses superiorly at the posterior region of the sternocleidomastoid
✅Indications of Occipital nerve block?
– Cervicogenic headache
– Occipital headache
– Anesthesia for posterior scalp procedure ( Scalp Prp)
– Migraine
✅Contraindications of occipital nerve block?
– Posterior fossa intracranial surgery
– Recent trauma
– Allergy to lidocaine/Bupivacaine
– Active infection at injection site
– History of Fits
✅what is the safe dose of lidocaine for an individual?
Ans: adult=4.5mg/kg plain…7mg/kg mixed with adrenaline
Paediatric and old age dose is half the adult dose.
✅what are 2 groups of local anesthetic?
ester and amide
✅which one is better?
Amide,lesser side effects and hypersensitivity
✅What is absolute contraindication to local anesthesia
history of hypersensitivity reaction or local infection at the site of infection
✅What is lidocaine toxicity?
Early: diplopia,tinnitus, lightheadedness, nausea, circumoral pallor, vomiting
mid: slurred speech, muscle twitching, tremors, seizures
late: apnea, coma, bradycardia, AV block, hypotension, arrythmia, hypoxia
✅How do u treat?
Early: recognize and observe
Mid: observe, oxygen, diazepam for seizures
Late: ACLS protocol
✅Alternative to local anesthetic?
normal saline or 10-25 mg/ml diphenhydramine
✅What is the gauge of needle used for occipital nerve block?
23 gauge and 25 gauge
✅ Amount of anaesthesia per nerve that can be given.
2 to 4cc
✅ Direction of needle?
It is directed upwards until periosteum is reached
✅ Location of Greater occipital nerve in relation to occipital artery?
It is medial to to occipital Artery.
🔵Needle size gauge 23 to 25 gauge needle used mostly for occiptal nerve block
🔵Amount of anesthesia per nerve should be known 2 to 4cc can be given
🔵Direction of needle should be known ..
It should be perpendicular to skull
🔵Post procedure care should be told as it is important
▪️After procedure patient should stay in procedure room for 20 to 30 min
▪️Its better not to drive home by himself as dizziness can occur
▪️Should not rub treated are or apply any irritant oil etc to treated area.
🔵Needle size gauge 23 to 25 gauge needle used mostly for occiptal nerve block
🔵Amount of anesthesia per nerve should be known 2 to 4cc can be given
🔵Direction of needle should be known ..
It should be perpendicular to skull
🔵Post procedure care should be told as it is important
▪️After procedure patient should stay in procedure room for 20 to 30 min
▪️Its better not to drive home by himself as dizziness can occur
▪️Should not rub treated are or apply any irritant oil etc to treated area.
*Viva questions & Answers*
Occipital block
*Course of Occipital Nerve*
✅The greater occipital nerve: this originates from the posterior ramus of the spinal nerve, C2. It pierces the fascia under the superior nuchal ridge and emerges on the superior nuchal line along with the occipital artery. It can be located about one-third of the dis- tance along a line drawn from the occipital protuberance to the mastoid process.
✅The lesser occipital nerve: this arises from the sec- ond and third cervical nerves. It courses superiorly at the posterior region of the sternocleidomastoid
✅Indications of Occipital nerve block?
– Cervicogenic headache
– Occipital headache
– Anesthesia for posterior scalp procedure ( Scalp Prp)
– Migraine
✅Contraindications of occipital nerve block?
– Posterior fossa intracranial surgery
– Recent trauma
– Allergy to lidocaine/Bupivacaine
– Active infection at injection site
– History of Fits
✅what is the safe dose of lidocaine for an individual?
Ans: adult=4.5mg/kg plain…7mg/kg mixed with adrenaline
Paediatric and old age dose is half the adult dose.
✅what are 2 groups of local anesthetic?
ester and amide
✅which one is better?
Amide,lesser side effects and hypersensitivity
✅What is absolute contraindication to local anesthesia
history of hypersensitivity reaction or local infection at the site of infection
✅What is lidocaine toxicity?
Early: diplopia,tinnitus, lightheadedness, nausea, circumoral pallor, vomiting
mid: slurred speech, muscle twitching, tremors, seizures
late: apnea, coma, bradycardia, AV block, hypotension, arrythmia, hypoxia
✅How do u treat?
Early: recognize and observe
Mid: observe, oxygen, diazepam for seizures
Late: ACLS protocol
✅Alternative to local anesthetic?
normal saline or 10-25 mg/ml diphenhydramine
✅What is the gauge of needle used for occipital nerve block?
23 gauge and 25 gauge
✅ Amount of anaesthesia per nerve that can be given.
2 to 4cc
✅ Direction of needle?
It is directed upwards until periosteum is reached
✅ Location of Greater occipital nerve in relation to occipital artery?
It is medial to to occipital Artery.
Viva questions
Occipital block
*Course of Occipital Nerve*
✅The greater occipital nerve: this originates from the posterior ramus of the spinal nerve, C2. It pierces the fascia under the superior nuchal ridge and emerges on the superior nuchal line along with the occipital artery. It can be located about one-third of the dis- tance along a line drawn from the occipital protuberance to the mastoid process.
✅The lesser occipital nerve: this arises from the sec- ond and third cervical nerves. It courses superiorly at the posterior region of the sternocleidomastoid
✅Indications of Occipital nerve block?
– Cervicogenic headache
– Occipital headache
– Anesthesia for posterior scalp procedure
✅Contraindications of occipital nerve block?
– Posterior fossa intracranial surgery
– Recent trauma
– Allergy to lidocaine/Bupivacaine
✅what is the safe dose of lidocaine for an individual?
Ans: adult=4.5mg/kg plain…7mg/kg mixed with adrenaline
Paediatric and old age dose is half the adult dose.
✅what are 2 groups of local anesthetic?
ester and amide
✅which one is better?
Amide,lesser side effects and hypersensitivity
✅What is absolute contraindication to local anesthesia
history of hypersensitivity reaction or local infection at the site of infection
✅What is lidocaine toxicity?
Early: diplopia,tinnitus, lightheadedness, nausea, circumoral pallor, vomiting
mid: slurred speech, muscle twitching, tremors, seizures
late: apnea, coma, bradycardia, AV block, hypotension, arrythmia, hypoxia
✅How do u treat?
Early: recognize and observe
Mid: observe, oxygen, diazepam for seizures
Late: ACLS protocol
✅Alternative to local anesthetic?
normal saline or 10-25 mg/ml diphenhydramine
🔶Needle size gauge can be asked in exam too 23 to 25 gauge needle used mostly for occiptal nerve block
🔶Amount of anesthesia per nerve should be known 2 to 4cc can be given
🔶Direction of needle should be known ..
It should be perpendicular to skull
🔶Post procedure care should be told as it is important
▪️After procedure patient should stay in procedure room for 20 to 30 min
▪️Its better not to drive home by himself as dizziness can occur
▪️Should not rub treated are or apply any irritant oil etc to treated area.
you all should have fine knowledge about landmarks and how to draw a line and points of nerve block
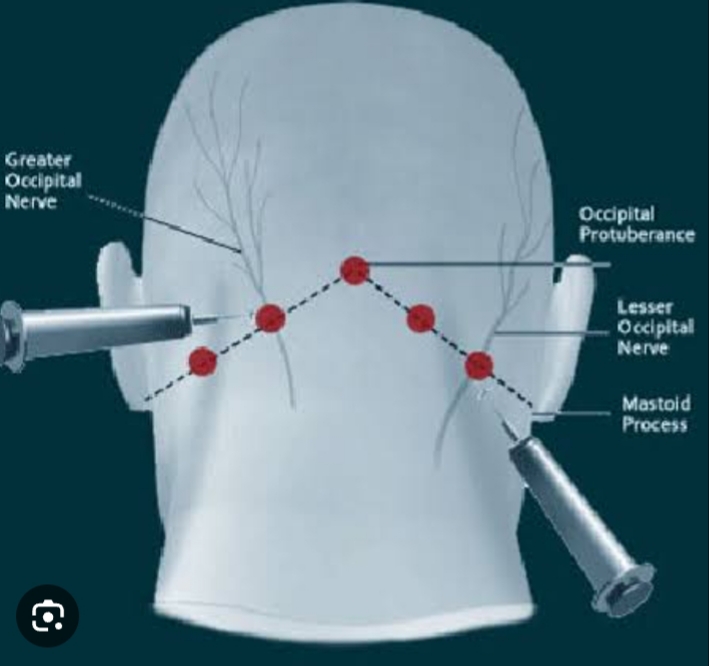
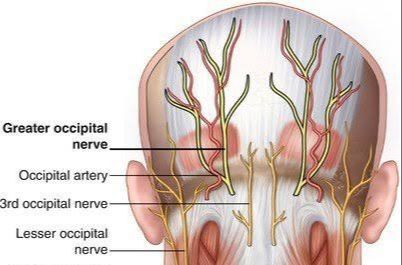
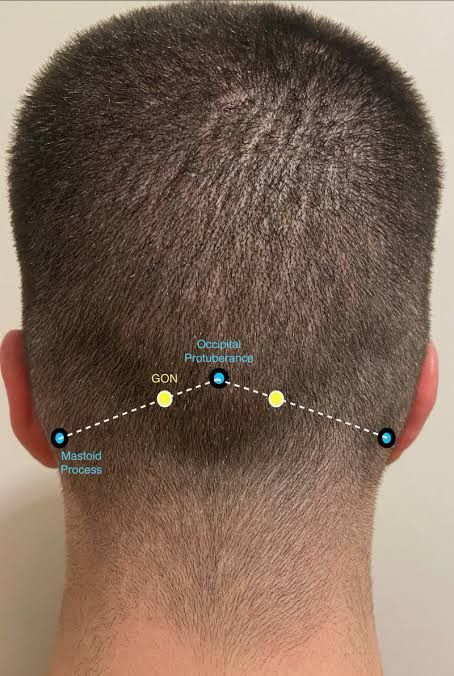

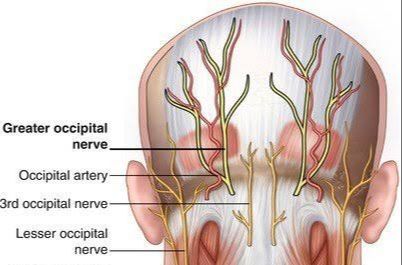
4 months old child presented with multilobulated violaceous to hemorrhagic nodular plaque on right side of forehead just above right eye. Lesion was in form of small papule on birth and now increased in size to 1.5*2cm. Mother also gives history of bleeding on trauma. How will you manage this patient?
🟥INFANTILE HEMANGIOMA TREATMENT ( by sir irfan)
*1* .Take normal saline or distilled water in a 10 ml syringe…
*2* . put a *10mg* crushed tab in it after removing the plunger and mix it well…
*3.* now you have got *1mg/ml* suspension ready..
*4.* Now according to weight of child you can directly dispense medicine after removing thr needle part….
*5.* discard the rest at the end of the day…
*6.* Daily prepare fresh suspension and shake well before use
If pt cant afford to get it dispensed . Its always better to get it dispensed
_*_DOSING*__
– *Initial 0-5-1mg/kg/ day* in 2-3 divided doses
*then doubling* of the dose every 3-7 days in _outpatient_ or every 1-3 doses in _inpatient_ til it reaches *2mg/kg/day*
– *For proliferating heamangioma*
treatment is till *9-15 months*
Dose should be tapered during intercurrent infections or vomiting
– *Taper over 2-4 weeks* befre stopping to prevent tachycardia
*Prednisolone suspension* is available I believe
If not then get it too from pharmacy at 1mg/ml
*Make it simple for“` urself~ .*_*
**1 mg / kg / days*
*And after 2 weeks *2mg /kg*
*1.* Outpatient propanolo initiation with assessing heart rate blood glucose and bp- whenever there is dose escalation and every 3-6 weeks when on a stable dose
*2* . pls remember Signs of hypoglycaemia-
..Early- sweating, rapid rate, shakiness
..late- poor feeding, hypothermia , seizures
*3.* Its better Feed the infant before each dose and 3-4 hours in young infants and 5 hourly in older infants
*4* . Addition of prednisolone avoid hypoglycemia
*Timolol drops is tds* , and u have to tapper steroids (0.5mg/kg/day) after three months to stop it after 6 months
🟥Mechanism of action of Propranolol
▪️Induction of vasoconstriction and decreased expression of angiogenic factors
🟥Monitoring for Propranolol
▪️BP and heart rate
▪️Blood sugar level
▪️ECG and Echo
🟥Classification of infantile hemangiomas
▪️Superficial
▪️Deep
▪️Mixed(Superficial and deep)
▪️Reticular, abortive or minimal growth
🟥Patterns of infantile hemangiomas
▪️Focal
▪️Multifocal
▪️Segmental
▪️Indeterminate
🟥Risk factors for infantile hemangiomas
▪️Girls
▪️Amniocentesis
▪️Breech presentation
▪️In vitro fertilisation
▪️First born
▪️Low birth weight <2500g
🟥Complications
▪️Ulceration
▪️Disfigurement
▪️Functional impairment
https://youtu.be/O_mktNYshLA?si=y86nTS2KDrxr3l_G
- Topical Propranolol 1% twice daily can also be used for superficial hemangioma but topical timolol is more effective.
- Besides beta blockers and Steroids, Other rx options for infantile hemangioma are PDL and surgery
- Although β-blockers may be helpful for the treatment of ulcerated infantile haemangioma, worsening of ulceration can occur, perhaps reflecting reduced blood flow.
- Patients with segmental IH and suspected PHACES syndrom ideally require MRA before starting propranolol – if not possible to obtain urgent MRA, start propranolol 0.5 mg/kg daily in 3 divided doses
- Dose of Propranolol and vitals montiroing interval also can be acc to weight of pt. Pic attached.
- Infantile hemangioma are different from vascular malformations on the basis of…. pic attached.
- Photograph of the lesion and size should be measured on start of rx and would be rechecked on every visit.
But if hemangioma is close to the eye,effecting vision..like functional impairment then there is indication of surgery.
Pdl laser is use for ulcerated hemangioma and also for telangiectases post involution
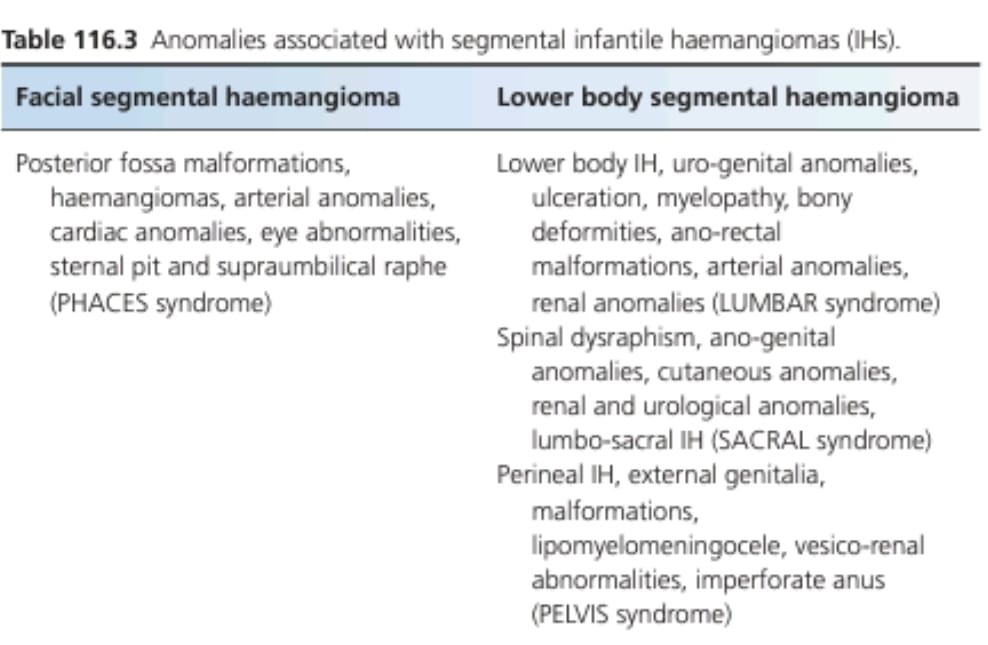

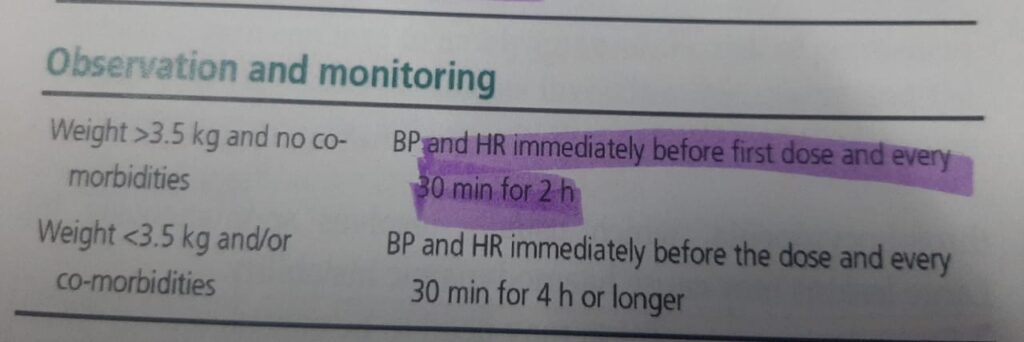
While doing filler the outline(vermilion border)and body of the lip both should be filled ..
We can use vertical line to fill the body it helps in everting the lip abit and the dot technique just give filling without eversion
♦️Non surgical lip augmentation techniques
Filler
Lip flip with botox
♦️ Indications
- Age related loss of volume
- To correct asymmetry
- To increase fullness of lips
- To enhance the shape (create more defined cupid bow)
♦️Complications
- Scarring
- Itching
- Asymmetrical lips
- Lumpy irregular lips
- Allergic reaction

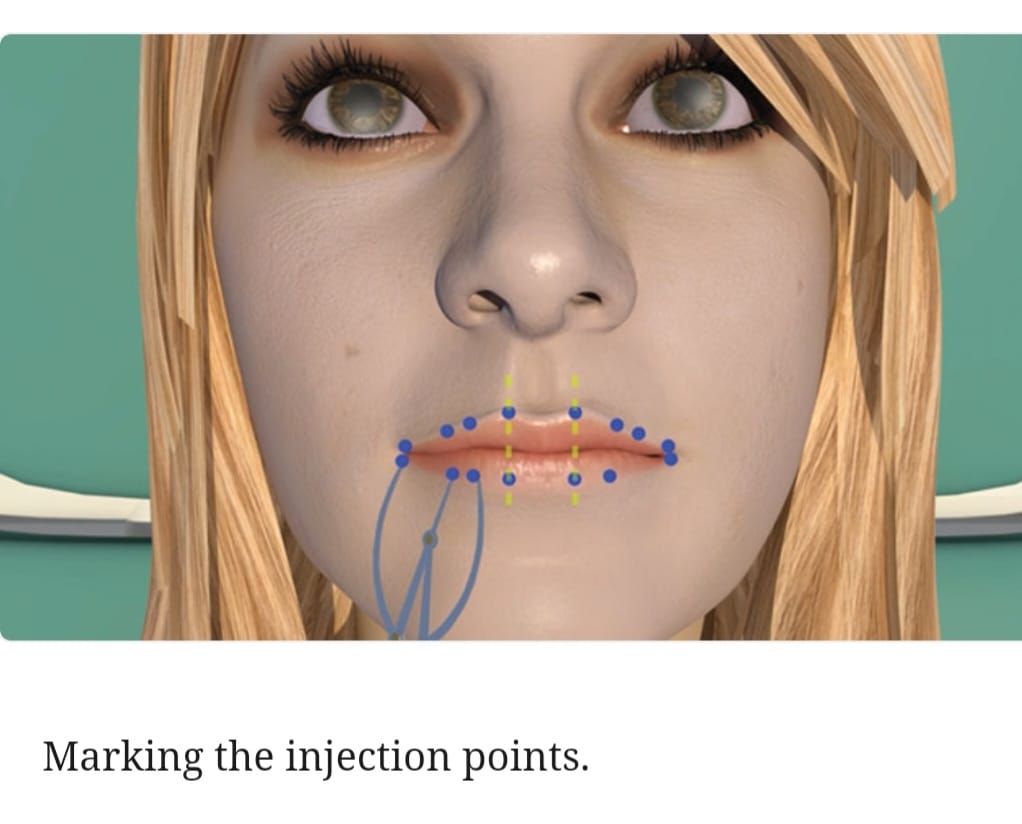
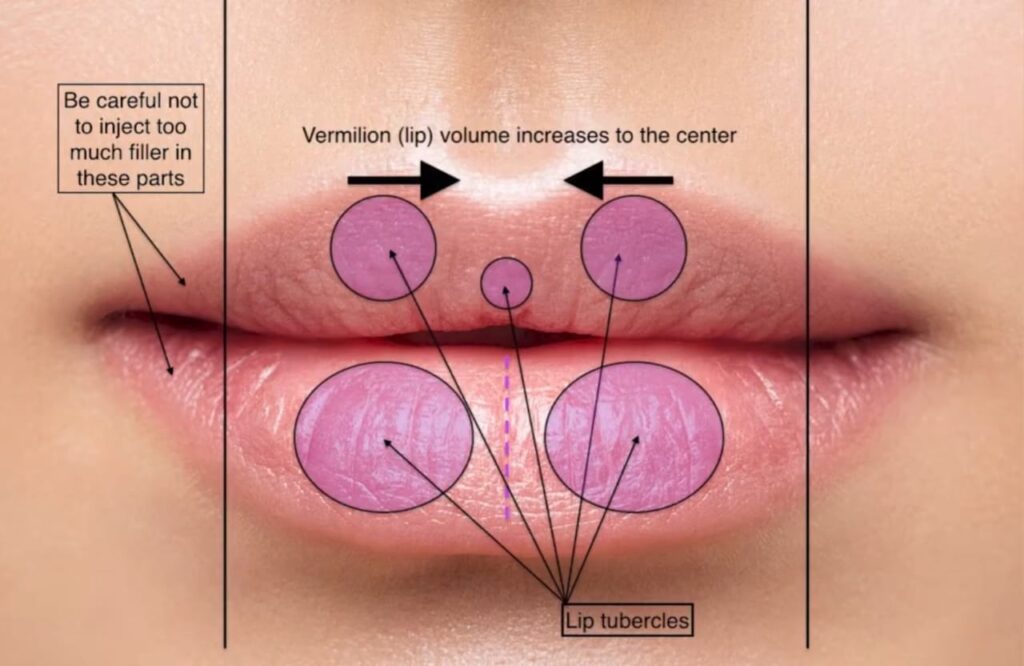
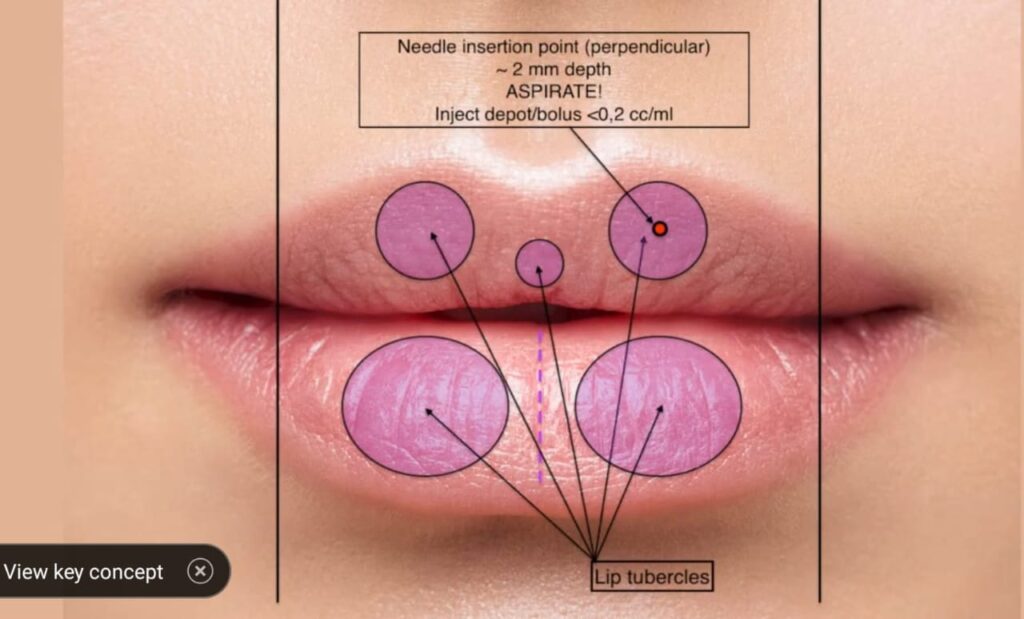
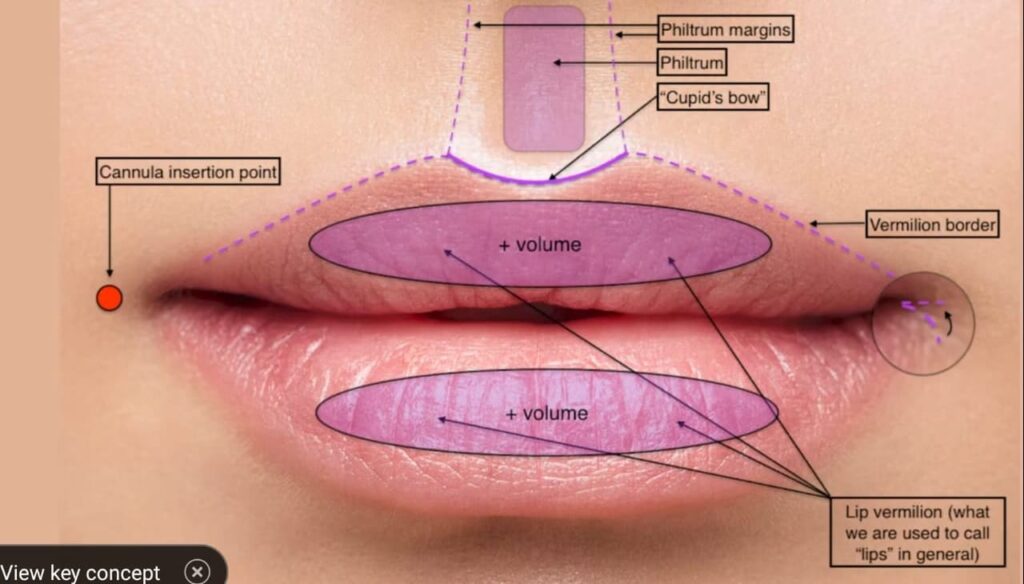
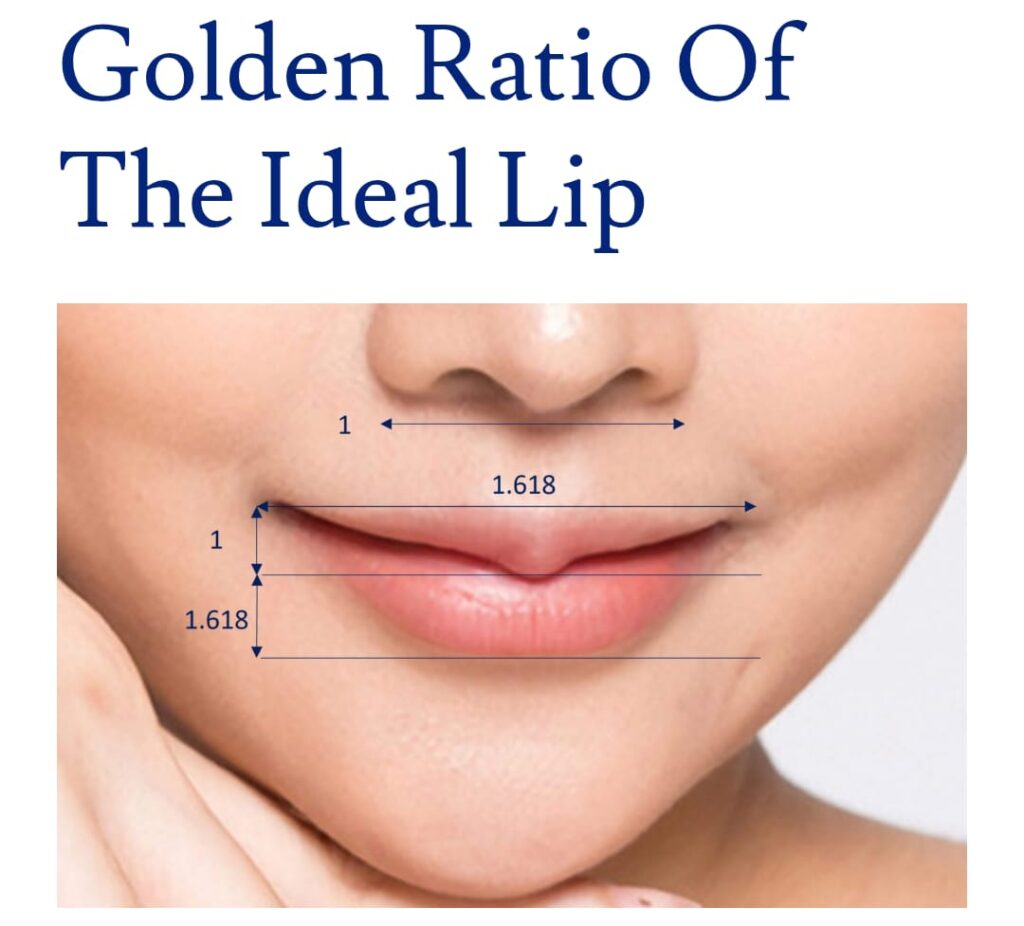
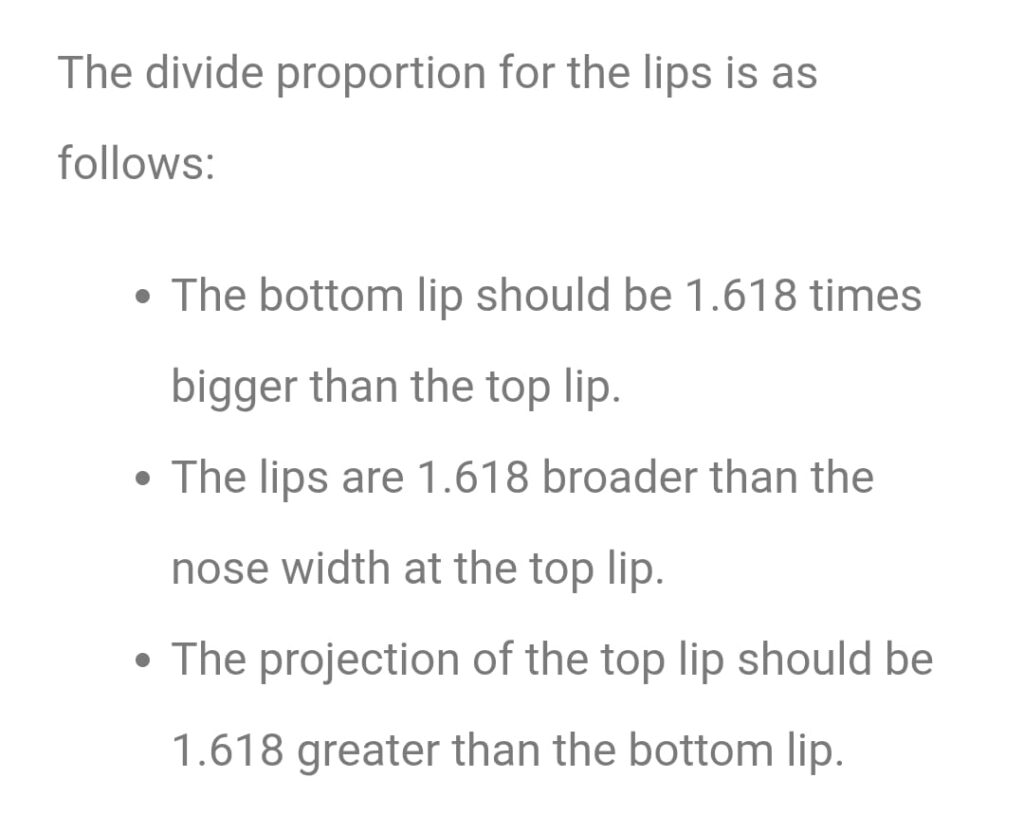

Q1.A 30 years soldiers presented with recurrent Ingrowing toe nail.How will you proceed?
Q.2A 37 year old man presented with toe nail onychomycosis. Already treated with oral antifungal multiple time.
What is next line of action?
🟥Nail AVULSION 🟥
🛑NAIL AVULSION 🛑
📗 NAIL ANATOMY::
📝 Nail has 3 borders
✅ Distal border….free
✅ Proximal border…clutched into fold & covered with skin flap Called EPONYCHIUM/CUTCLE
✅ Lateral border…also attached
📝 MATRIX….
✅ Distal sterile matrix…..NAIL BED
✅intermediate matrix….epithelial lining of ventral surface of PNF
✅ Distal terminal matrix….new nail arise from here
Germinal matrix is covered with Eponychium
🟥WHAT ARE INDICATIONS OF SURGICAL NAIL AVULSION ?
🟢 DIAGNOSTIC::
📍Exploration of NAIL bed & nail matrix .
📍Exploration of proximal nail fold (PNF) & lateral nail fold.
📍Performing biopsy on nail bed and nail biopsy
🟢 THERAPEUTICS::
📍Before chemical and surgical matricectomy
📍Ingrowing toe nail ( onychocryptosis)
📍Chronic onychomycosis
📍Traumatic nail injuries
📍Chronic paronychia
📍Retronychioa
📍Pincer nails ( Omega nails / Trumpet nails)
📍Warts
📍Tumors
🟥 WHAT ARE CONTRAINDICATIONS OF SURGICAL NAIL AVULSION?
📍Peripheral vascular disease
📍Collagen vascular disease
📍Diabetes mellitus
📍Disorders of hemostasis
📍Acute infection and inflammation of nail unit
🟥WHAT ARE COMPLICATIONS OF SURGICAL NAIL AVULSION
📍Pain
📍Swelling
📍Infection
📍Hematoma
📍Allergy to anesthesia
📍Minor wound discharge
📍Nail deformity
📍Malalignment
📍Nail impaction ( distal embedding)
📍Local spicule growth
🟥WHAT ARE TYPES OF SURGICAL NAIL AVULSION 🟥
✅ Distal & proximal avulsion
✅ Partial / Complete avulsion
🔴WHICH ANASTHESIA IS PREFERRED🔴
💊 perform digital block with 1% lidocaine
💊 Epinephrine should be avoided especially in
🖊️ Uncontrol Hypertension
🖊️ Extensive Vascular disease
🖊️ Thrombotic/ vasospastic disease
🛑HOW WOULD YOU PERFORM SURGICAL NAIL AVULSION? 🛑
🟥Complete Surgical nail avulsion 🟥
Carried out by
🟢 Distal approach
🟢 Proximal approach
🟥 DISTAL APPROACH 🟥
💊 An elevator is gently slid under the proximal nail fold in a backand-forth motion from side to side
💊 Avoiding injuring the fragile longitudinal nail bed ridges, until the proximal nail fold is freed from the nail plate
💊The elevator is then pushed under the nail plate from the distal free edge until the elevator gives way (meaning the elevator has reached the matrix area to which the nail plate is loosely attached)
💊 Caution must be taken to detach the lateral horns of the nail plate fully.
💊A jaw of a sturdy haemostat is slid under the whole length of a lateral portion of the nail plate and grasped firmly
💊In an upward rotating motion, the nail plate is avulse
🟥PROXIMAL APPROACH 🟥
💊proximal approach is advised when the distal subungual area strongly adheres to the nail plate (e.g. thick hyperkeratosis) & dificult to find a cleavage plane between the plate and the bed.
💊The proximal nail fold is detached as described above
💊The elevator then relects the proximal nail fold and is delicately inserted under the base of the nail plate where the adherence to the matrix is weak.
💊The procedure is repeated along the whole width of the nail root
💊 The avulsion progresses distally following the natural cleavage plane up to the hyponychium
🟥PARTIAL SURGICAL NAIL AVULSION 🟥
Advantage of this technique is that it leaves a large portion of normal nail plate that still exerts a pressure on the underlying soft tissues, reducing the risk of distal embedding
💊 used for treatment of some types of onychomycosis (longitudinal streaks, lateral disease, dermatophytoma, onychomycosis due to moulds)
💊Partial nail avulsion is part of many surgical procedures:
✅Chemical cautery of a part of the matrix in ingrowing toenails
✅ treatment of acute paronychia
✅ Surgical exploration of any nail bed or matrix tumour
💊 Performed in the same way as the distal approach method of total surgical nail avulsion but is restricted to a limited portion of the nail plate
💊For exposure of the matrix area, avulsion of the proximal third of the nail plate is best
💊It starts with two lateral incisions on the proximal nail fold at 45∘ enabling it to be relected
💊A jaw of a nail splitter is inserted under the lateral border of the nail plate, approximately 5 mm distal to the lunula
💊The plate is cut horizontally to the other side
💊 A haemostat grasps the lateral portion of the plate and lifts it up laterally, as for a sardine tin, exposing the whole matrix area
💊After surgery, the plate is laid back in place and sutured to the lateral fold
🟥POSTOPERATIVE CARE🟥
✅non- adherent, highly absoable dressing is ideal
✅kept in place with elastoplast/ paper tape
✅Lateral groove must studded with paraffin gauze/ antibiotic tulle
✅Dressing remove after 24 hrs after soaking in warm water & Saline
✅Apply povidone- iodine solution to promote healing
✅keep operated limb elevated to decrease pain & swelling
✅Do minimum activity for 2 weeks of affected site
🔴diagnostically nail avulsion is done for different inflammatory dermatosis like LP , PSORIASIS , CT diseases and infections
🔴To confirm certain nail unit tumors and malignancy if there is clinically longitudinal melanonychia .
🔴Therapeutically it is also done if there is
🔴Chronic nail pain
🔴Retronychia
🔴And tumors .
🔵Normal nail growth :
finger nails grow in app 9 months and great toe nail in 18 months .
🔵Causes of slow growth rate are :
Poor nutrition
Kwashiorkor
Hypothyroidism
Yellow nil syndrome
Relapsing polychondritis
Drugs like metho , AZA
🔵 Faster growth rate causes are :
Psoriasis
PRP
Hyperthyroidism
Levodopa
Pregnancy
One method is chemical nail avulsion in which 40% urea ointmeis put directly on the bail bed and secured for a week..
Caution is to keep the dressing dry…
Secondly TCA is also use in place of phenol to destropy the matrix in partial nail avulsion…i was specifically ask this question in tocs by mam sadia tabassum


♦️half life of adalimumab
🔸 14 days
♦️ discontinue adalimumab before surgery — should be equal to 4 ×half life of that drug
🔸6-8 weeks
While 4-6 weeks for infliximab,2 weeks for etanercept
♦️Prerequisites before starting TNF alpha inhibitors*
CBC
screening for hepatitis B and C , tuberculosis and HIV
ELISA for hep B and C and IGRA testing, CXR and quantiferon gold test for TB
HIV by PCR
Give test dose of infliximab and check for any hypersensitivity reactions and if any then give prior to administration antihistamines prednisolone and acetinophen etc…
♦️Pregnancy and lactation safety
🔸Adalimumab, Etanercept, Infliximab all are category B and are also secreted in breat milk
Use during pregnancy and lactation should be avoided wherever possible
🔸Certolizumab lacks Fc portion, doesnt cross placenta and any effect on baby’s immune system is minimal
- Ask for H/O demyelinating disease (in person or family- Multiple sclerosis, optic neuritis)
- Ask for H/O active or past H/0 TB (in person or close contacts)
- Ask for H/O cardiac failure, malignancy or planned surgery
- Ask for H/O angioedema, anaphylaxis and drug allergies.
- Ask about live vaccinations
And About latent tuberculosis,
If patients with investigations suggestive of diagnosis of latent tuberculosis, treatment with ATT is indicated, patient should complete 2 months of tre before starting biologics. During treatment and after 6 months of discontinuation, high indices of suspicion should be maintained.
Its given by s/c route and if incase tb came positive or even igra latent tb tested positive then treat tb first then give biologics .
After stating biologics response should be achieved by 3 months if no response by 3 months stop biologics..maximum biologics are given for 6 months
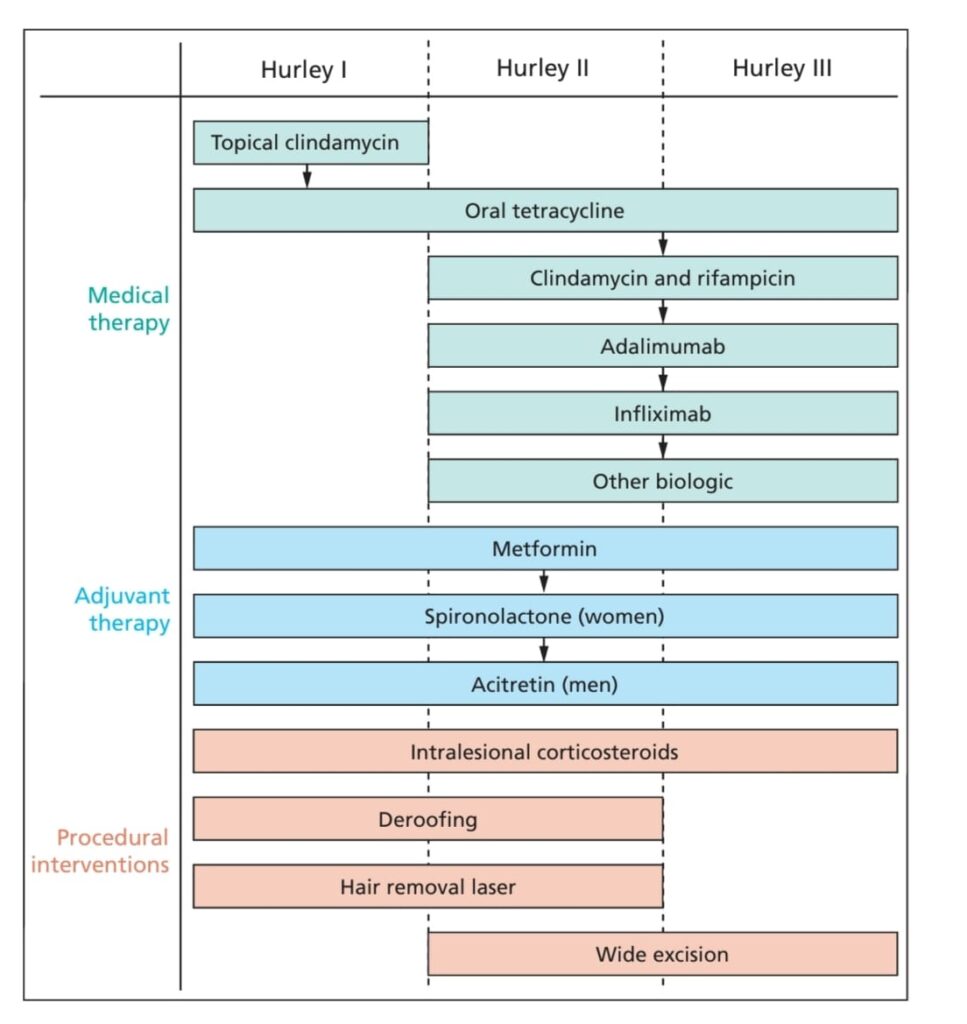
🔰 IMPORTANT NOTE👇🏻
Technique for Hyaluronidase injection following vascular occlusion over ala of nose:
Hyaluronidase is an endoglycosidase that breaks down hyaluronic acid into monosaccharides by cleaving its glycosidic bonds; additionally, to some extent, it also breaks down other acid mucopolysaccharides in the connective tissue
✍🏻In order for hyaluronidase to dissolve a hyaluronic acid filler, it must be able to access the intramolecular bonds within hyaluronic acid. The factors that interfere with access include the number of crosslinks between hyaluronic acid molecules and the concentration of hyaluronic acid. The more cross-linking, the more difficult it is for hyaluronidase to access its binding sites inside the hyaluronic acid filler. For this reason, fillers with extensive cross-linking require a long time to dissolve with hyaluronidase [12]. In addition, the higher the concentration of hyaluronic acid, the slower it will be dissolved by hyaluronidase
✍🏻Local injections of hyaluronidase can cause side effects such as local pruritus and allergic reactions. The incidence of allergic reactions is reported to be 0.05% to 0.69%, and urticaria and angioedema have also been reported to occur at a low frequency (less than 0.1%)
✍🏻A occlusion is a potentially severe adverse outcome that can occur when hyaluronic acid filler is accidentally injected into a blood vessel.
If a vascular occlusion is not promptly diagnosed and managed appropriately, tissue necrosis can ensue. Outcomes are all the more catastrophic when involving anastomotic connections between the external and internal carotid arteries; in these circumstances, blindness and stroke are both possible.
A vascular occlusion can cause a retinal infarction in 12 to 15 minutes.
✍🏻Mechanism of vascular occlusion:
Ischemia and its effects on tissue can give rise to vasospasm. When the tissue is ischemic, the vasospasm occurs because of desensitization to nitrous oxide. Combined with compression due to extravascular edema, changes in the surrounding tissue can be expected. Further, hyaluronic acid filler, when injected intravascularly, can act as a noxious stimulus, producing inflammation and further intense vasospasm.These secondary vascular changes will worsen the ischemia caused by the direct intravascular occlusion.
✍🏻It is possible that an embolic event in a distal (to the site of injection), narrower arteriole can cause delayed ischemic changes.
✍🏻The hygroscopic nature of the hyaluronic acid leads to an increase in bolus size, causing a more complete occlusion or compression in predisposed areas outside the vessel.
✍🏻The initial bolus might not be large enough to fully occlude the vessel. However, the vessel subsequently becomes occluded through platelet aggregation.
✍🏻Vascular occlusions might be immediately apparent or presentation might be delayed, sometimes presenting hours or even days after the treatment
Assessing capillary refill time. It is vital to assess the capillary refill time (CRT) along the distribution of the artery immediately after injection. It is advisable to allow 30 to 45 minutes to assess a patient after injection of high-risk areas, such as the nose, glabella, or forehead. The CRT—the amount of time needed for the blood in a peripheral area of the body to return after compression—must be checked on both sides of the corresponding region of the face and is considered normal if it is less than two seconds. A brisk CRT can indicate venous insufficiency.
Pain. Some discomfort during the procedure is normal. However, if local anesthetic has been used either in combination with the hyaluronic acid or injected separately, the pain can be masked until the anesthesia wears off. Sudden escalating pain during treatment either at the site of the injection or in a distant site is not normal. The injection should be stopped immediately and the tissue assessed.
Skin color. Skin color is an important marker of ischemic changes. The skin signs can be explained in Stages 1 to 5 (Figure 2A–2E) to assist in predicting whether a good recovery can be expected or if there is likely to be tissue breakdown and a wound that will require management. Once the blood supply has been interrupted or restricted, the tissue can appear pale or dusky. The pallor, or blanching, may be fleeting but will be replaced by a reticulated purple pattern as the deoxygenated blood in the tissue builds up
If an arterial occlusion is left untreated, the tissue will progress through the stages of ischemia. The extent of tissue damage is dependent upon the occlusion size, underlying anatomy, collateral supply, general vascular integrity, healing ability, and presence of infection.
It is important to state that antiplatelets do not dissolve established thrombus; rather, they reduce platelet clumping but do not stop coagulation.
STEPS TO MANAGING AN ESTABLISHED VASCULAR OCCLUSION
- Video the area in good light ensuring the capillary refill time is checked along the track to the affected artery.
- Disinfect the skin and mark out the whole area of ischemia.
- CMAC recommend reconstituting 1,500 units of hyaluronidase with 1ml bacteriostatic NaCl 0.9% or 1–2% lidocaine (or suitable alternative).
- Infiltrate 1,500 units by needle or cannula (if appropriate) over the course of the affected artery and the wider area of ischemia. Be prepared to use more than one vial at a time if the area affected is significant. It is important to achieve full coverage and focus less on the number of units used. Treat to effect.
- Apply heat, and massage the area vigorously to aid mechanical breakdown of the hyaluronic acid
- Reassess capillary refill time and compare with pre-hyaluronidase video. If CRT is still delayed >3 seconds, repeat.
CMAC does not recommend performing skin tests in the event of a vascular occlusion, as the risk of anaphylaxis is minimal and there is no recognized validated test concentration to accurately assess Type 1 hypersensitivity (See CMAC guideline for hyaluronidase).
✍🏻Good Practice Guidelines
✍🏻KNOWLEDGE OF INJECTION ANATOMY
Understand depth, distribution, and common variations of major vessels to guide safe injection plane.
✍🏻Extreme caution should be taken when injecting those with previous facial surgery, as this may have altered the anatomy.
✍🏻Caution should be applied when injecting areas where there is scar tissue or previous surgery.
✍🏻Technique
Inject slowly at a low pressure (this will limit how much may inadvertently enter a vessel, limit retrograde flow, and limit extent of ischemia).
✍🏻Consider using a cannula of 25 gauge or larger.1
✍🏻Inject in small increments per site to limit potential occlusion size.
✍🏻If aspirating, understand that this is not failsafe and even when done correctly, it is unreliable.
✍🏻Consider using targeted digital pressure to compress arterial pathways, particularly preventing retrograde filler movement.
✍🏻Do not use adrenaline with lidocaine as this may mask the blanching produced by occlusion.
⭕️In case of signs of vascular occlusion caused by HA filler inject hyaluronidase around the injected area and the course of affected artery.
⭕️
Hyaluronidase is effective only within the first 4 hours after injection .
⭕️ while injecting , the needle should be perpendicular to the skin and several injections are often necessary. ( a high dose pulsed large volume of hyaluronidase 450-1500 unit should be infiltrated) .
⭕️observe and reassess capillary refill after 60 minutes ; if there is still vascular compromise , repeat treatment at hourly interval for upto 4 cycles.
⭕️once the retinal artery has been occluded, there is a window period of90 minutes before blindness is irreversible. Retrobulbar injection of hyaluronidase ( 2000-5000) into infero- lateral orbit region is recommended in cae HA filler is used.
Pain and swelling is common in areas where filler is dissolved
https://www.sciencedirect.com/science/article/pii/S2212426824000629
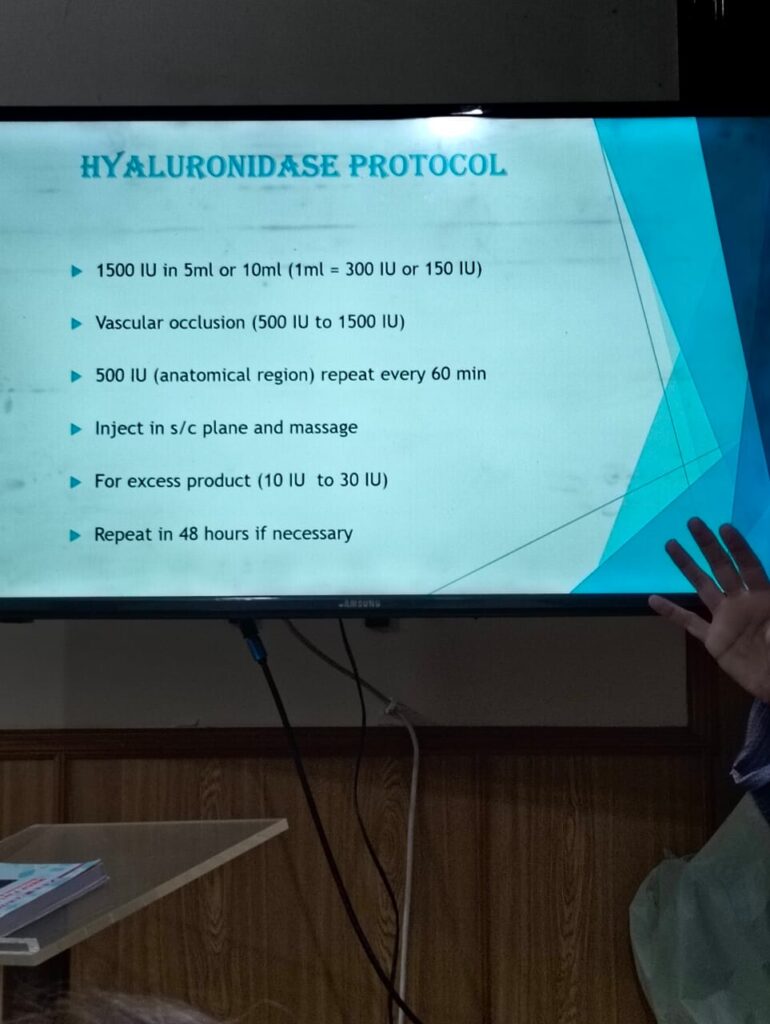


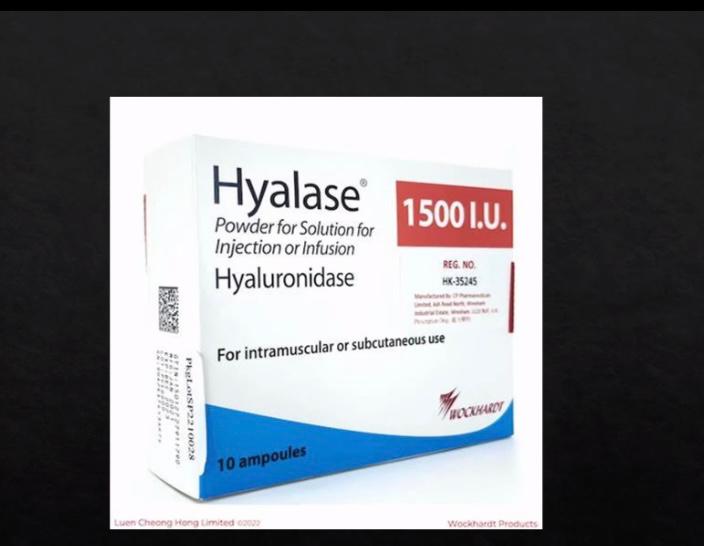



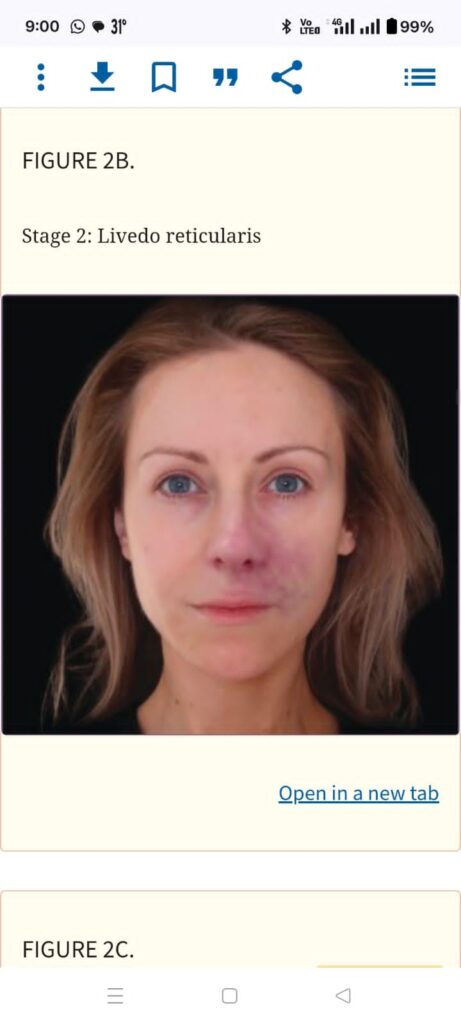
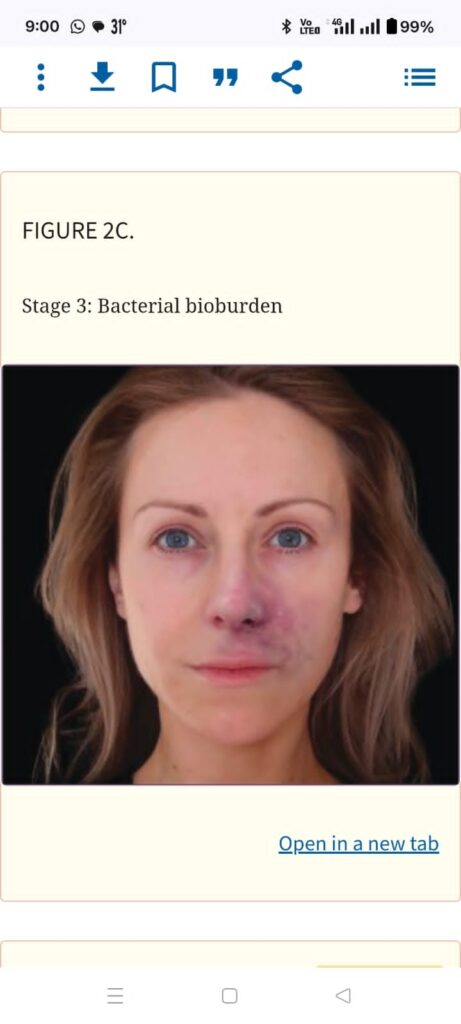


1️⃣ MOPHISTO SIGN
2️⃣ CROOKED SMILE
How to fix a crooked smile
3️⃣ BROW PTOSIS
https://youtube.com/shorts/fUb–UsNlzU?si=ywx6bmwWzyLdYl7F
*Tag biopsy specimen of BCC with viva Questions and Answers*
.*VIVA QUESTIONS*
🧠Why is tagging of BCC done?
Ans :To locate the medial, lateral ,upper and lower borders of the specimen
🧠If e.g at 3’O clock margin of biopsy sample is not clear on histopathology, what to do next ?
Ans: Re-excise at 3’O clock position.
🧠Non Surgical methods of BCC treatment
Ans 1.Curretage
2.Cauterization
3.CO2 ablation
- Cryotherapy
🧠Medical Rx options for BCC
Ans 1.5 flourouracil
2.topical imiquiomod
🧠Other options
Photodynamic therapy
🧠Indications of MMS:
- centrofacial ,including
periocular and ears
2.Morpheic
3.>5cm giant bcc
4.infiltrative and
micronodular
5.perineural and
perivascular involvemnt
6.immunosuppresion
7.Recurrent
8.Lymph node involvement
or distant mets
⚪ In my opinion the procedure should be explained to the pt in detail as well before taking consent and the purpose of doing it that is both diagnostic and therapeutic aswell as explain the plan for follow up.
⚪ A few other questions that can be asked are
◻️ vismodegib and its use?
It is an inhibitor of SMO used in treatment of locally advanced and metastatic bcc as well as NBCCS that cannot be treated by surgery or radiotherapy.
◻️When is radiotherapy considered ?
pt unwilling for surgery
unable to tolerate surgery
👉 palliative treatment in advanced bcc
◻️Features of high risk bcc on histology ?
infiltrative or mocronodular type
perineural perivascular involvement
🧠An elderly lady 65yrs of age presented to the opd with a nodule on her forehead that had a shiny surface and overlying telengiectasia.On iquiring her about its evolution she said it has increased in size over the last month.She was anxious and wanted to know if its cancerous. How will you proceed for a biopsy specimen and labelling.
🌼 Why is tagging of BCC done?
Ans :To locate the medial, lateral ,upper and lower borders of the specimen
🌼 If e.g at 12’O clock margin of biopsy sample is not clear on histopathology, what to do next ?
Ans: Re-excise at 12’O clock position.
🌼Treatment in metastatic and locally advanced BCCs?
Ans Vismodegib is given in metastatic and locally advanced BCCs.
🌼Histopathological patterns of BCC?
Ans: 1..Superficial
2..Nodular
3..Infiltrative
4..Micronodular
5..Pigmented
6..Morphea form
7..Basosquamous
🌼 Risk factors for BCC?
Ans: 1. Skin type 1 and 2
- Solar UV radiation
- Human papilloma virus
- Iatrogenic immunosuppression
- Acquired immunodeficiency syndrome and non-Hodgkin lymphoma
- PUVA therapy
- Photosensitizing drugs
- UVB therapy
- Ionizing radiation
- Occupational factors
- Arsenic exposure
- Previous history of BCC
🌼 Indications of MMS:
- Centro-facial ,including peri-ocular and ears.
- Morpheic
- >5cm giant bcc
- Infiltrative an micro-nodular
5.peri-neural and perivascular involvement
- Immunosuppression
- Recurrent
- Lymph node involvement or distant mets

*MOA of podophyllin?*
Podophyllin is a cytotoxic agent that has been used topically in the treatment of genital warts. It arrests mitosis in metaphase by inhibiting formation of microtubules, The active agent is podophyllotoxin.
*Difference between podophyllin and podophyllotoxin?*
Podophyllotoxin is standardised and stable, whereas podophyllin has a variable composition. In an open comparison of self applied podophyllotoxin 0.5% versus podophyllin 20% applied by a doctor to treat external penile warts, podophyllotoxin was more effective and gave quicker resolution than podophyllin.
Q#1🔲What is the causative organism of anogenital warts?
HPV types 6 and 11
Q#2🔲Mode of transmission other than sexual?
HPV is spread by direct skin-to-skin contact or any other contact involving the genital area (eg, hand-to-genital contact), also vertical transmission
Q#3🔲How to treat genital warts?
Various options to treat genital warts..
➡️Medical treatments —
🔸Podophyllin 0.15% twice daily for 3 days in a week for 4 weeks
🔸trichloroacetic acid
🔸Imiquimod 5% or 3.75% 3 times per week for 16 weeks
🔸interferon
➡️Surgical treatment —
🔸Cryotherapy (only therapy that is safe in pregnancy)
🔸Electrocautery
🔸Excision using Anaesthesia
🔸PDT
🔸Laser
Q#4🔲
GENITAL WARTS FOLLOW-UP…
Patient should be asked to come for follow up visits as orderd by physician and for next 3 – 6months after treatment as most of the warts come back within this time period..
Q#5🔲
GENITAL WARTS PREVENTION
HPV vaccine — Two vaccines, quadrivalent (commercial name Gardasil) and 9-valent (commercial name Gardasil 9), are available for prevention of genital warts.
Q#6🔲MECHANISM OF ACTION of Podophyllin?
🟠*Mechanism of Action*
▪️It inhibits the formation of microtubules.
◾️It also suppresses cellular nucleoside transport.
◾️cause the arrest of cells in metaphase of the cell cycle hence causes reduced cell division
Q#7🔲
How will we prepare the solution?
Podophyllum resin 25% topical solution USP prepared by mixing
25 grams of podophyllum resin in alcohol +10 grams of the alcohol-soluble extract of benzoin
and finally Add alcohol to make 100 ml.
Q#8🔲
Commercially available preparations??
🟠Preparations Available in pakistan are
🔸Podophyllin 25% solution in tincture benzoin
🔸25% podophyllin ointment
Or 🔸podophyllin 25gm in 100ml of tincture benzoin
Or
Podophyllum [Cream 0.15 %w/w]
Brand Name
WARTEC
GLAXOSMITHKLINE
Price /810
Other preparations used worlwide are
🔸Podofilox 0.5% gel.
🔸Cantharidin 1%, podophyllin 2%, salicylic acid 30% (CPS1) solution.
Q#9🔲
Indications for the use of podophyllin??
*Clinical Uses*
🟠Presently, podophyllin is used successfully for the topical treatment of anogenital warts. However, only Podofilox 0.5% gel has received FDA approval to be used in the treatment of anogenital warts.
🟠*List of various dermatoses where Podophyllin has been used*
🔸*Viral Infections*
Condyloma acuminata
Verruca vulgaris
Plantar and periungual warts
Molluscum contagiosum
🔸*Fungal Infections*
Tinea capitis
🔸*Benign Dermatoses*
Acanthosis nigricans
Black hairy tongue
Contact dermatitis
Lichen simplex chronicus
Pyogenic granuloma
Seborrheic keratosis
🔸*Premalignant*
*Dermatoses*
AK
Arsenical keratosis
Bowen’s disease
Keratoacanthoma
🔸**Malignant Dermatoses **
Bcc
Scc
Mycosis fungoides
🔲*Contraindications *
🔸Pregnancy
🔸Lactation
🔸Drug hypersensitivity
🟠important points
🔶it should be performed as an office procedure.
🔸do vaginal examination and proctoscopy also while examining the affected site
🔸The volume of the solution applied should be kept minimal (≤ 0.4–0.5 mL)
🔸The solution should be allowed to dry properly, and the initial test application should remain in place for 1 h, and then can be washed off.
🔸Alcoholic beverages, general anesthesia, and CNS depressants should not be used for several hours after treatment.
*Side effects*
*⚫️*Early symptoms of too much medicine being absorbed into the body**
Abdominal or stomach pain
clumsiness or unsteadiness
confusion
decreased or loss of reflexes
diarrhea (may be severe and continuing)
excitement, irritability, or nervousness
hallucinations (seeing, hearing, or feeling things that are not there)
muscle weakness
nausea or vomiting
sore throat and fever
unusual bleeding or bruising
*⚫️*Late symptoms of too much medicine being absorbed into the body**
Constipation
convulsions (seizures)
difficult or painful urination
difficulty in breathing
dizziness or lightheadedness, especially when getting up from a lying or sitting position
drowsiness
fast heartbeat
numbness, tingling, pain
Treatment of the partner if he has similar complaints, should also be done

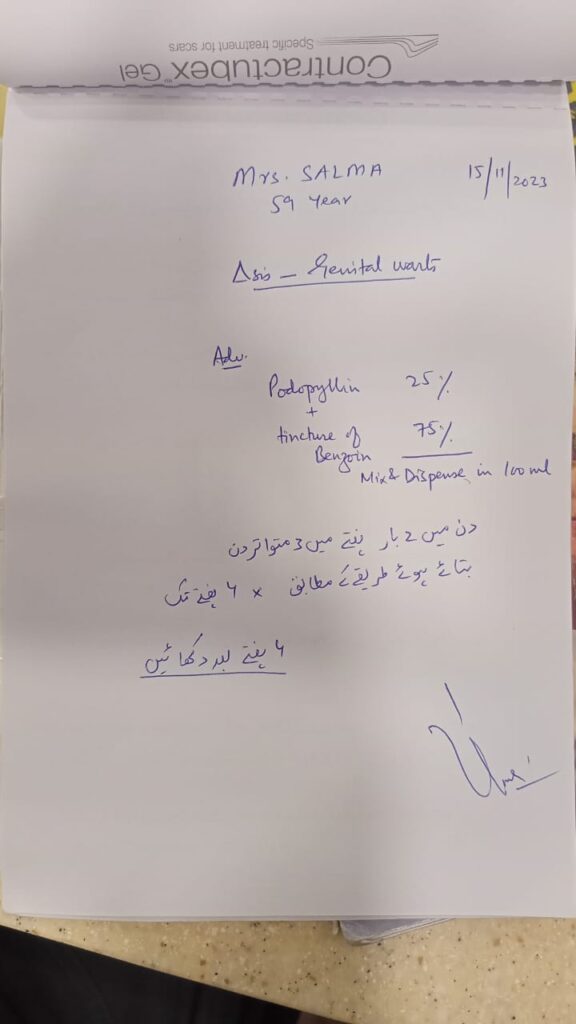
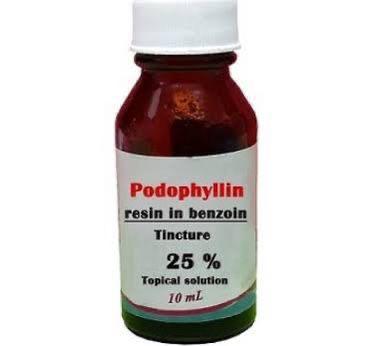
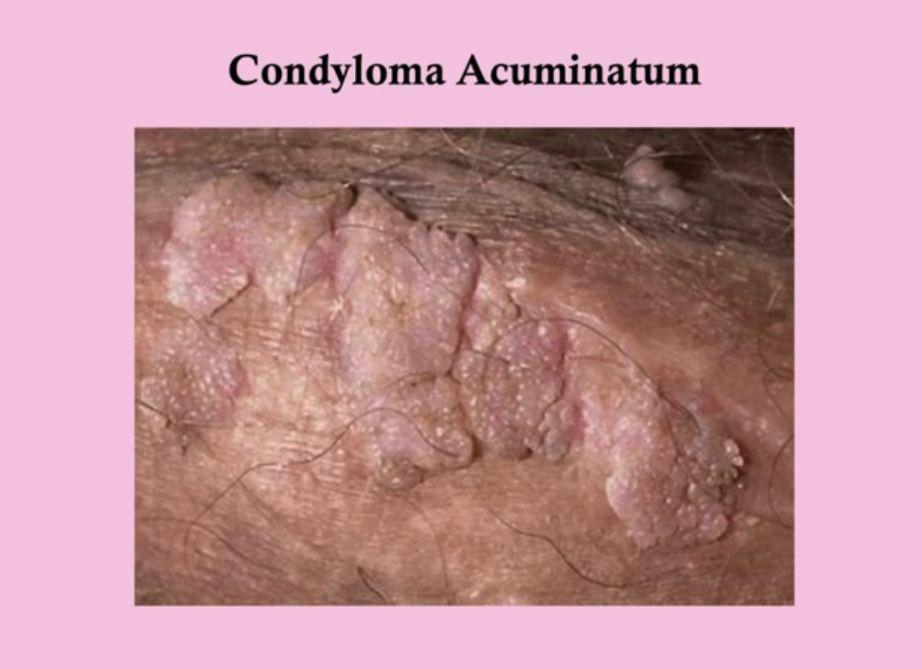
Types of stitches and protocol of how to stitch a knot (clockwise and anticlockwise):
🔹Absorbable and nonabsorbale sutures
Absorbable are those sutures that are absorbed by tissue enzymes or hydrolysis in the body cells and tissue fluids. These are Surgical gut, Chromic gut and Dexon ( polyglycolc acid)
Non absorbable sutures are those that cannot be absorbed by body cells or fluids and require manual removal postop. These include Nylon, Prolene, cotton, silk, braided nylon and multifilament Dacron
🔹Types of suture material used for cutaneous stitches
Nylon
Polypropylene ( prolene, surgilene)
🔹Sutures used for mucosal surfaces
Silk and polyester
🔹Types of suture material for subcutaneous stitches
Polyglactin 910 (vicryl) and polyglyconate (Maxon)
🔺 suture size for ▪️face and neck➡️ 5.0-6.0
▪️Back and scalp➡️3.0-4.0
▪️trunk and extremities ➡️4.0
🔺removal time for suture
▪️face 5-7 days
▪️nack 7-10 days
▪️back and scalp 14-21 days
▪️trunck and extremities 10-14 days
Rest seniors can guide.
before starting procedure u should ask about any bleeding disorder or skin disorder on increased fragility.
diabetes or any immunocompromised state that delays healing.
while suturing ,knot ,and then is there any stretch on underlying skin once u have taken knot
aseptic techniques should be always established.
u can give pain killers ,polyfax to patient and if he is diabetic or immunocompromised u can ask to give short course of oral antibiotics too
before starting procedure u should ask about any bleeding disorder or skin disorder on increased fragility.
diabetes or any immunocompromised state that delays healing.
while suturing ,knot ,and then is there any stretch on underlying skin once u have taken knot
aseptic techniques should be always established.
u can give pain killers ,polyfax to patient and if he is diabetic or immunocompromised u can ask to give short course of oral antibiotics too
The lazy S design may reduce the tension on the wound by using 2 principles: less skin excision and conversion of the tension vectors. The shape of the lazy S design breaks the straight line into 3 or more different directions and vectors. The central area of the wound thus better tolerates tension and gravity
Stitching a knot
Step 1… twice clockwise…
Step 2…one anticlockwise
Step 3…one clockwise
Dog ears usually arise due to shortened incisions like during a tummy tuck. Shorter surgical cuts are harder to suture-close. Thus, the skin at one or both ends of the incision tend to fold and protrude. The location of the surgical incision not only leads to the formation of dog ears but also affects the length of the cut…
– before taking consent ask regarding allergy to local anesthetics
– do explain regarding the potential of scarring in this procedure to remove any unrealistic expectations.
-while marking margins for excision a scale can be used to measure exactly
-mention suture diameter for this particular area that you are performing
– apply sterile petroleum jelly over suture
– in end tell patient when to come back for removal of suture.
Also for knot,repeat 3-4 throws to ensure knot security.over each throw reverse the direction of wrap.
- What is pulley sutures?
Modified vertical mattress sutures, which provide additional wound closure strength.
- What is the rule of suture removal?
The greater the tension across a wound, the longer the suture needs to be in place.
- How is suture sized?
Suture size corresponds to specific tensile strength. Tensile strength decreases as the suture number increases.
- Advantages and disadvantages of different sutures;
- a) Simple interrupted suture
Adv: less potential for wound oedema
Disadv: more tissue required & risk of cross hatching
- B) simple running sutures
Adv: quick placement
Dis : puckering of suture line. Wound dehiscence can occur.
C)vertical mattress suture
Adv: maximum wound eversion and reduced deep space
Dis:risk of cross hatching
- D) horizontal mattress sutures
Adv: useful in areas of high tension
Dis: risk of tissue strangulation
- E) Buried sutures
Adv: useful for wide gaping wounds
Dis: The knot needs to be placed deep in dermis, so it doesn’t present through epidermis
- F) Running subcuticular sutures
Adv: best cosmetic results
Dis: doesn’t contribute to wound strength
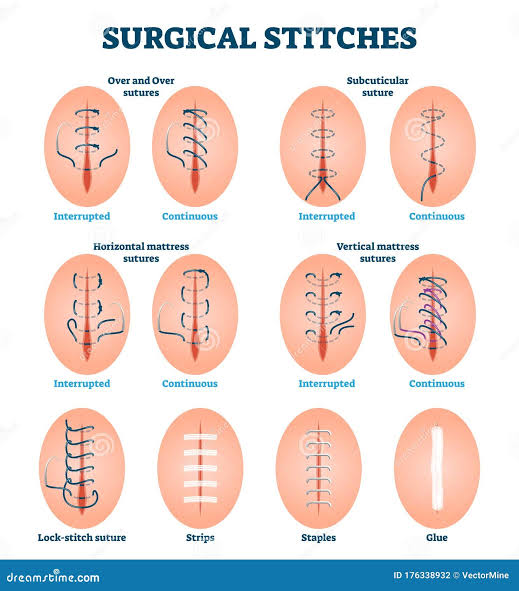
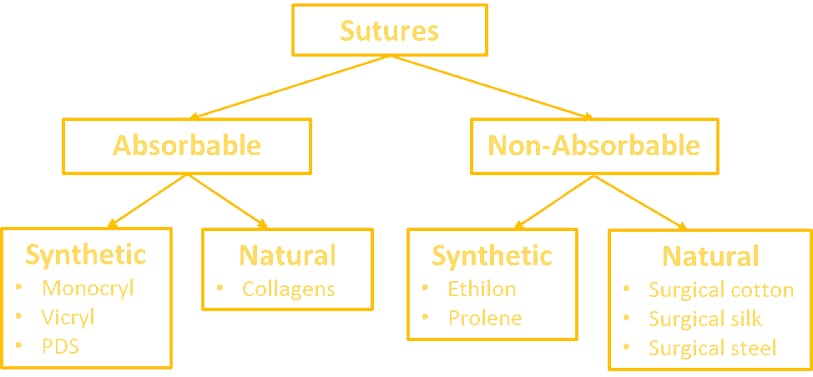



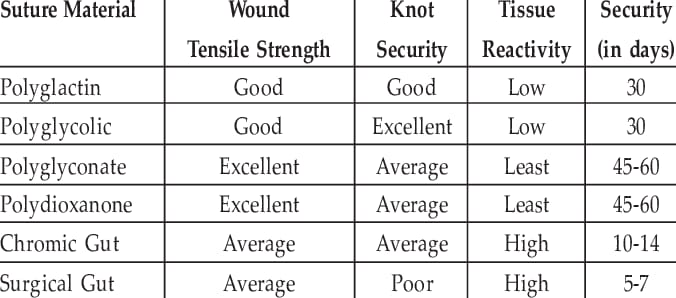

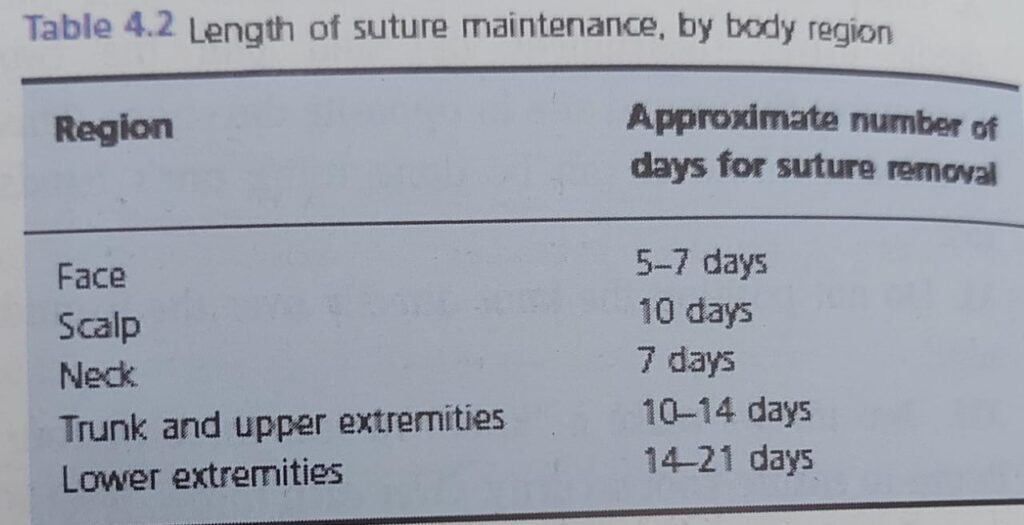
urea lactic acid should also be avoided in first year of life
🔹complications also include…poor sucking,digital vascular constructions
We cannot predict at this stage the outcome of this Mention the optimum temperature and humidity required for good impresson
Counsel that they must bring the child to the hospital in case of fever, illness, infection.
High protein diet.
Counselling for next pregnancies is very important.
Must memorise causes of collodion baby
Q1: What are Adherens junctions?
A: Adherence Junctions are electron dense, transmembrane structures that engage with actin skeleton. They can associate with tight junctions and desmosomes.
Q2. What are Gap junctions?
A: Also known as connexins, which directly form connection between the cytoplasm of adjacent keratinocytes and other cells.
Q3: What are Hemidesmosomal proteins?
A: The hemidesmosomes are seen ultrastructurally as electron dense attachment complexes which extend from intracellular compartment of the basal keratinocytes to lamina lucida in the upper portion of dermoepidermal basement membrane.
Q4: What are the laminins?
A: laminins are other structures that contribute to the formation of BMZ. The major laminin present within the BMZ is Laminin 332, previously known as Laminin 5
Q5: Major collagen present in Basement membrane?
A: Collagen IV
❓ *What are Desmosomes?*
🔹primary keratinocyte intercellular junction Provide structure and integrity to the epidermis by anchoring/attaching to keratins
🔹Consist of desmoplakin (cytoplasmic), plakophilin (cytoplasmic), plakoglobin (cytoplasmic), desmocollin 1/2/3 (transmembrane), and desmoglein 1/3 (transmembrane)
🔹 Desmocollin, desmoglein, and other cadherins are calcium-dependent
❓ *Ideal Site for Biopsy for DIF*
🔹Autoimmune diseases: lesional skin for h/p and perilesional (less than 1cm) skin for DIF. Should be a new lesion
🔹 Connective Tissue diseases: established lesion (sun exposed area) ideally an old lesion more than 06 months but still active .
🔹 Vasculitis: lesion less than 24 hrs old.
❓ *Different Staining Patterns*
🔹Intercellular staining pattern
🔹Linear BMZ pattern
🔹granular BMZ pattern
🔹Shaggy BMZ
🔹Vascular Pattern.
❓ *What are Lamellar Bodies?*
🔹 Odland bodies (lamellar granules) are produced by Golgi bodies in spinous layer Primarily contain *ceramide* (most important lipid involved in epidermal barrier function;
🔹ceramides help form the cornified cell envelope
🔹 *Flegel’s disease* and Harlequin ichthyosis are 2° to ↓lamellar granules 🔹 *X-linked ichthyosis* occurs due to absent steroid sulfatase in lamellar granules
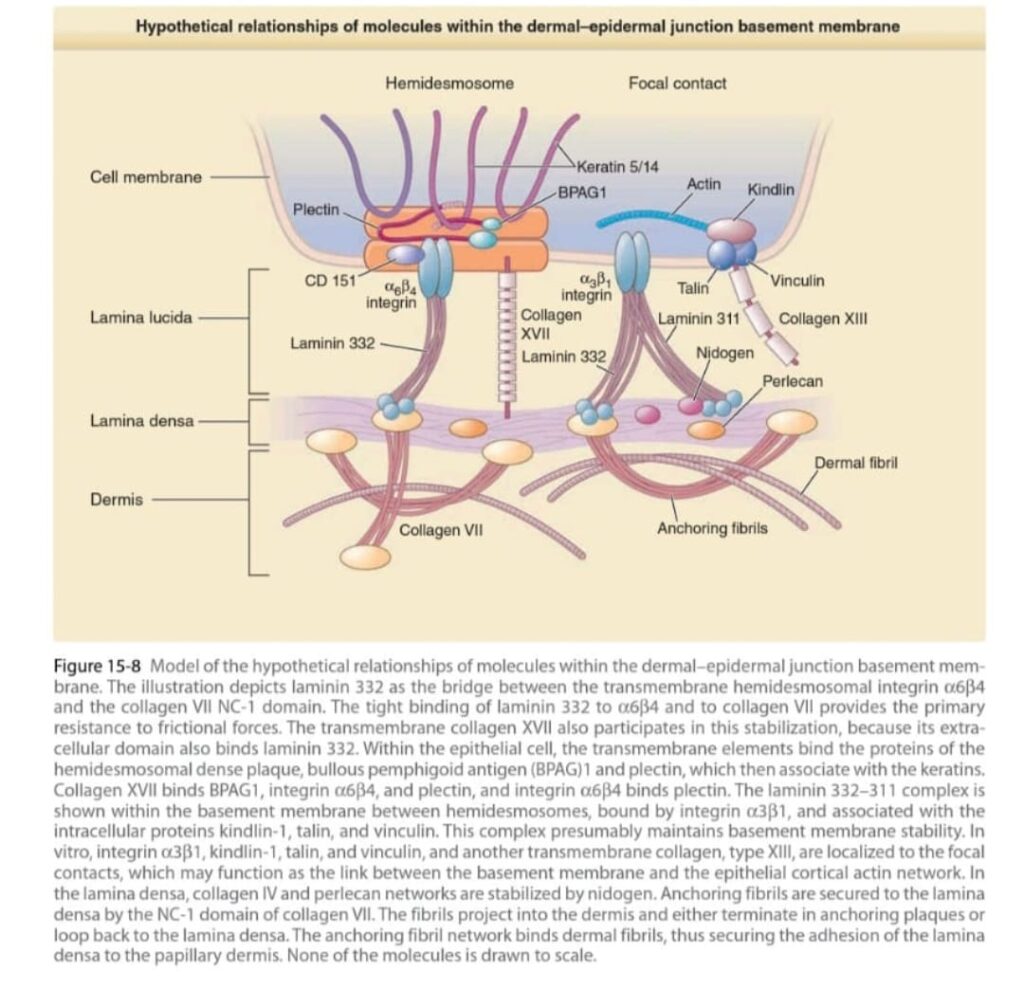
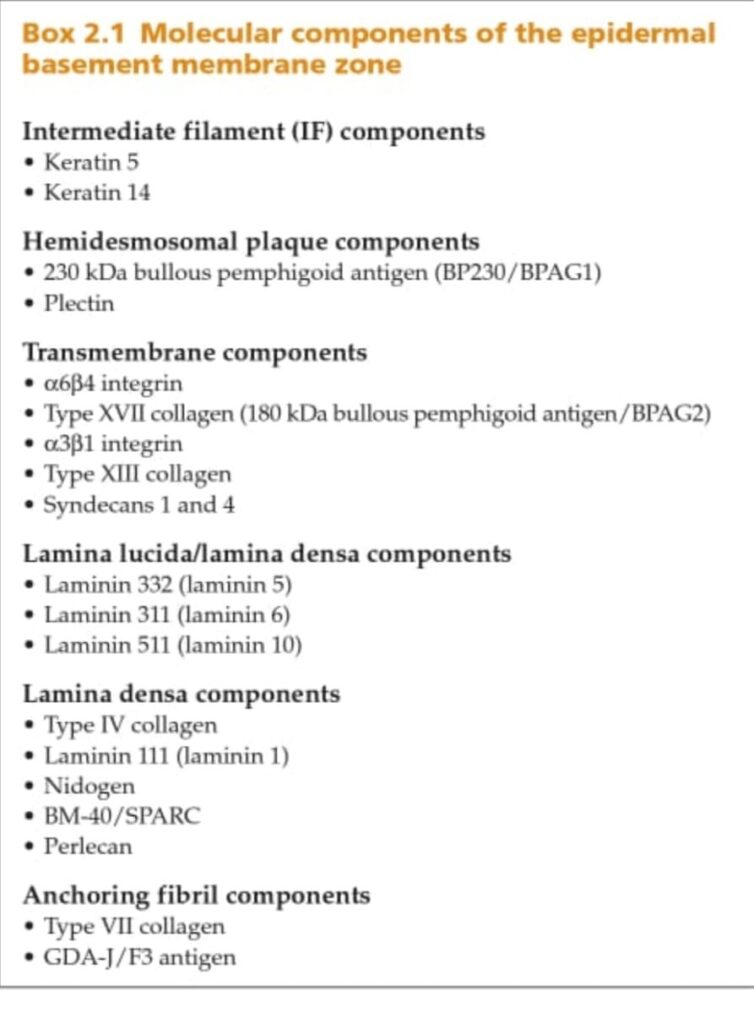
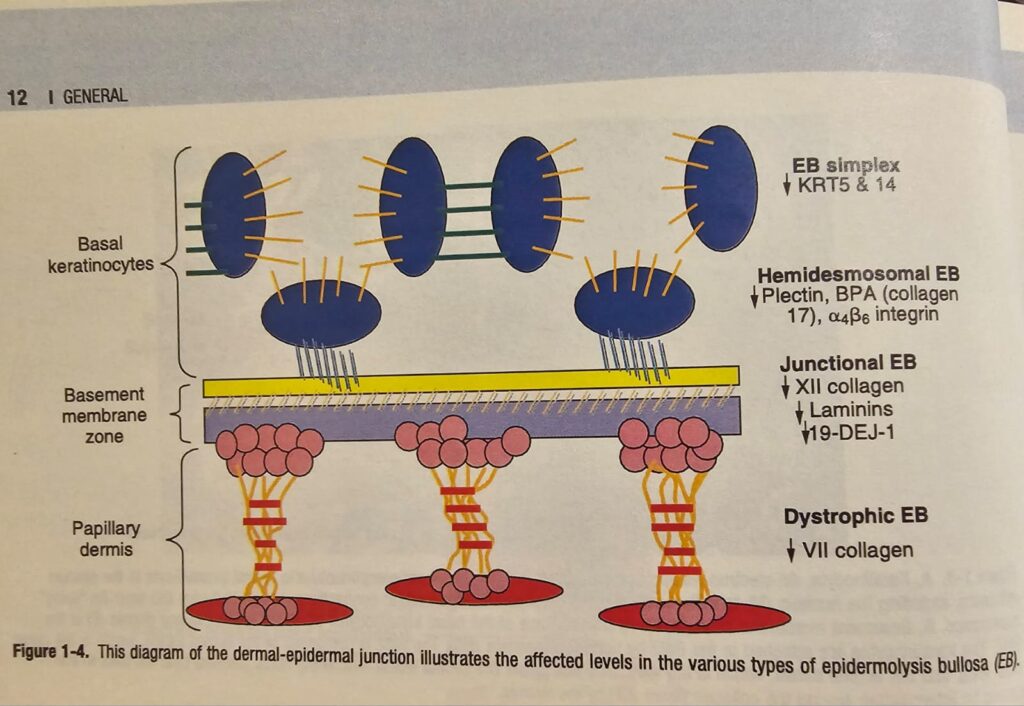

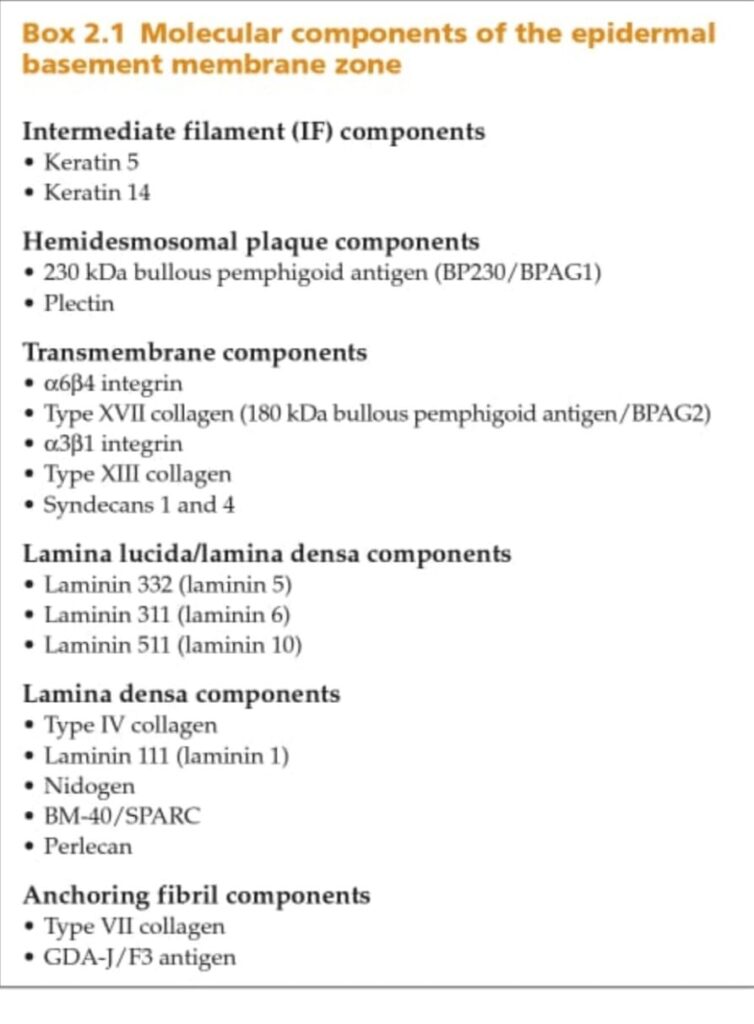
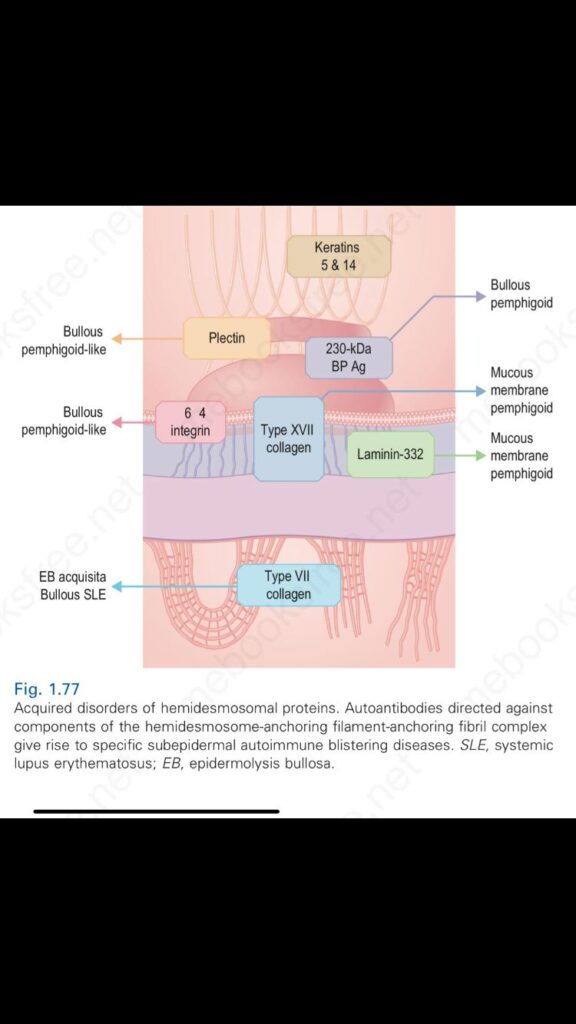
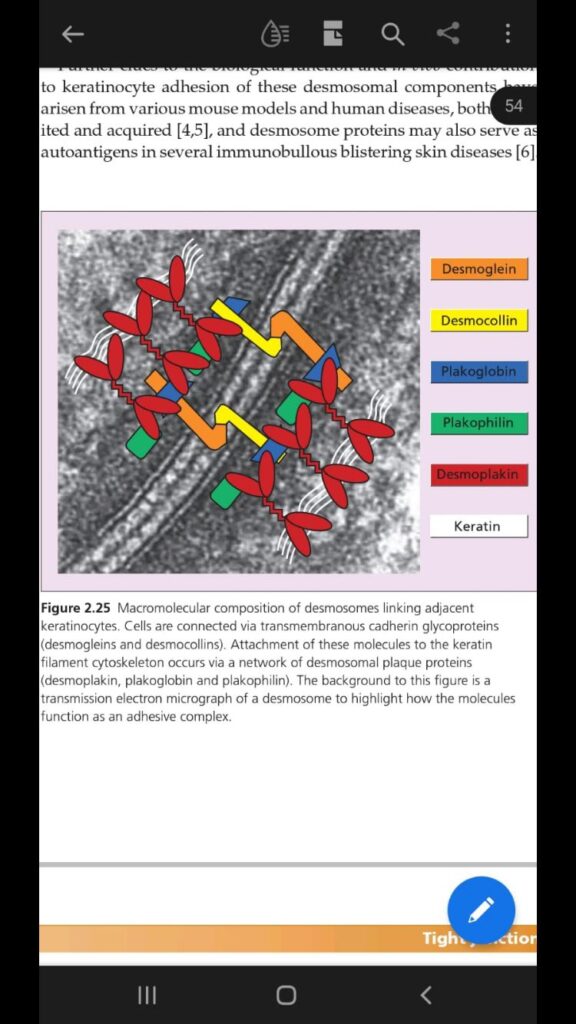
🔰Dr faria’s much fav toacs station 👆🏻
Practice drawing the components of basement membrane
- Mechanism of action of ivermectin?
- It is selective positive allosteric modulator of glutamate-gated chloride channels found in scabies mite.
- Dose of ivermectin?
- 200microgram /kg stat
repeat after 7days.
for crusted scabies, same dose 3 doses, 3 weeks
- contraindications of Ivermite
pregnancy
Lactation
children under 6 years
anaphylaxis to that drug
- How to treat persistent scabies nodule?
- intralesional steroid
- How to treat crusted scabies?
- isolation
3 applications at day 1, 3 and 7
Ivermite 3 weekly doses
trim nails and scrub nail beds daily
Q.Mechanism of action of permethrin?
A.It targets eggs, lice, and mites via working on sodium transport across neuronal membranes causing depolarization.
- complications
A.
nodules
superadded bacterial infections
erythroderma
Glomerulonephritis
vasculitis
– Tell patient that we’re suspecting scabies which is caused by this organism.
– Tell from where you’ll take sample (burrows)
– Keep a gauze piece with you and dab it after the nick just for a good impression
– 10X French letter O
– 40X jet with contrail
– Avoid KOH cuz it will destroy faeces
✅Dermoscopy of burrows and adhesive tape tests are other alternative tests to scraping
🔺On dermoscopy charcteristic ‘Jet with contrail’ is seen
✅In babies face should also be treated with topical to avoid transmission through breastfeeding
Lotion scabion contains sulphur and crotamiton
🔰Also memorize the table given in rooks for the treatment of scabies mite. Names of treatment used, safety window, time of application and adverse effects
1)what’s the basic pathology for melasma
Ans: number of melanocytes not increased in melasma but melanocytes become larger and dendritic suggesting hypermetabolic state
2) what is epidermal dermal n mixed melasma
And: these three types can b distinguished by wood lamp examination
Epidermal melasma give light brown appearance clinically and enhanced colour contrast on wood lamp
Dermal melasma give grey and blusih appearance and less contrast on wood lamp
Dermal melasma is less responsive to treatment
3)give 5 treatment options for melasma
sun protection
kligman regimn
Azelaic acid 20%
Topical rucinol
Kojic acid
Laser therapy( IPL)
Chemical peels
Topical liquiritin
Dermabrassion
Oral,I/L Transamine
Q.What are the main types of epidermal melanin pigmemts?
A.eumelanins
Pheomelanins
Trichochromes
Q.What is kligman regimen?
- Combination of hydroquinone 4%, tretinoin 0.05%, flucinolone acetonide 0.01%
*Darkness*
0 none
1 light brown
2 brown
3 dark brown
4 black
*Homogenisity*
0 none
1 speckled
2 <2cm patch
3 >2cm patch
4 homogenous without clear area
*Coefficient*
Forehead 0.3
Right Cheek 0.3
Left cheek 0.3
Chin 0.1
Area
1 <10%
- 10-30%
- 30-50%
- 50-70%
- 70-90%
- >90%
*MASI score*
Coefficient *(Darkness + homogenisity) *Area
Score is 0- 48
*Modified MASI score*
Coefficient * Darkness * Area
Score is 0-24
If results show reduction from baseline MASI score
>75% Excellent response
50-75% Good response
25-50% fair response
<25% poor response

VIVA QUESTIONS:
What is the mechanism of action of bleomycin?
🔹It has antitumor, antibacterial and antiviral activity.
In low doses it inhibits mitosis and in high doses blocks DNA uptake of thymidine,impeding the S-phase of dividing normal and malignant cells
What are the indications of intralesional Bleomycin injection?
🔹Recalcitrant common,palmar,plantar and periungal warts
🔹Condyloma acuminata
🔹Keloids
🔹Lymphangioma circumscriptum
What are side effects of Inj bleomycin?
🔹Pain
🔹Lymphangitis
🔹Flagellate hyperpigmentation
🔹Raynaud’s phenomenon
What are the containdications?
🔹Pregnancy
🔹Lactation
🔹 vaso occlusive disease
🔹Known hypersensitivity
How much injection can be given at one treatment sitting?
🔹The amount of inj depends on size of wart for 5mm 0.2ml,10mm 0.5 ml,more than 10mm 1.0ml
Total volume injected is limited ro 2ml for a single wart to 1ml
How often to repeat this injection?
🔹Once in 3 weeks.Lesions usually resolve after 1 to 3 injections.
What sign responding warts show?
🔹Hemorrhagic eschar
What is the new technique for bleomycin treatment in warts?
🔹A new technique in which a drop of bleomycin is placed over wart and pricked with a needle into lesion.
Station:5
Intraleseional bleomycin
Other question in this station will be
.how to prepare inj bleomycin for intraleseional
what is price per vial
Price of inj bleomycin 9960 Rs
other causes of Flegellate erythema
Sciatica mushroom
Phytophotodermatitis/ streaky dermatis caused by
Primula albumica
Anacardiacea
🔅For bigger warts you can first par the lesion then give intralesional injection
🔅After prepration of injection it can be stored for 60days at 4-8c
🔅A new technique in which drop of bleomycin is placed over the wart and pricked with needle in to the lesion can also be used

https://youtu.be/VCf5v-p6RJg?si=4GAj0d_jetZ_TvC8
*Important viva questions?*
*What are affects of SLE on pregnancy* .
SLE increases the risk of spontaneous abortion, intrauterine fetal death, preeclampsia, intrauterine growth retardation, and preterm birth. The presence of SSA and SSB antibodies can lead to fetal heart block and neonatal lupus.
*What is the prognosis of mother and child during SLE in pregnancy.*
The prognosis for both mother and child is best when SLE is quiescent for at least 6 months before the pregnancy and when the mother’s underlying kidney function is stable and normal or near normal. Lupus nephritis can worsen during pregnancy.
*How flare of SLE is treated during pregnancy* .
Flares of SLE are uncommon during pregnancy and are often easily treated with steroids. The most common signs and symptoms of these flares include arthritis, rashes, and fatigue.
*What laboratory studies are recommended with the first visit after or when pregnancy is confirmed:*
Kidney function tests, including determination of the (GFR), urinalysis, and measurement of the urinary protein-to-creatinine (P/C) ratio
CBC,
Test for anti-Ro/SSA and anti-La/SSB antibodies,
Lupus anticoagulant and anticardiolipin antibody studies,
Anti–double-stranded DNA (anti-dsDNA) test,
Complement studies (CH50 or C3 and C4).
*What is the safe dose of prednisolone that can be used safely during breastfeeding in a woman with SLE.*
Prednisone (< 15-20 mg/d) can be used safely during breastfeeding because only small amounts (5% of the dose) are secreted in breast milk. Breastfeeding women who are taking doses of prednisone higher than 20 mg once or twice daily should pump their breast milk and discard it 4 hours after taking the prednisone, to minimize drug exposure to the infant.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5446003
*Risks in SLE*
8-36% abortion
20% pre eclampsia
1/3rd. Premature
1/3rd. C section
APLA 45-90% abortion which when rx dec to 30%
2% 1st pregnancy
25% 2nd pregnancy
🔺What are types of microscope?
✏️Simple Microscope
✏️Compound Microscope
✏️Electron Microscope
✏️Stereo Microscope
✏️Scanning Probe
🔺indications of oil immerssion lens
✏️to visualize lepra bacilli
✏️to visualize scabies mite
🔺which oil in used?
✏️cedar wood oil
🔺what is confocal microscopy?
✏️The primary functions of a confocal microscope are to produce a point source of light and reject out-of-focus light, which provides the ability to image deep into tissues with high resolution, and optical sectioning for 3D reconstructions of imaged samples.
HOW TO USE IMMERSION OIL?
Purpose:
To increase the resolving power of the microscope.
STEPS:
1.the slide alongwith the coverslip must be viewed at 4X,10X and 40X first.
2.lower the stage
3.move objectives between 40X and 100X.
4.put one generous drop of immersion oil on the coverslip.
5.move to 100X objective.
6.adjust focus to move the stage back till oil and objective come in close contact.
The objective nearly touches the cover slip.
7.view the slide in detail.
8.pull down the stage
9.remove the slide.
10.clean the objective with lens paper bit by bit by gently dabbing till no oil is left.
Precautions:
1.Never go back to 40X once there’s oil on objective and slide.
2.never clean the 4X,10X and 40X objectives with the same lens paper that was used to clean oil.
🛑 WHAT IS ABPI?
🔵 The ankle-brachial index (ABI) is a quick, non-invasive technique used to check vascular status ESPECIALLY for peripheral arterial disease (PAD).
🛑 INDICATIONS OF APBI?
🔵
☑️. Symptoms of peripheral artery disease:
Intermittent claudication or cramping pain in the legs.
☑️.. Wounds on the legs that are slow to heal.
☑️.. Leg that feels colder than other parts of the body or is a different shade of color.
☑️.. Patients age more than 70 or patients with age >50 having risk factors of PAD, like smoking, obesity, family history of dyslipidemia, early stroke or myocardial infarction.
☑️.. Monitoring of very low initial ABPI or if patient taking therapy for PAD.
🛑 *RISK FACTORS OF PAD?*
☑History of tobacco use/SMOOKING
☑Diabetes
☑High blood pressure
☑High cholesterol
☑Restricted blood flow (atherosclerosis) in other parts of body. Such as CAD.
☑History of stroke or transient ischemic attack.
☑Family history of heart disease.
☑Over 70 years of age.
🛑 *CONTRAINDICATIONS OF ABPI?*
❌ *DEEP VEIN THROMBOSIS:* Avoid compression of the extremity with known or suspected deep vein thrombosis due to concern for breaking and embolizing a thrombus.
❌ *SEVERE LEG PAIN:* Performing ABI measurement requires significant pressure to be applied to the leg. Whether related to leg ischemia, fracture/swelling, or wounds, this procedure can cause significant pain for the patient.
❌ *PATIENT UNABLE TO LIE IN SUPINE POSTION*: Either because of other articular disease, sever pain in limb due to any reason like PAD, ULCER OR FRACTURE.
🔥🔥 *IMPORTANT STEPS BEFORE PERFORMING ABPI: *
📌. *REST AND RELAX THE PATIENT:* patient should have a specific rest period before assessing ABI, ranging from 10 to 30 minutes. your method of greeting and counseling about procedure will also decrease the anxiety of patient, in other words WHITE COAT HYPERTENSION during this time.
📌 . *AVOID NICOTINE:*~ smoking selectively affects the ankle but not the brachial systolic pressure, resulting in artificially elevated values. tell patient not to smoke or take tea , coffee or tobacco during this time.
📌. *SUPINE POSITION:* with sitting position, there is increase in the ABI value by approximately 0.3 in contrast to supine position.
📌. *QUIET SPACE:* Avoids underestimating systolic pressure due to difficulty with the audibility of systolic sounds. 5. COVER WOUNDS: Reduces the risk of contaminating wounds or equipment.
🛑 *PROCEDURE:*
In exam, you might not have doppler ultrasound but you should mention that doppler ultrasound would be better for this procedure if available. Second thing is that if you are using finger method for pulse detection in lower limbs, i think you should also use the same method for brachial artery instead of stethoscope to avoid the error…because you need systolic pressure only… So either use stethoscope for both upper and lower limbs or use finger method. But ideally same method for both..
Here i will request the SENIORS for expert opinion as I didn’t find that.
🛑 LIMITATIONS OF ABPI?
*📌.* Calcification of arteries in DIABETES, CHRONIC KIDNEY DISEASE (shows increase ABPI, more than 1.4), joint problems.
*📌.. Cannot localize the exact position of blockage or narrowing. Use duplex scan for such reasons.
*📌.. If there is a large ulcer that is painful and also not enough space for cuff to apply.
https://youtu.be/nhL0Y_xOJI8?si=J9uL7IGk6SK4tfSl
In exam, usually non ulcer pt is there but they can bring any thing n any patient so be prepared for worst n must see videos for taking ABPI in real ulcer patient as well usually in that u cover ulcer with guaze and put cuff of bp app a little higher not on the ulcer .
Literature search
Operational definition
Ethical considerations👇🏻👇🏻
Informed consent
Voluntary participation
Confidentiality
Potentional for less harm Result communication
Study design👇🏻
Descriptive study👆🏻
Analytical study👇🏻
Experimental study
Selection of controls
Sampling
Data
Bias
Confounders
Null hypothesis
Testing of hypothesis and P value
Sensitivity and specificity

Objective, methodology and rationale
Objective, methodology and rationale
Metaanalysis
Reference writing
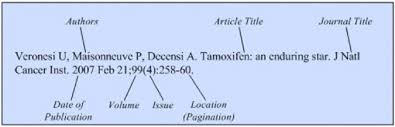
Author name.article title.journal title.year;volume(issue):page
Plegiarism
Who is an author
Research k liye ap ne toacs tak yehi prepare karna hai 👆🏻
🔰 IMPORTANT NOTE
For research above given voice notes summarize everything. For practice its very important tht u go through the abstracts of different study and try to find out the type of study, point out the important aspects of an bstract bcoz sometimes they provide u an abstract and ask for the missing parts of tht particular abstract. Calculation of specificity and sensitivity is another imp and fav question of cpsp which frequently comes in mcq exam.
For reference, u may read this ppt as well which provided by cpsp.
*Procedure:*
1️⃣Greet and introduce yourself
2️⃣take informed consent (explain possible side effects)
3️⃣rule out all the contraindications
4️⃣ask to take photographs for future references
5️⃣Ist clean the face with alcohol swab to make it free of any cosmetics
6️⃣Apply anesthetic cream starting from forehead and covering whole face
*Note : to make it work better we can use polythene wrap to cover it*
Leave it for 30-60 minutes and then wipe the cream clean with a help of a swab
7️⃣mark the area to be treated with a white skin pencil
8️⃣Start injecting the mesotherapy solution in the form of small depots at a distance of 1cm,starting from any one side
You can use guaze to clean any spill of blood by using a dabbing movement( donot rub)
9️⃣make the patient wait for 30 mins to observe any excessive bleed,ooze or swelling before leaving
🔟explain all post-procedure care and say thanks to the patient.
https://images.app.goo.gl/5Beu1exrp2QVCgMu7
*🛑🛑🛑*VIVA QUESTIONS*🛑🛑
🛑What is mesotherapy???
❇️ Its a technique of injecting certain substances into skin (intradermally) using very fine needles
🛑What are the indictaions of mesotherapy??
❇️acne,acne scars
❇️to decrease melasma
❇️wrinkles and fine lines ❇️body sculpting
❇️mesobotox
❇️Alopecia
❇️chronic non healing ulcers
🛑 what substances can be injecting using mesotherapy techniques
❇️enzymes
❇️vitamins
❇️minirals
❇️hormones
❇️plant extracts
❇️growth factors
❇️ drugs
🛑Which chemicals are commonly used for the treatment of melasma?
❇️Glutathione
❇️tranexemic acid
❇️Vitamin C
❇️niacinamide
🛑 What is the mechanism of action of tranexemic acid in melasma
❇️In melasma, the hypothesised mechanism of action of tranexamic acid includes the shrinkage of dermal vasculature and reduced melanin synthesis by altering the interaction of keratinocytes and melanocytes and reducing tyrosinase activity.
🛑Enumerate few contraindictaions
❇️hypersensitivit to any chemical being used
❇️pregnancy,lactation
❇️blood thinning agents
❇️bleeding tendencies
❇️keloidal tendencies
❇️use of NSaids
❇️Use of isotretinoin in last three months
🛑Explain post-mesotherpay care to the patients
❇️ keep your self hydrated
❇️ stay away fron sun and use sunscreens religiously for next two weeks
❇️you can resume your daily activities immidiately after the procedure
❇️use topical antibiotic for next 3-5 days
❇️book for next appointment after 2 weeks
⭐️Rule out active infection and address unrealistic expectations of the patient before the procedure
⭐️Topical antibiotic cream should be prescribed after the procedure.
⭐️Follow up regimen should be properly explained to patient.
https://youtu.be/X7jwq0H1Zk4?si=tym4_ZBP8YBcpD_v
🛑 Tell the patient about outcome and of number of sessions needed as patients desire their best results in 1 or 2 sittings. Mesotherapy usually requires 3-15 treatment sessions 2 wks apart.
🛑🛑In contraindications add:
📍age less thsn 18 years
📍use of cardiac drugs like amiodarone, CCB, beta blockers
📍insulin department diabetes
📍seizures
📍lupus
📍radiotherapy within last year
📍📍stop NSIDs 1 week before procedure .
PUVA therapy with viva Questions and Answers
*What are psoralens and their types?*
Psoralens are naturally occurring tricyclic furocoumarins present in a large number of plants, but synthetic compounds also exist.
Types
🔺8-MOP (methoxypsoralen)- plant origin
🔺5-MOP
🔺4,5,8 TMP (trimethoxypsoralen)
*What is the mechanism of action of PUVA therapy?*
*Anti-proliferative effect*
Photo conjugation to DNA results in suppression of mitosis, DNA synthesis, and cell proliferation.
*Anti-inflammatory and immunosuppressive effects*
Down regulates >>> lymphocyte and APC functions
Influences adhesion molecule expression
Diminishes langerhans cell numbers within the epidermis.
*Stimulate melanogenesis*
Photo conjugation of psoralen to DNA in melanocytes, increased formation and menlanization off melanosomes, an increased transfer of melanosomes to keratinocytes and activation and increased synthesis of tyrosine mediated by stimulation of cAMP activity.
*How to initiate the therapy?*
🔺 Starting dose 8-MOP (0.6-0.8mg/kg) and 1.2 mg/kg for 5-MOP.
Dose according to body surface area:
🔺25 mg/m2 for 8-MOP and 50 mg/m2 for 5-MOP
taken 2 hours before UVA exposure, with food.
🔺Determine MPD as a starting dose.
🔺Frequency of therapy:
Twice weekly
🔺Increment of dose at each visit:
Initial 0.5 to 1.0j/cm2
🔺If no response:
Then 1.0- 1.5 j/cm2
🔺If there is no response after 15 sessions:
Then,increase the dose of MOP(0.8mg/kg)
*What is the Minimal Photo-toxic dosee (MPD) ,and how is it calculated?*
🔺The dose of PUVA is required to produce a minimally perceptible erythema (E1) 48 hours after exposure.
🔺The starting dose should ideally be based on the patient’s MPD
and between 40% (topical PUVA) and 70% (oral PUVA) of the MPD, it is recommended.
🔺If MPD testing is unavailable or the patient’s skin is too extensively involved to measure the MPD, the starting dose is based on skin phototype:
🔹I, 0.5 J/cm2;
🔹II, 1.0 J/cm2;
🔹III, 1.5 J/cm2;
🔹IV, 2.0 J/cm2.
🔺The starting dose of bath PUVA should always be based on MPD testing because of the risk of severe photosensitivity
*What are the grades of erythema?*
🔺E0: No erythema
🔺E1: Minimally perceptible erythema (faint pink)
🔺E2:marked erythema
🔺E3:Fiery red erythema with oedema
🔺E4:Fiery red erythema with oedema and blistering
*How to manage if erythema occurs?*
🔺If trace erythema occurs,the dose should not be increased, but the patient may be treated with previous exposure time.
🔺If more than trace erythema occurs, with tightness or burning,areas should not be treated until symptoms subside.
*What is the maintainance protocol?*
🔺If > 95% clearance>>>>> last clearance dose once weekly.
🔺If persists for 4 weeks>>>> reduce frequency of fortnightly
🔺If it persists for 8 weeks>>>> reduce to once monthly
🔺I it persists for 4 months, treatment may be stopped
🔺 If there is relapse during maintainance,increase to twice weekly and increase dose by 0.5 to 1.5 J/cm for each successive treatment.
*When to label treatment failure?*
🔺No significant response(at least 50% clearance) after 30 treatments.
*How to manage defaulter cases?*
🔺Missed one treatment -> use the last dose
🔺Missed more than 1 session -> dose should be reduced by 0.5 J/cm per session missed
🔺Missed more than a month -> Start from the baseline
*What are the indications of PUVA?*
🔺Psoriasis
🔺Atopic Dermatitis
🔺CTCL
🔺Vitiligo
🔺Polymorphic light eruption
🔺Others : Alopecia areata , lichen planus, granuloma annulare , necrobiosis lipoidica , systemic sclerosis/ Morphea , PRP, etc.
*What are the contraindications of PUVA?*
*Absolute contraindications*
🔹Dysplastic naevus syndrome
🔹Systemic lupus erythematosus
🔹Dermatomyositis
🔹Genetic skin cancer syndromes (xeroderma pigmentosum,Gorlin syndrome)
🔹Bloom syndrome
🔹Cockayne syndrome
🔹Concomitant specific oral immunosuppressive medication:
🔹azathioprine
🔹ciclosporin
🔹 mycophenolate mofetil
🔹tacrolimus
🔹Patients unwilling or unable to comply with safety procedures.
🔹Patients who are medically unfit and unable to stand, e.g.severe cardiovascular or respiratory disease
*Relative contraindications*
🔹Age<16years
🔹Previous or current non-melanoma skin cancer
🔹Previous melanoma
🔹Previous exposure to arsenic or ionising radiation
🔹Current premalignant skin lesions
🔹Previous or concomitant oral immunosuppressive therapy
🔹Photo-induced epilepsy
🔹Pregnancy
🔹Cataracts
🔹Bullous pemphigoid/pemphigus
🔹Significant liver dysfunction
*What are the different methods of delivering PUVA therapy?*
🔺Systemic / Oral
🔺Topical PUVA
🔺Bath for whole body
🔺Soaks, cream, gels, and paints for hands feet and scalp and localized areas.
*What are the complications?*
*Acute effects*
🔺 Phototoxicity
Peak erythema following administration of oral PUVA occurs between 72 and 120 h.
Topical PUVA between 96 and 144 h.
Rarely, *photo-onycholysis* or *subungual haemorrhage*
🔺Pruritis and Pain
🔴PUVA pain is important to identify as management is difficult. Low-frequency electrotherapy topical capsaicin and oral gabapentin or phenytoin have all been advocated.
The continuation of PUVA or further courses in the future are contraindicated as recurrence of pain is common.
🔺Nausea
🔺Blistering
🔹Subepidermal blister
🔹Induction of bullous pemphigoid
🔺Provocation of photodermatosis
🔹Polymorphic light eruption, SLE
🔹Reactivation of herpes simplex
*Chronic*
🔺PUVA keratosis
🔺PUVA lentigines
🔺Photoageing
🔺Carcinogenesis
🔺Risk of nonmelanoma skin cancers
🔺Melanoma
🔺 Cataract
*What combination therapies can be given with puva?*
More effective and synergistic effects
Decrease comulative dose of UVA
🔺 Topical treatments
🔹Emollients
🔹Tar
🔹Dithranol
🔹Tazarotene
🔹Calcipotriol
🔺Systemic
🔹Oral Retinoids
🔹Interferon Alpha
🔹Bexarotene
*What are the Post treatment precautions?*
🔺Protective eyewear be worn for 12 h after the ingestion of psoralen and for 24 h in individuals with pre-existing cataracts or who may be at increased risk of cataract (e.g. children and patients with atopic eczema)
🔹Avoidance of sunlight with sunscreen
*Maximum treatment sessions?*
🔺150 – 200 sessions
🔺1000 to 1500 j/cm²
🔹Maintainance therapy should be avoided.
*Benefits of topical over systemic puva?*
🔺Topical therapy is preferable to oral therapy in patients with:
🔹 hepatic dysfunction
🔹gastrointestinal disease
🔹cataracts
🔹poor compliance with eye protection
🔹risk of drug interactions (e.g., warfarin)
🔹to allow shorter irradiation times (e.g., for children, the elderly or those with claustrophobia).
*How is the patient monitored?*
🔺CBC RFTs, LFTs monitoring as required
🔺Ophthalmological exam: baseline, 6, 12 months interval
🔺Thorough cutaneous examination 3 monthly
Mostly examiners ask about pre requisite, counselling, post procedure care, counseling related to it.
🔘 *Counselling / Viva on Drug – Secukinumab*
💊 *Scenario:*
A young male is newly diagnosed with plaque Psoraisis with multiple scaly, erythematous, and pruritic plaques on scalp, trunk, and knees, involving BSA of 10% with involvement of nails. He has no other known comorbids and has heard about biologic drug Secukinumab from his friend that this drug can completely arrest the disease progression so he consulted you to prescribe him Secukinumab, how will you assess and counsel the patient?
🔘 *Viva Questions (Q) and their Answers (A)*
🧐 Q: What is the mechanism of action of Secukinumab?
🌜 A: Secukinumab is a monoclonal antibody that selectively targets and neutralizes interleukin-17A (IL-17A), thereby reducing inflammation in conditions such as psoriasis and psoriatic arthritis.
🧐 Q: What are the FDA-approved indications for Secukinumab?
🌜 A: Secukinumab is FDA-approved for the treatment of moderate to severe plaque psoriasis, psoriatic arthritis, and ankylosing spondylitis in adult patients who have had an inadequate response or intolerance to previous therapies.
🧐 Q: How is Secukinumab administered?
🌜 A: Secukinumab is administered by subcutaneous injection.
🧐 Q: What are the common adverse effects of Secukinumab?
🌜 A: Common adverse effects of Secukinumab include upper respiratory tract infections, headache, injection site reactions, and diarrhea. Additionally, there is a potential risk of developing serious infections and allergic reactions.
🧐 Q: Can Secukinumab be used in pregnant women?
🌜 A: The use of Secukinumab in pregnant women is not recommended unless the potential benefits outweigh the risks. Pregnant women should consult their healthcare provider before using Secukinumab.
🧐 Q: How does Secukinumab compare to other biologic agents in the treatment of psoriasis?
🌜 A: Secukinumab has demonstrated efficacy in the treatment of psoriasis, particularly in patients who have not responded adequately to other systemic therapies. It has been shown to have comparable or superior efficacy to other biologic agents such as etanercept and ustekinumab in clinical trials.
🧐Q: What investigations should be conducted before initiating treatment with Secukinumab?
🌜 A: Before initiating treatment with Secukinumab, patients should undergo screening for latent tuberculosis infection (LTBI) with tuberculin skin testing or interferon-gamma release assays. Additionally, baseline assessments of liver function tests along with test for other chronic diseases & infections including Hepatitis B/C & IBDs and blood counts, should be performed. In patients with psoriatic arthritis, baseline assessments of joint function and imaging studies may also be indicated. Assessment for Malignancies & Psychological evaluation are also indicated prior to starting Secukinumab.
🧐 Q: What is the recommended dosing regimen for Secukinumab in the treatment of psoriatic arthritis?
🌜 A: The recommended dosing regimen for Secukinumab in the treatment of psoriatic arthritis involves a loading dose of 150 mg or 300 mg administered by subcutaneous injection at weeks 0, 1, 2, 3, and 4, followed by maintenance doses of 150 mg or 300 mg every 4 weeks thereafter, depending on the patient’s response. It’s the same as for Psoriasis.
🧐Q: What investigations should be conducted after initiating treatment with Secukinumab?
🌜 A: After initiating treatment with Secukinumab, patients should be monitored for signs of infection, including tuberculosis. Periodic assessments of liver function tests and blood counts should also be conducted to monitor for potential adverse effects. In patients with psoriatic arthritis, assessments of joint function and disease activity may be performed at regular intervals to evaluate treatment response.
🧐Q: Are there any specific contraindications to the use of Secukinumab in patients with psoriasis?
🌜 A: Secukinumab is contraindicated in patients with a history of hypersensitivity to the active substance or any of the excipients in the formulation. Additionally, caution should be exercised in patients with active infections, including chronic or localized infections, as Secukinumab may increase the risk of serious infections.
*Absolute Contraindications:*
- Hypersensitivity: Patients with a known hypersensitivity to Secukinumab or any of its components should not receive the drug due to the risk of severe allergic reactions.
- Active Infections: Secukinumab should not be initiated in patients with active infections, including chronic or localized infections, as it may exacerbate the infection or increase the risk of serious infections.
*Relative Contraindications:*
- Latent Tuberculosis Infection (LTBI): While not an absolute contraindication, caution should be exercised in patients with LTBI. Treatment for LTBI should be initiated prior to starting Secukinumab to reduce the risk of reactivation.
- Malignancy: The safety of Secukinumab in patients with a history of malignancy has not been established. Caution should be exercised, and the potential risks and benefits should be carefully evaluated in patients with a history of malignancy.
- Pregnancy and Lactation: While there is limited data on the use of Secukinumab in pregnant or breastfeeding women, caution is advised, and the potential risks and benefits should be discussed with the patient.
- Immunocompromised Patients: Secukinumab may increase the risk of infections in immunocompromised patients. Caution should be exercised, and the patient’s overall immune status should be considered before initiating treatment.
🧐Q: How does interleukin-17A contribute to the pathogenesis of psoriasis?
🌜 A: Interleukin-17A (IL-17A) is a key cytokine involved in the pathogenesis of psoriasis. It promotes the activation and recruitment of various immune cells, including neutrophils, T cells, and dendritic cells, leading to inflammation and keratinocyte hyperproliferation. IL-17A also induces the production of other pro-inflammatory cytokines and chemokines, exacerbating the inflammatory cascade and contributing to the development of psoriatic plaques.
🧐 Q: Can Secukinumab be used in patients with comorbidities such as diabetes or hypertension?
🌜 A: Secukinumab can generally be used in patients with comorbidities such as diabetes or hypertension. However, caution should be exercised in patients with uncontrolled comorbidities, as there may be an increased risk of complications. Close monitoring and coordination with other healthcare providers may be necessary to ensure optimal management of comorbid conditions during treatment with Secukinumab.
🧐 Q: What is the efficacy of Secukinumab in patients with nail psoriasis?
🌜 A: Secukinumab has demonstrated efficacy in the treatment of nail psoriasis, characterized by improvements in nail bed and nail matrix psoriasis severity scores. Clinical trials have shown that treatment with Secukinumab leads to significant improvements in nail psoriasis symptoms, including nail pitting, onycholysis, and subungual hyperkeratosis.
🧐Q: Are there any special considerations for the use of Secukinumab in elderly patients?
🌜 A: Elderly patients may be more susceptible to certain adverse effects of Secukinumab, such as infections. Therefore, caution should be exercised when initiating treatment in this population, and close monitoring for signs of infection is recommended. Additionally, elderly patients may have age-related changes in renal or hepatic function that could affect drug metabolism and clearance, so dose adjustments may be necessary in some cases.
🧐Q: Can Secukinumab be used in patients with a history of malignancy?
🌜 A: The safety of Secukinumab in patients with a history of malignancy has not been established. Caution should be exercised when considering treatment with Secukinumab in patients with a history of malignancy, and the potential risks and benefits should be carefully weighed on a case-by-case basis. Close monitoring for signs of malignancy recurrence or progression is recommended during treatment with Secukinumab.
🔴 trade name of secukinumab?
-Cosentyx (comes in vial as well as pre-filled)
-Fraizeron (comes in vial)
In Pakistan, they are available in 150mg strength
150mg vail for 60,000rps
* FDA approved also in Hypertrophic palmoplantar psoriasis, Generalized pustular psoriasis
* Cautions: in IBD pts, patients with sucidal ideation, malignancies
* Contraindications: hypersensitivity, active infections
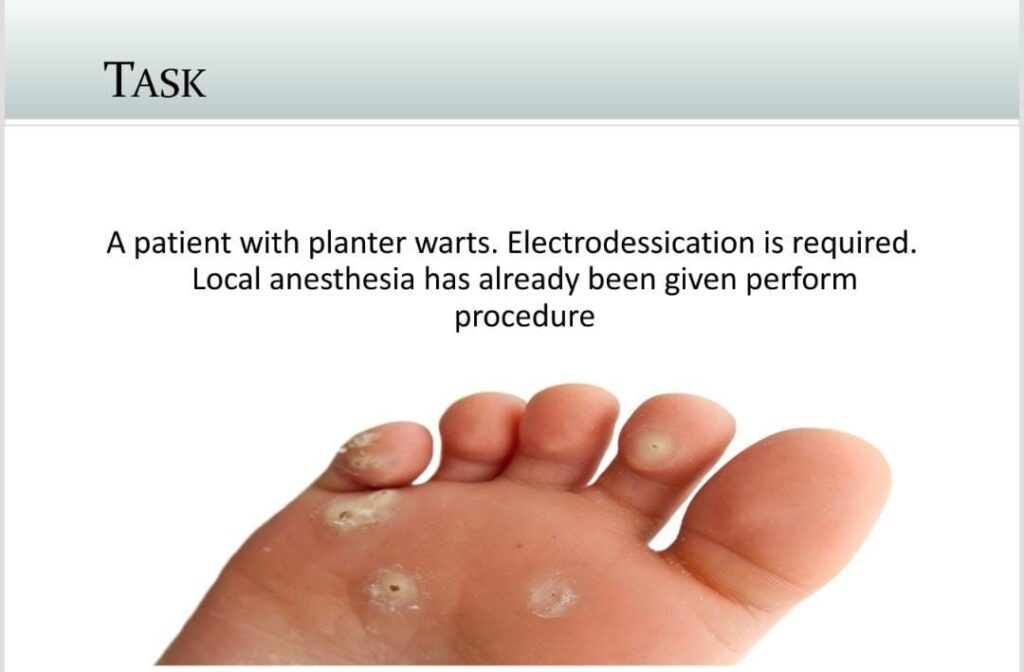


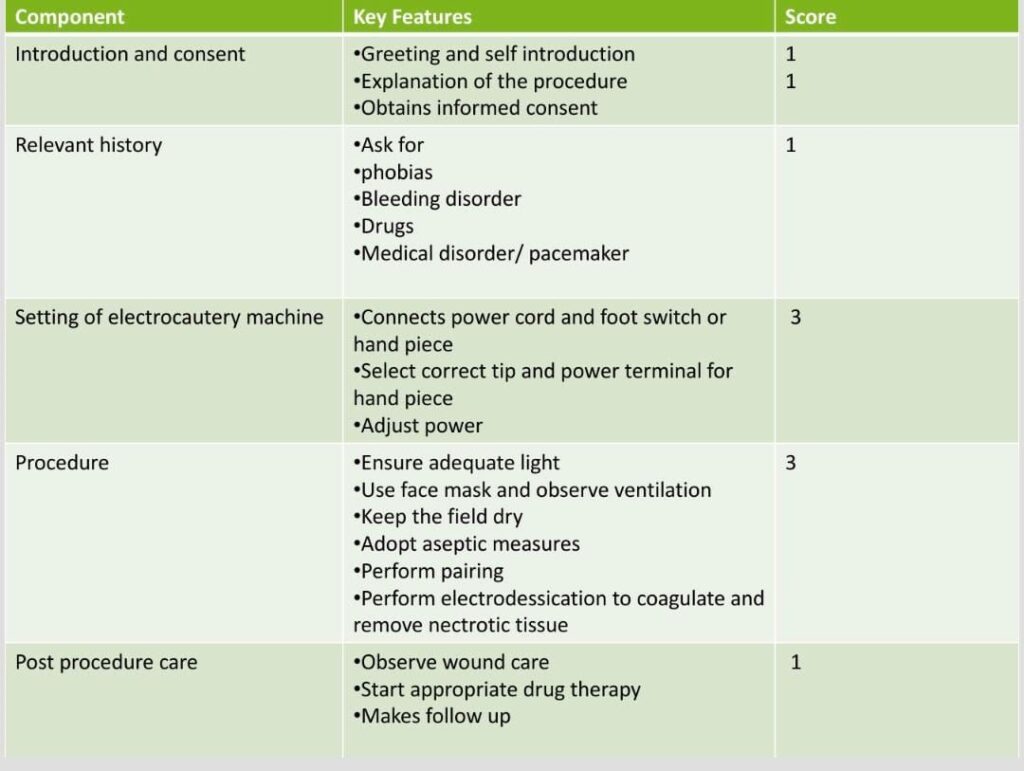
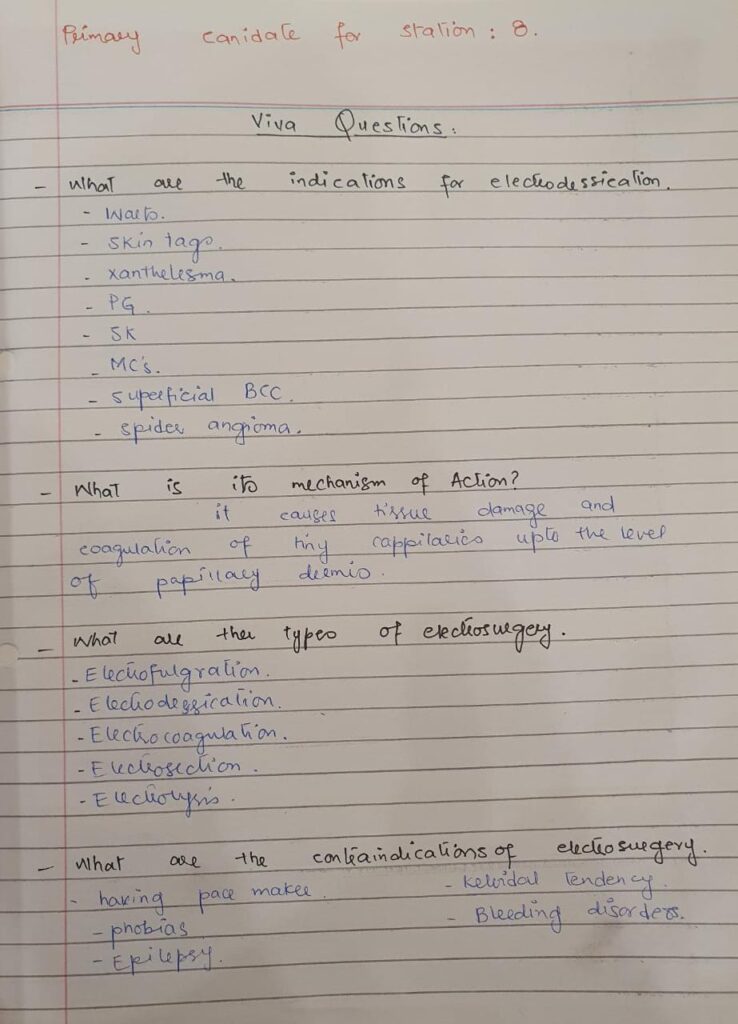

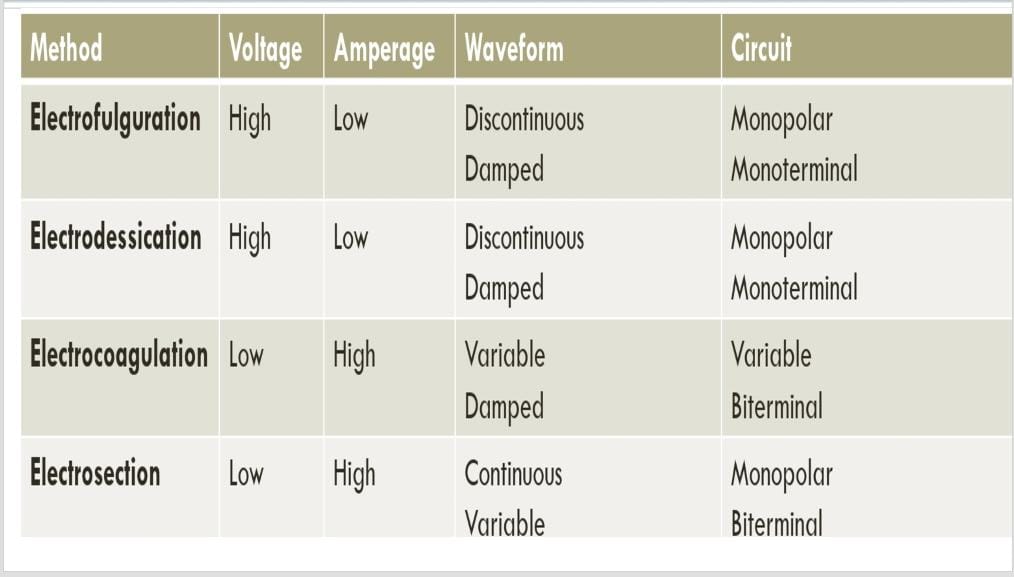

different target levels of each type of electrosurgery
Electrofulgration -very superficial / upto epidermis, thats why it heals w/o scarring
Electrodessication – upto papillary dermis / minimal scarring
Electrocoagulation – upper reticular dermis
Electrosection – to cut the tissue
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.