This is for the simple text copy pasting formate template for work file
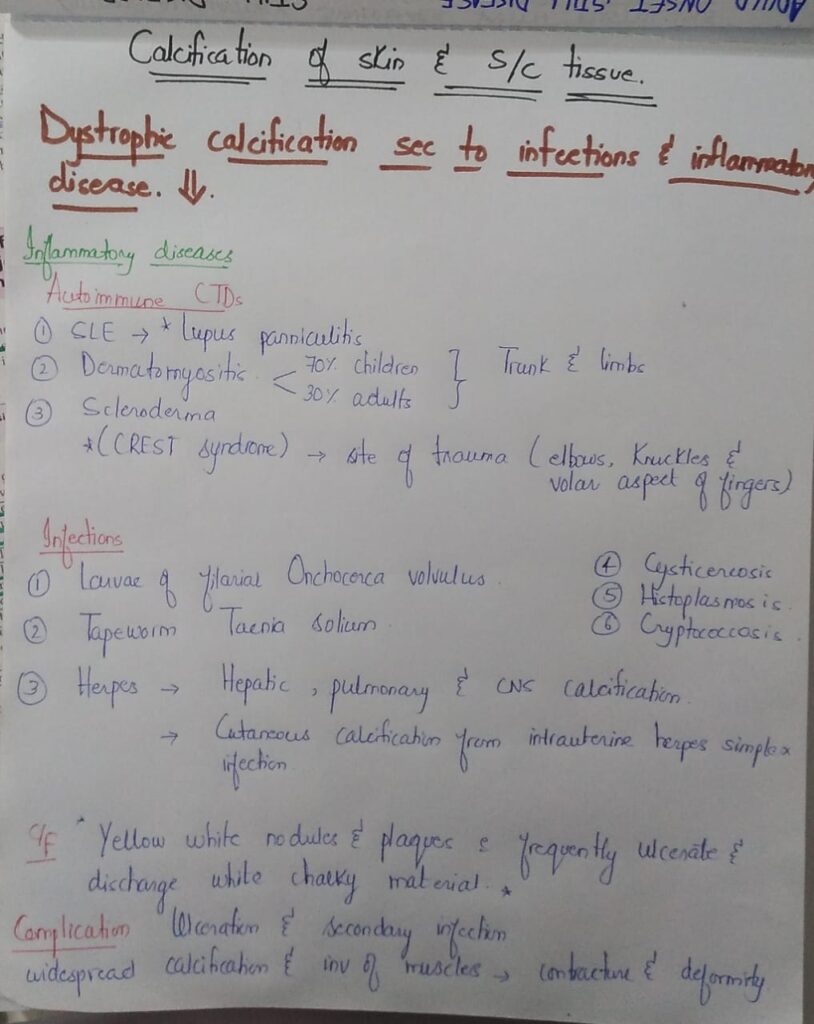

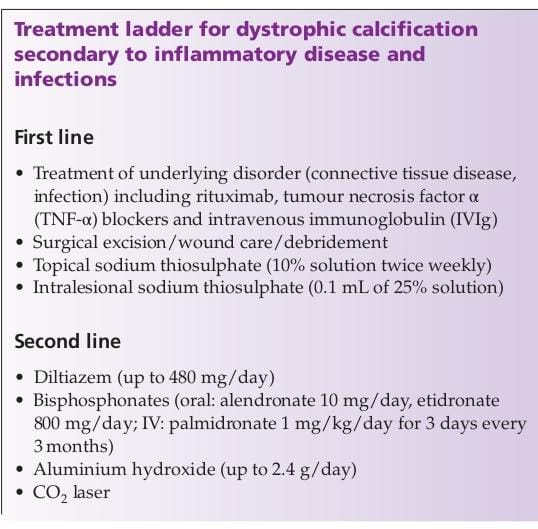



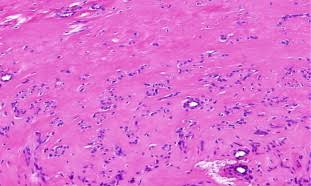
Calcinosis cutis
Metastatic calcification






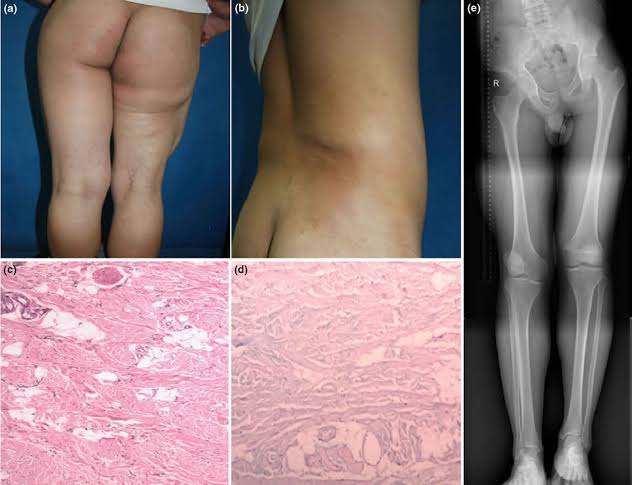
3️⃣ Eruptive xanthoma

4️⃣ Plane xanthomas
Xanthelasmas

Plane xanthoma

Palmar xanthoma

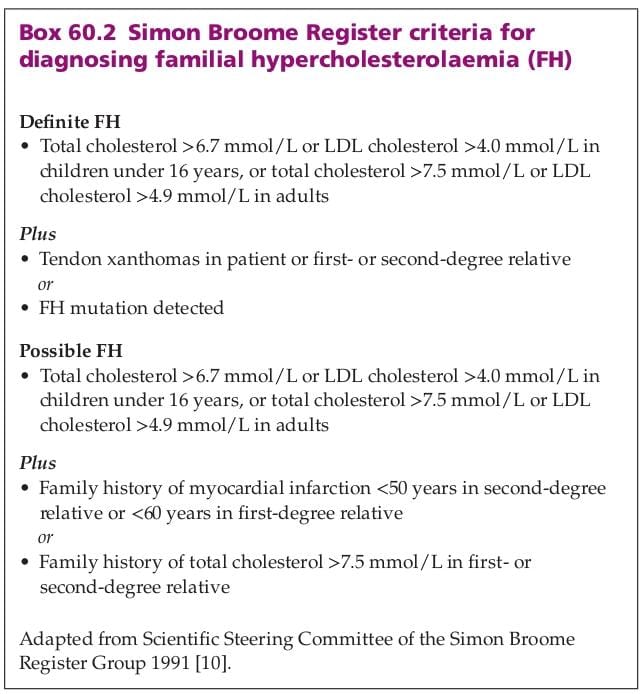
Familial hypercholesterolaemia

Type III hyperlipoproteinaemia

Type I hyperlipoproteinaemia
Type V hyperlipoproteinaemia
Type IV hyperlipoproteinaemia


Happy learning




Plasma cholesterol levels are normal




Diarrhea
Premature osteoprosis
Inc risk of CVD

Chenodeoxycholate




These transport plant sterols to facilitate their excretion.
Defects leads to raised levels of plant sterols ” Beta sitosterol” in body

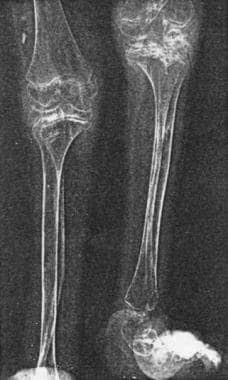
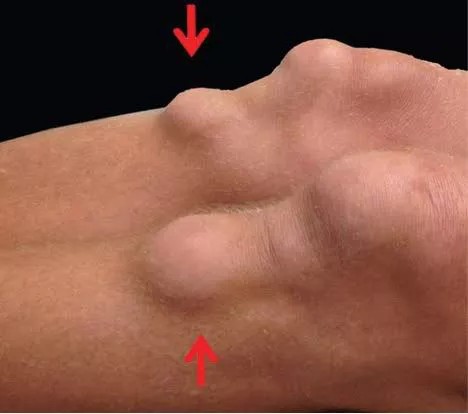
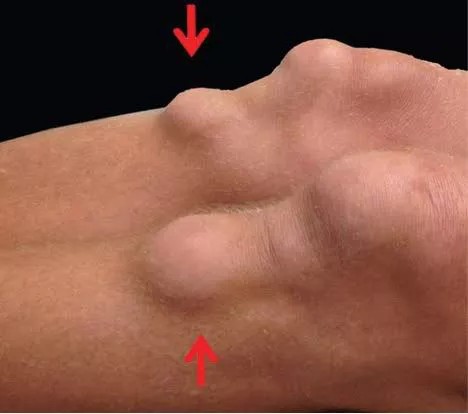
Tendon xanthomas
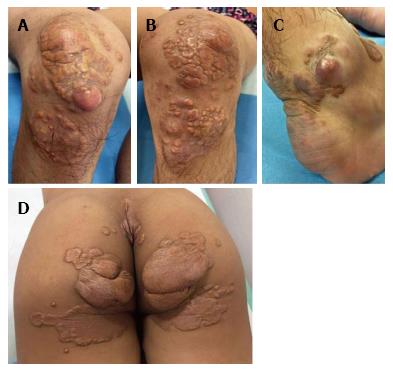
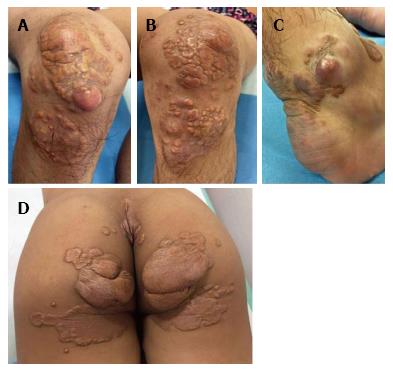
Tuberous xanthomas
Anaemia and thrombocytopenia
Arthritis
Inc risk of premature CVD

*Ezetimibe* reduces plant sterol levels
Type 1 lipoproteinemia nicotinic acid+ antioxidants
Type 2 statin , ezetimibe, bile acid sequestrant, mipomersen, Lopitamide, LDL apheresis
Type 3 Statin, Fibrate
Type 4 Statin
Type 5 Nicotinic Acid, Antioxidant, Fibrate
Type 1 and Type 5 have chylomicrons so same treatment
Type 2, 3, 4 all have LDL so same treatment
Type 2 is most serious so needs special measures like LDL Apheresis

1️⃣ Diabetes mellitus
Type I Increased HDL, LDL and VLDL and hence increased risk of CVD
Type II Decreased HDL, Normal LDL and Increased Tgs.
2️⃣ Chronic cholestasis
Increased Cholesterol
3️⃣Nephrotic syndrome
Increased cholesterol
4️⃣ Chronic renal failure
Increased Tgs
5️⃣Alcohol
Increased Tgs
6️⃣Systemic steroids
Increased LDL and HDL
7️⃣ Ciclosporin
Increased LDL cholesterol
8️⃣ Retinoic acid deriavatives
Increased Tgs



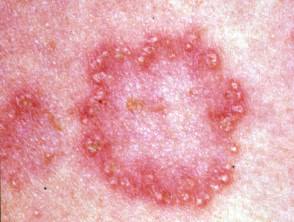
3️⃣ Eruptive xanthoma

4️⃣ Plane xanthomas
Xanthelasmas

Plane xanthoma

Palmar xanthoma

Familial hypercholesterolaemia

Type III hyperlipoproteinaemia

Type I hyperlipoproteinaemia
Type V hyperlipoproteinaemia
Type IV hyperlipoproteinaemia


Happy learning




Plasma cholesterol levels are normal




Diarrhea
Premature osteoprosis
Inc risk of CVD

Chenodeoxycholate




These transport plant sterols to facilitate their excretion.
Defects leads to raised levels of plant sterols ” Beta sitosterol” in body

Tendon xanthomas
Tuberous xanthomas
Anaemia and thrombocytopenia
Arthritis
Inc risk of premature CVD

*Ezetimibe* reduces plant sterol levels
Type 1 lipoproteinemia nicotinic acid+ antioxidants
Type 2 statin , ezetimibe, bile acid sequestrant, mipomersen, Lopitamide, LDL apheresis
Type 3 Statin, Fibrate
Type 4 Statin
Type 5 Nicotinic Acid, Antioxidant, Fibrate
Type 1 and Type 5 have chylomicrons so same treatment
Type 2, 3, 4 all have LDL so same treatment
Type 2 is most serious so needs special measures like LDL Apheresis

1️⃣ Diabetes mellitus
Type I Increased HDL, LDL and VLDL and hence increased risk of CVD
Type II Decreased HDL, Normal LDL and Increased Tgs.
2️⃣ Chronic cholestasis
Increased Cholesterol
3️⃣Nephrotic syndrome
Increased cholesterol
4️⃣ Chronic renal failure
Increased Tgs
5️⃣Alcohol
Increased Tgs
6️⃣Systemic steroids
Increased LDL and HDL
7️⃣ Ciclosporin
Increased LDL cholesterol
8️⃣ Retinoic acid deriavatives
Increased Tgs




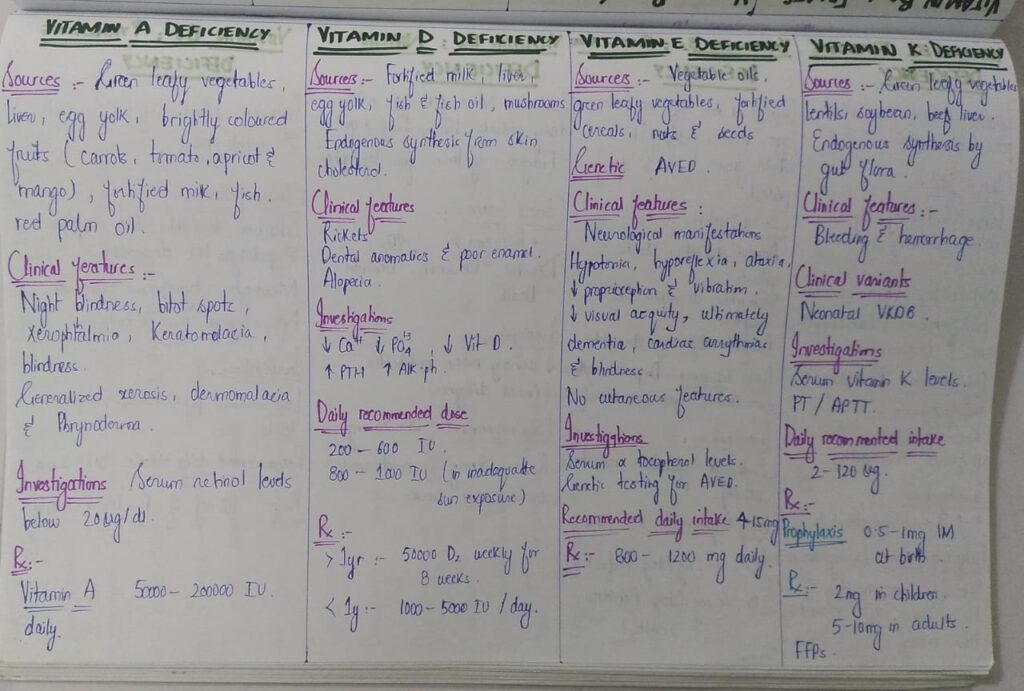
1️⃣ Vitamin A
Vitamin A deficiency

Vitamin A excess
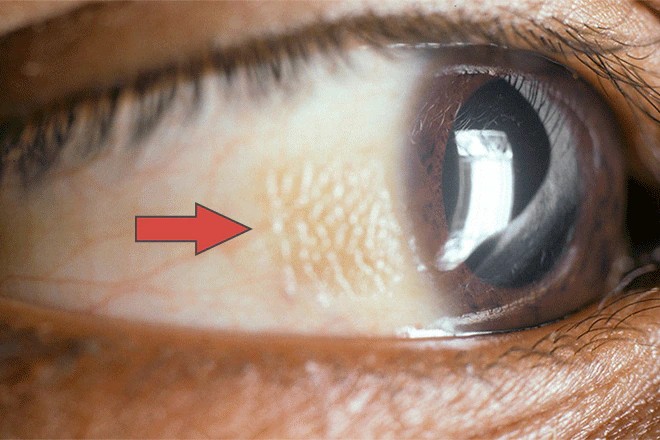
Bitot spots
Phrynoderma

Carotenaemia

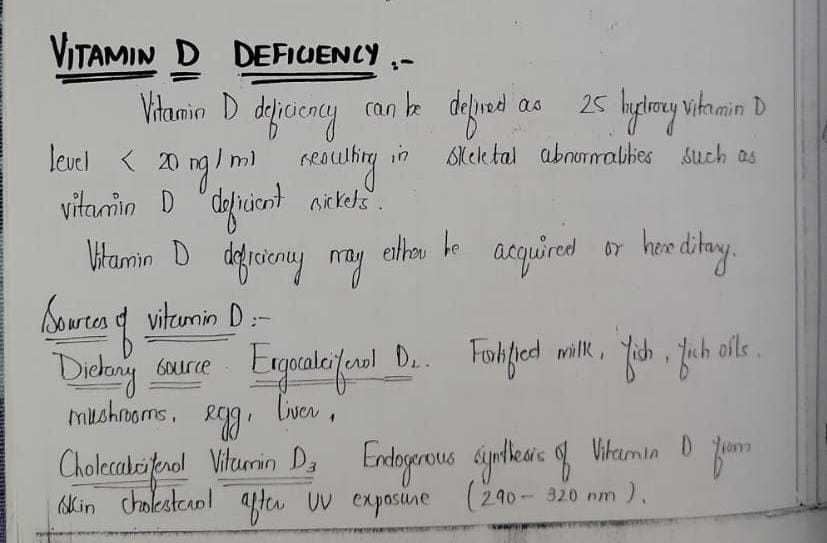
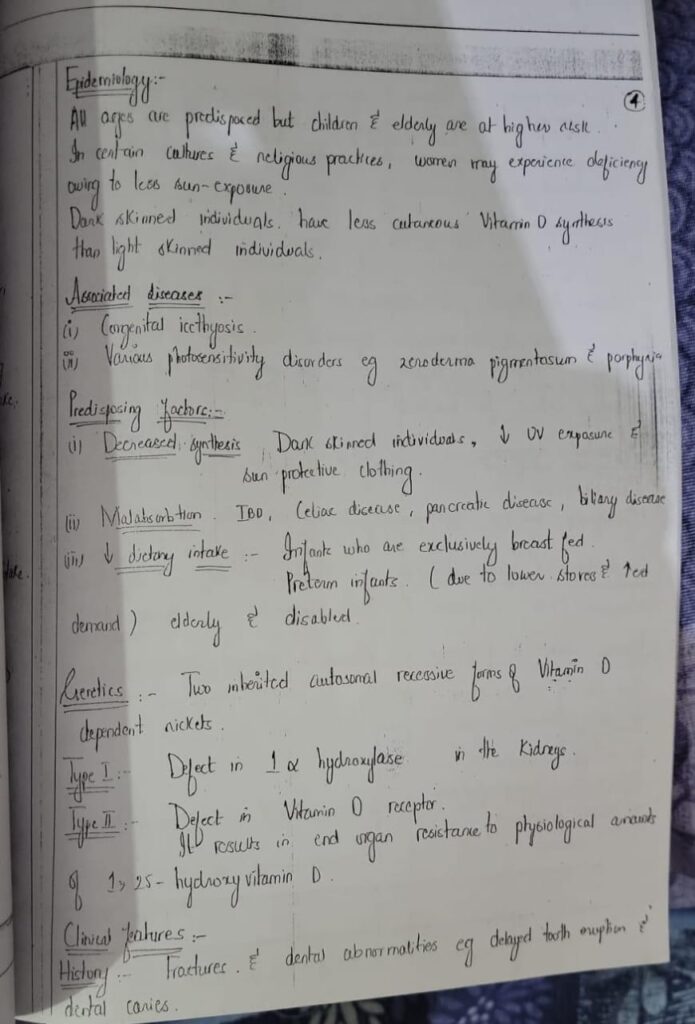
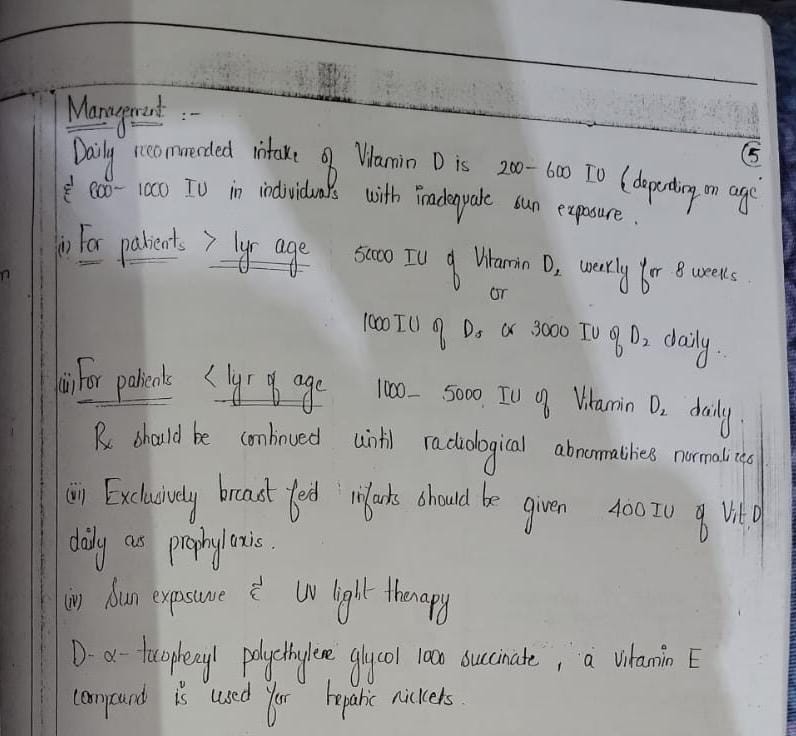
2️⃣ Vitamin D
Vitamin D deficiency


3️⃣ Vitamin E
Vitamin E deficiency
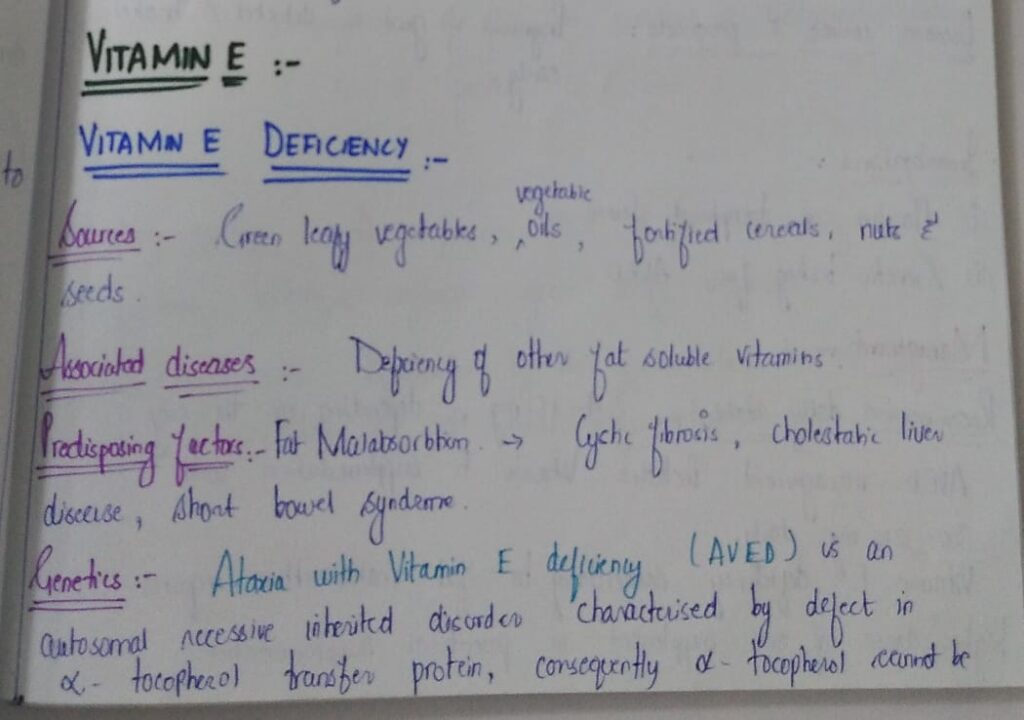
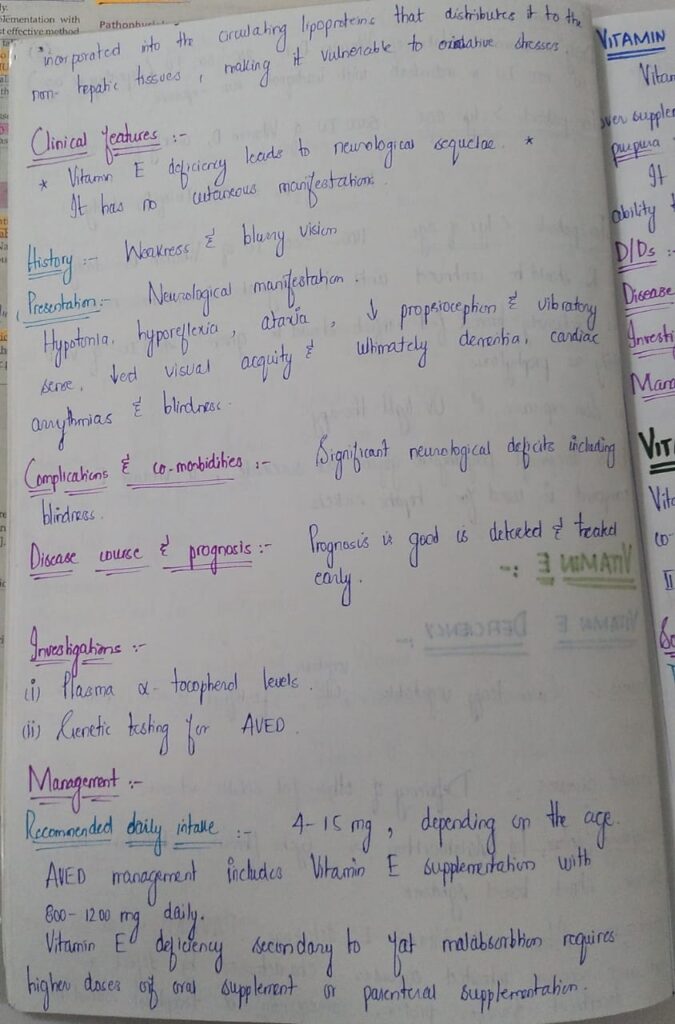
Vitamin E excess

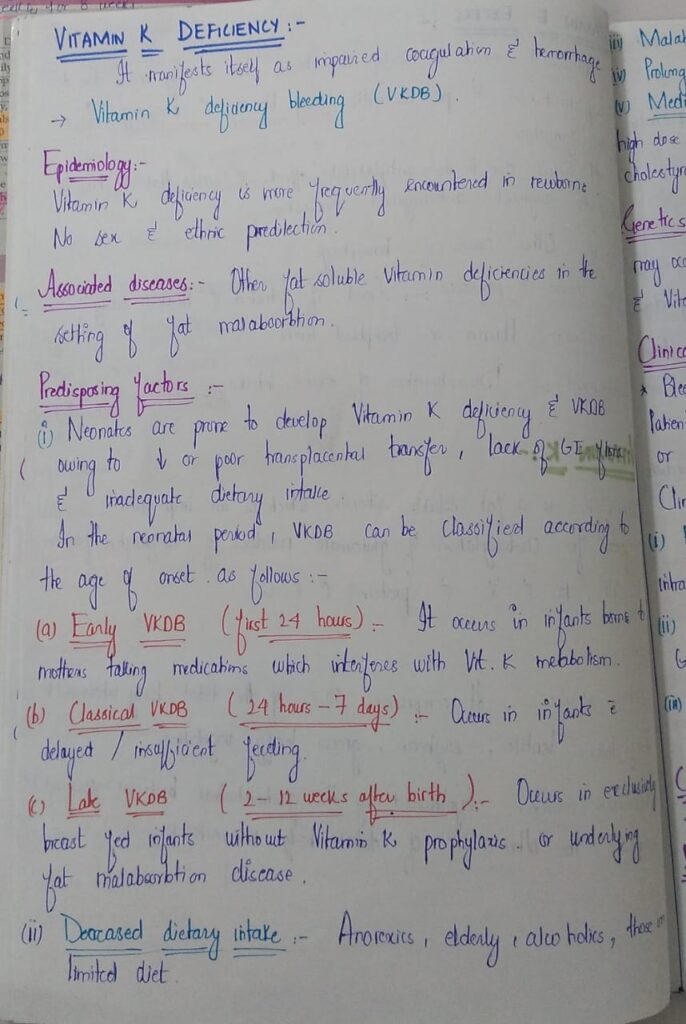
4️⃣ Vitamin K






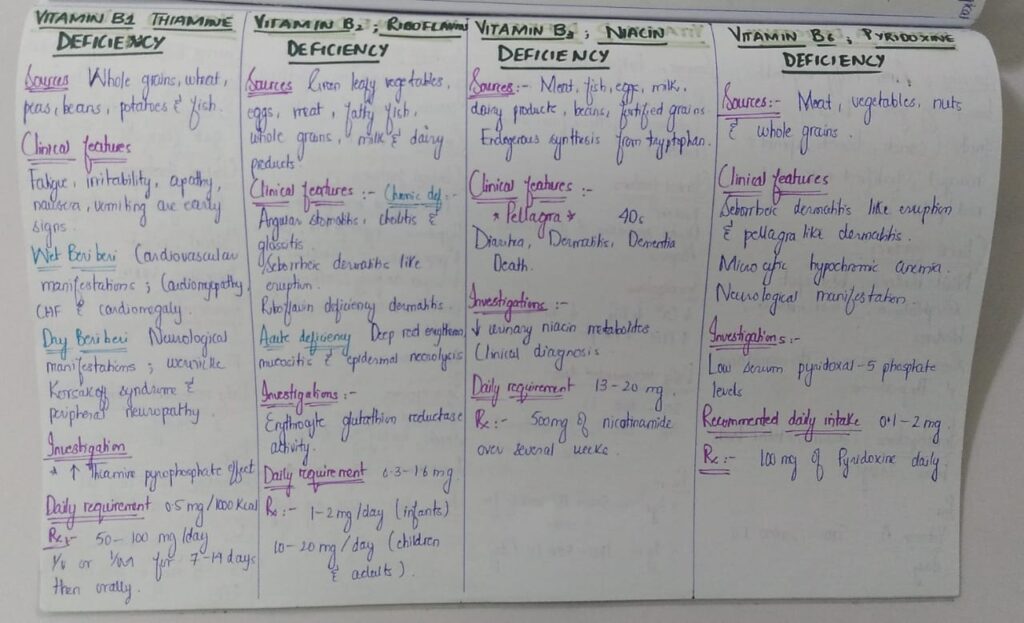
5️⃣ Vitamin B1/ Thiamine deficiency

6️⃣Vitamin B2 / Riboflavin deficiency

7️⃣ Vitamin B3 / Niacin deficiency
Pellagra


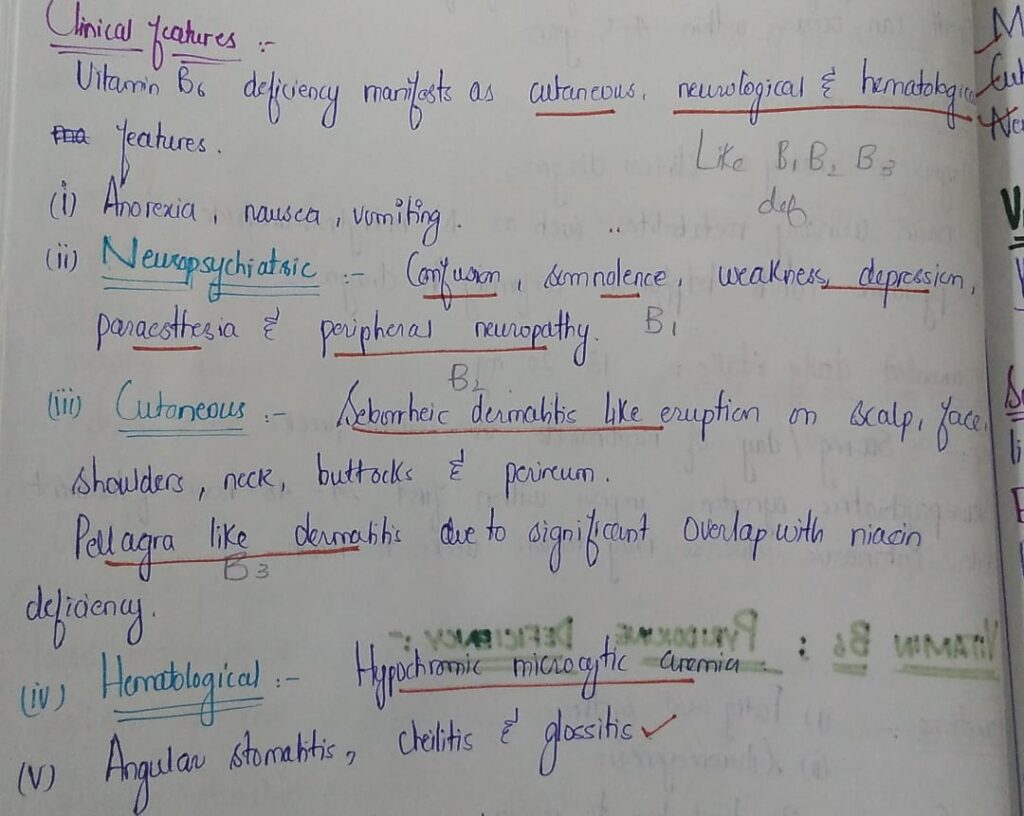
8️⃣ Vitamin B6 / Pyridoxin deficiency
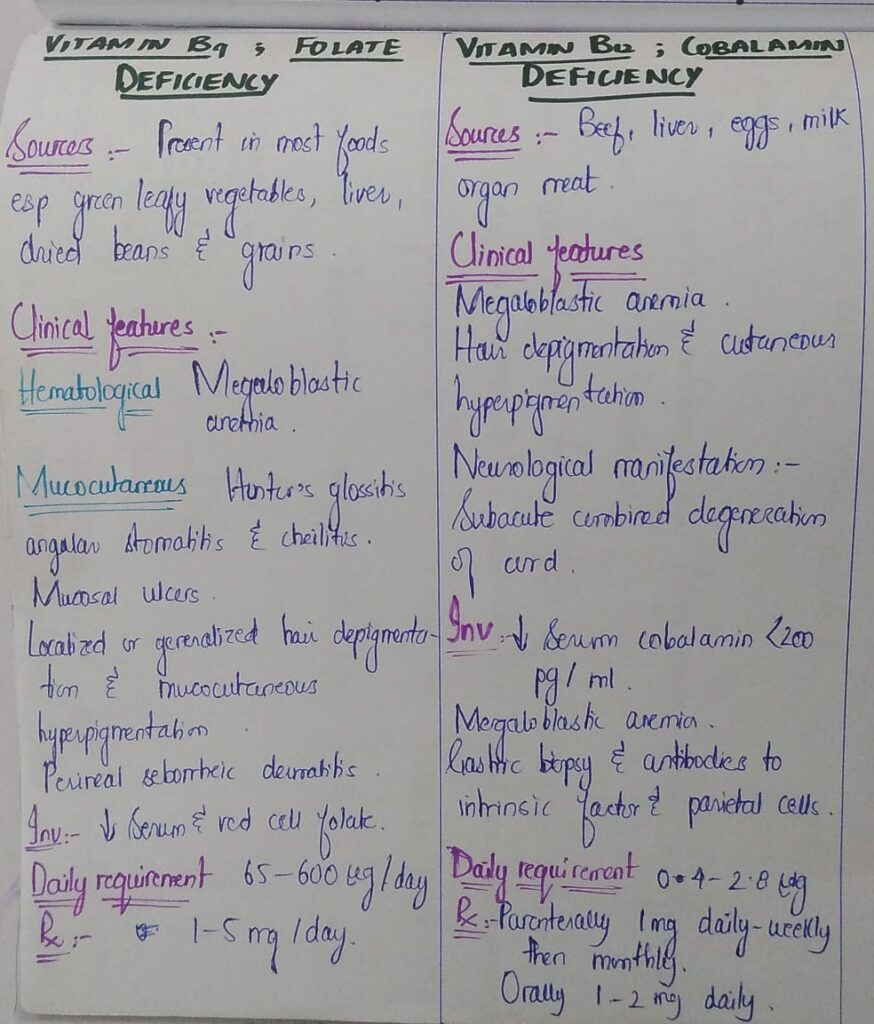
9️⃣ Vitamin B9 / folate deficiency






🔰Vitamin B7/ Biotin deficiency


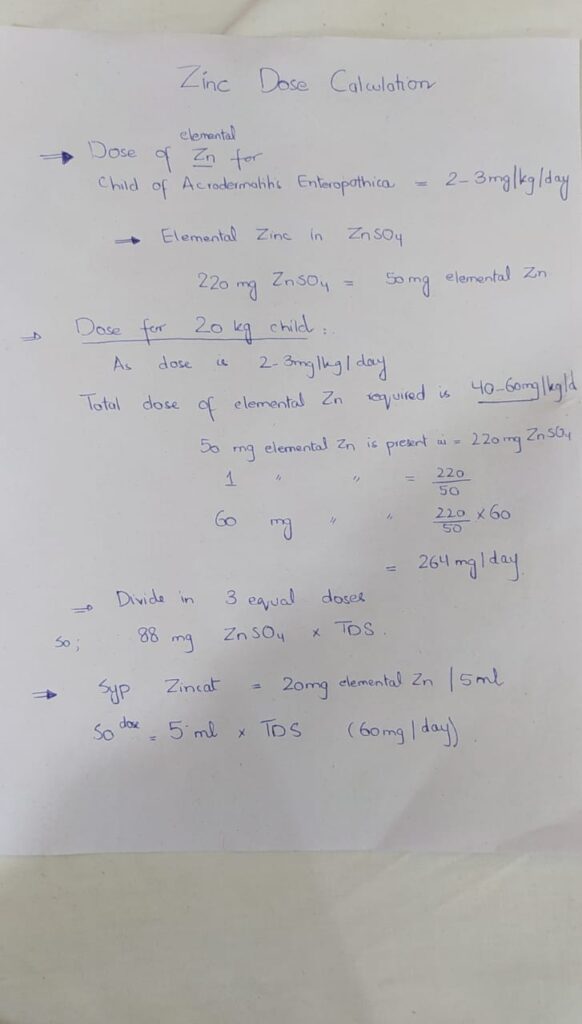
ZINC DEFICIENCY
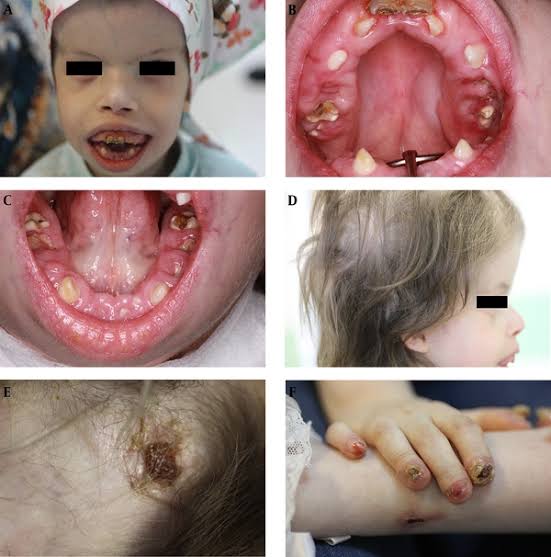
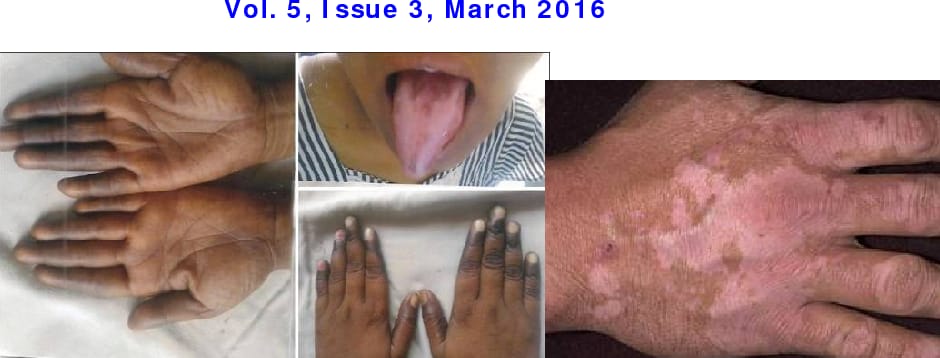
Acrodermatitis enteropathica👇🏻



🔰 Iron deficiency👇🏻
🔰 Copper deficiency


🔰 Selenium deficiency / Keshan disease
🔰 Summary👇🏻



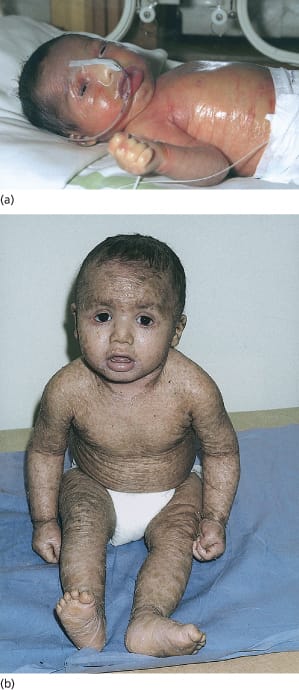
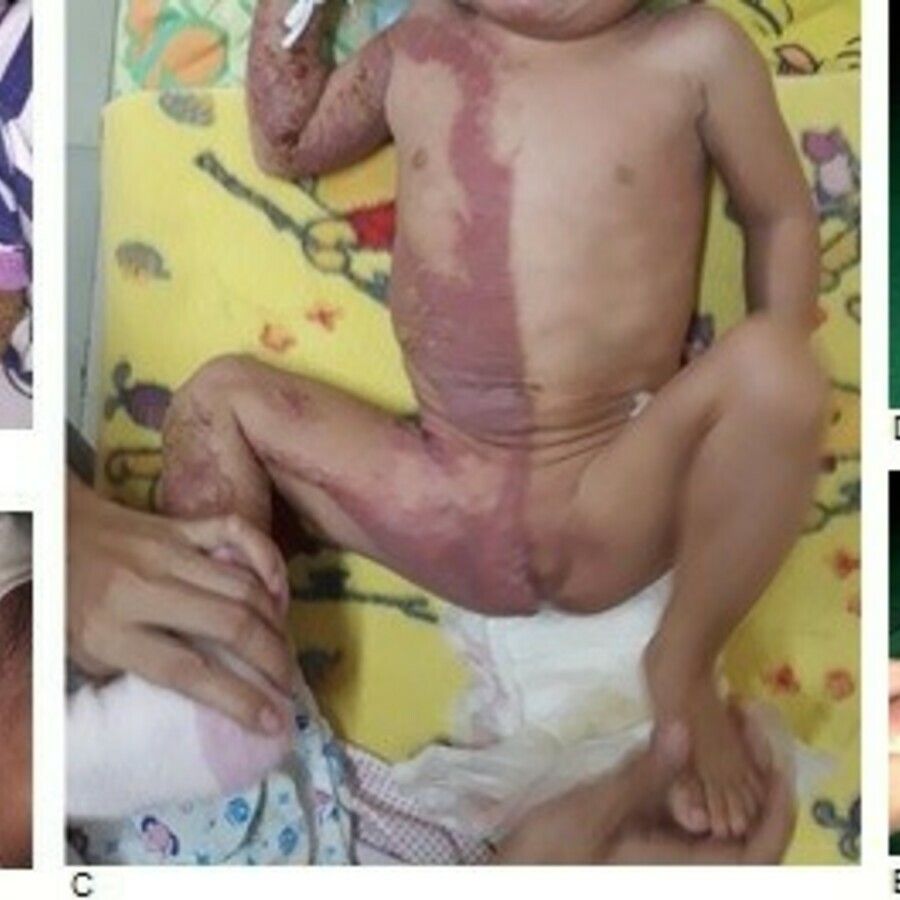
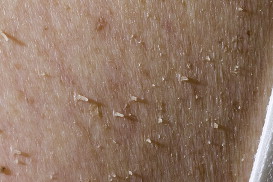
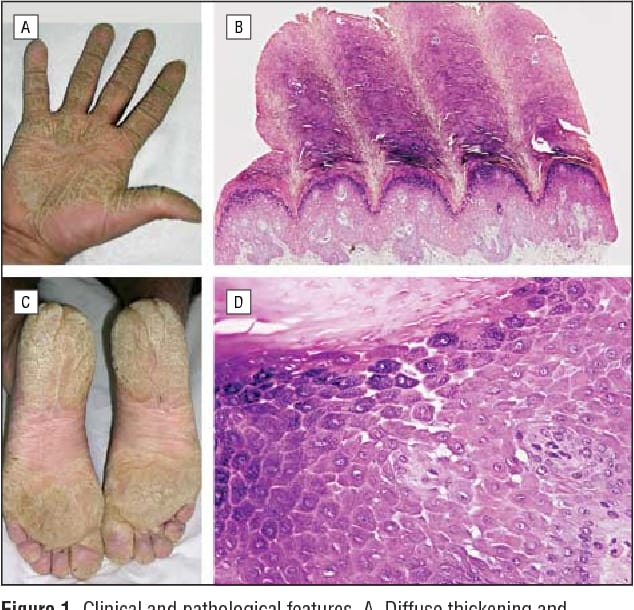
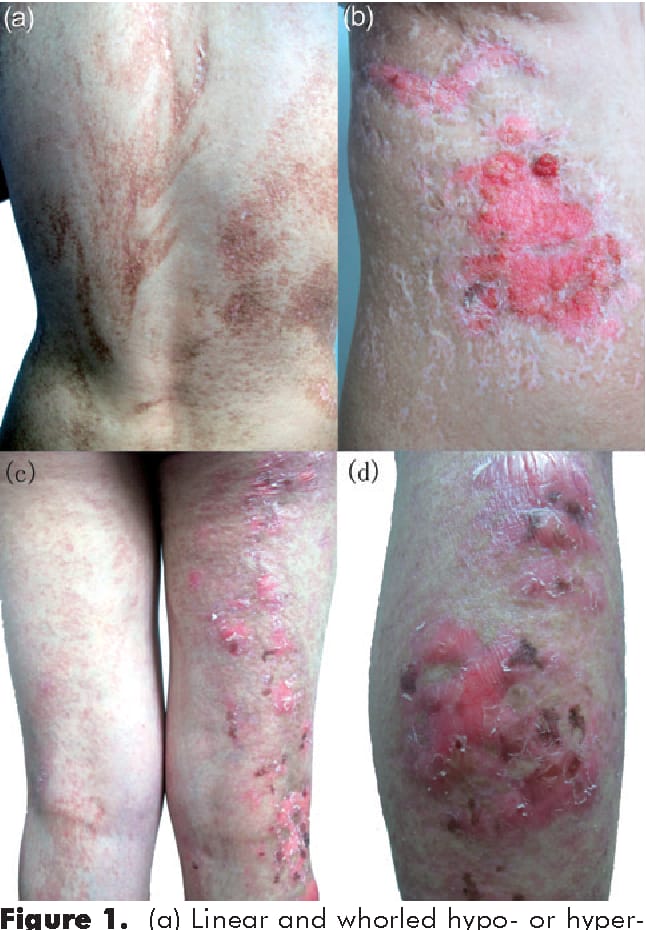
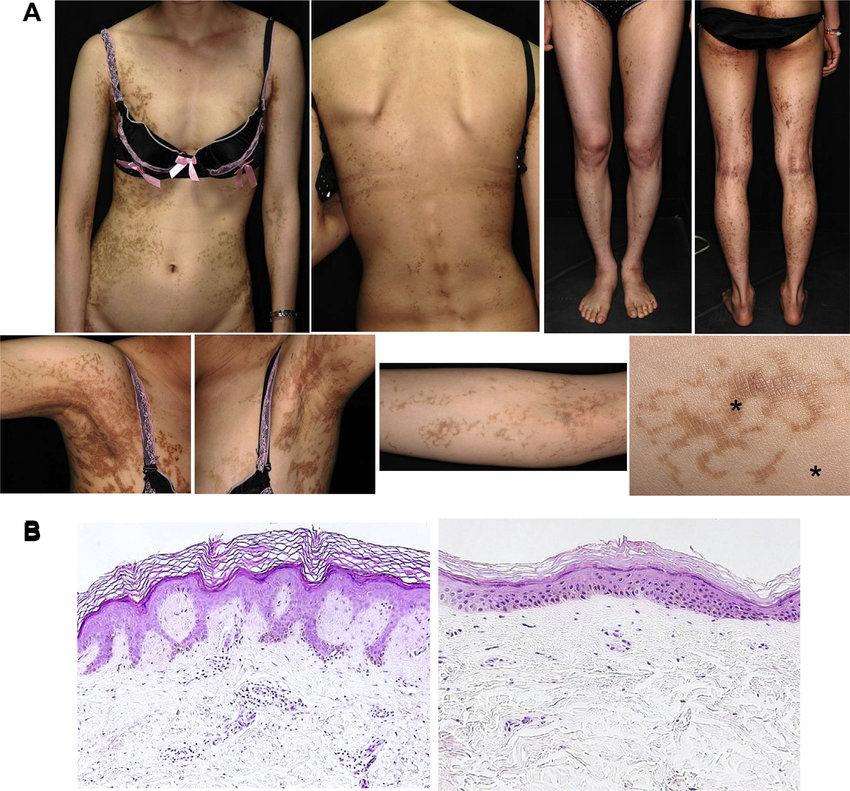
AUTOSOMAL RECESSIVE CONGENITAL ICHTHYOSIS
1. Harlequine ichthyosis

Collodion baby and self improving congenital ichthyosis
IV : light Grey scales covering extensor, always sparing flexures ,palmo plantar hyperlinearity
RXLI: large thick dark brown to yellowish brown crust.
Dirty look of neck and sides of trunk.
flexures usually involved
Palm and soles spared.
Lamellar :thick ,plate like dark brown crust involving whole body
Maintain hydration humidity maintain 60 to 80 percent decrease every 3 to 4days
Emolient
50%LP 50WSP
Taking bath with pinch of sodabicarb
Acetretin
Eye care artificial tears
For wounds antibacterials fudic cream
30min in taking bath and remove scale and 30min of applying emolients
*1* emolients : high water content ointments.. keratolytics urea and lactic acid ,bathing daily with sodium bicarbonate additive systemic therapy . isotretinoin or acetretin *.. Genetic* *counselling* of parents
Retinoids also improve sweat gland function in these patients
To prevent icthyosis:
Topical tazarotene gel
Topical n acetyl cysteine.
Once developed :
Artificial tears
Surgical correction
To prevent icthyosis:
Topical tazarotene gel
Topical n acetyl cysteine.
Once developed :
Artificial tears
Surgical correction
In management plan
Ist general
Emollients regular with keratolytics
Systemic treatment retinoids for harlequin icthyosis
Special aspects of treatment
Eyes lubricants, taz gel for ectrobion
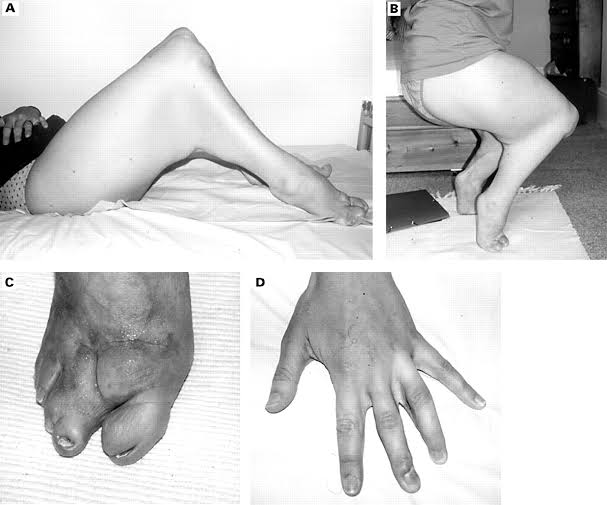
Physiotherapy for contractures
Vit d supplements
Treat superinfections
How will u give retionids in small child?
0.5 MG/kg dose .
Freezing capsule and then cutting and dissolving in honey or olive oil.
Bathing suit ichthyosis

Lamellar ichthyosis and Congenital ichthyosiform erythroderma







KERATINOPATHIC ICHTHYOSIS

ERYTHROKERATODERMA 👇🏻
Erythrokeratoderma variabilis

Progressive symmetric erythrokeratoderma

OTHER NON SYNDROMIC FORMS OF ICHTHYOSIS👇🏻
SYNDROMIC ICHTHYOSIS👇🏻
X LINKED SYNDROMIC ICHTHYOSIS ASSOCIATED WITH CHOLESTEROL BIOSYNTHESIS👇🏻
- Conradi Hunermann Happle syndrome👇🏻

This is mcq of Conradi–Hünermann–Happle syndrome ansswer should be E. Basic defect in cholestrol biosynthesis

CHILD syndrome👇🏻
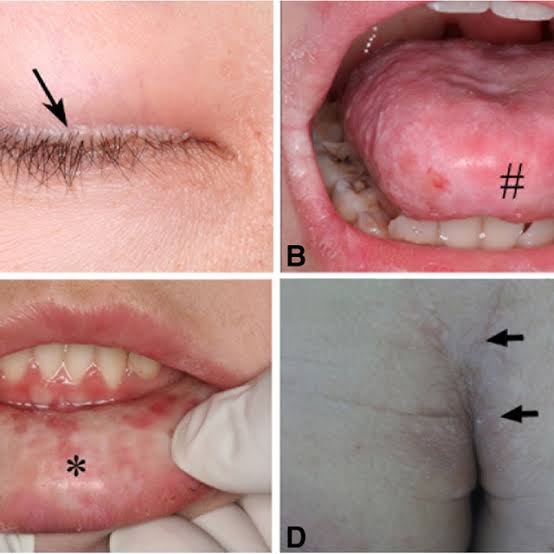
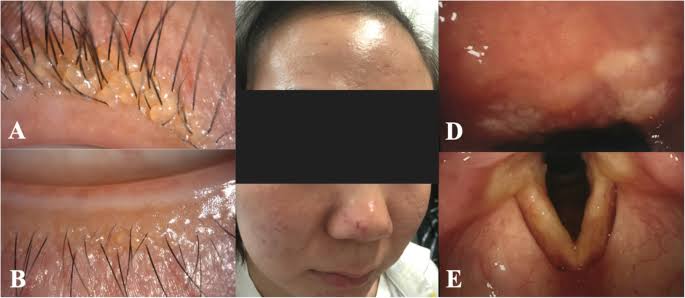
Ichthyosis follicularis-atrichia-photophobia syndrome 👇🏻
IFAP
✅for diagnostic purpose… u have to pluck the hair ?or cut ?
And
Which Site????
Cut. Hair will break on an attempt to pluck

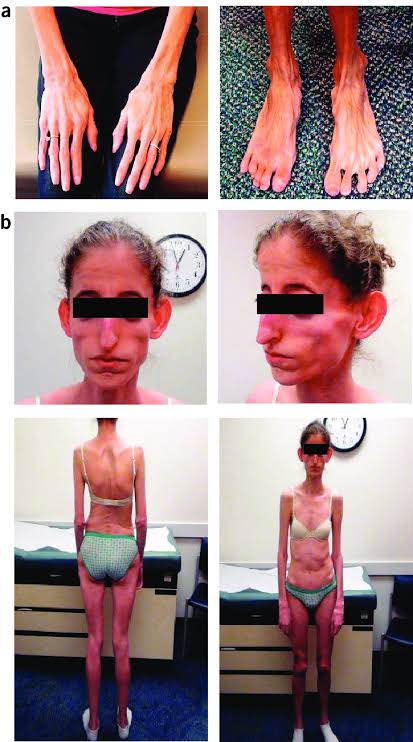
SAM syndrome (severe dermatitis-multiple allergies-metabolic wasting)
PEELING SKIN SYNDROMES👇🏻
Type A Peeling skin syndrome👇🏻
Type B Peeling skin syndrome👇🏻
Acral peeling skin syndrome👇🏻
Ichthyosis prematurity syndrome👇🏻
🔰 NEURO-ICHTHYOTIC SYNDROMES👇🏻
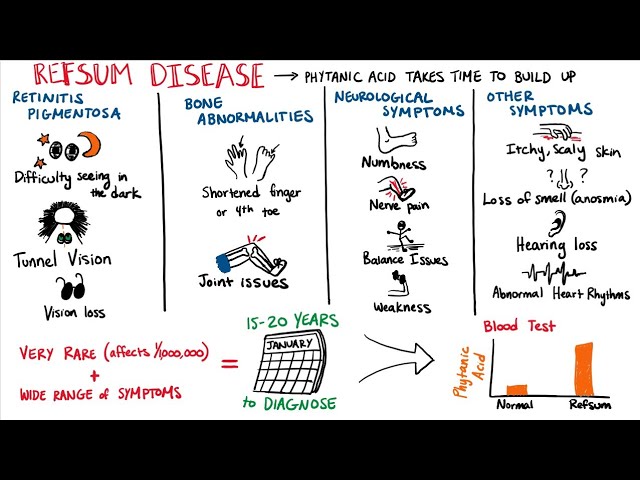
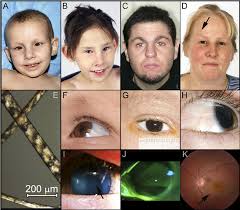
Refsum disease👇🏻
Multiple sulphatase deficiency👇🏻
Sjogren-Larsson syndrome👇🏻

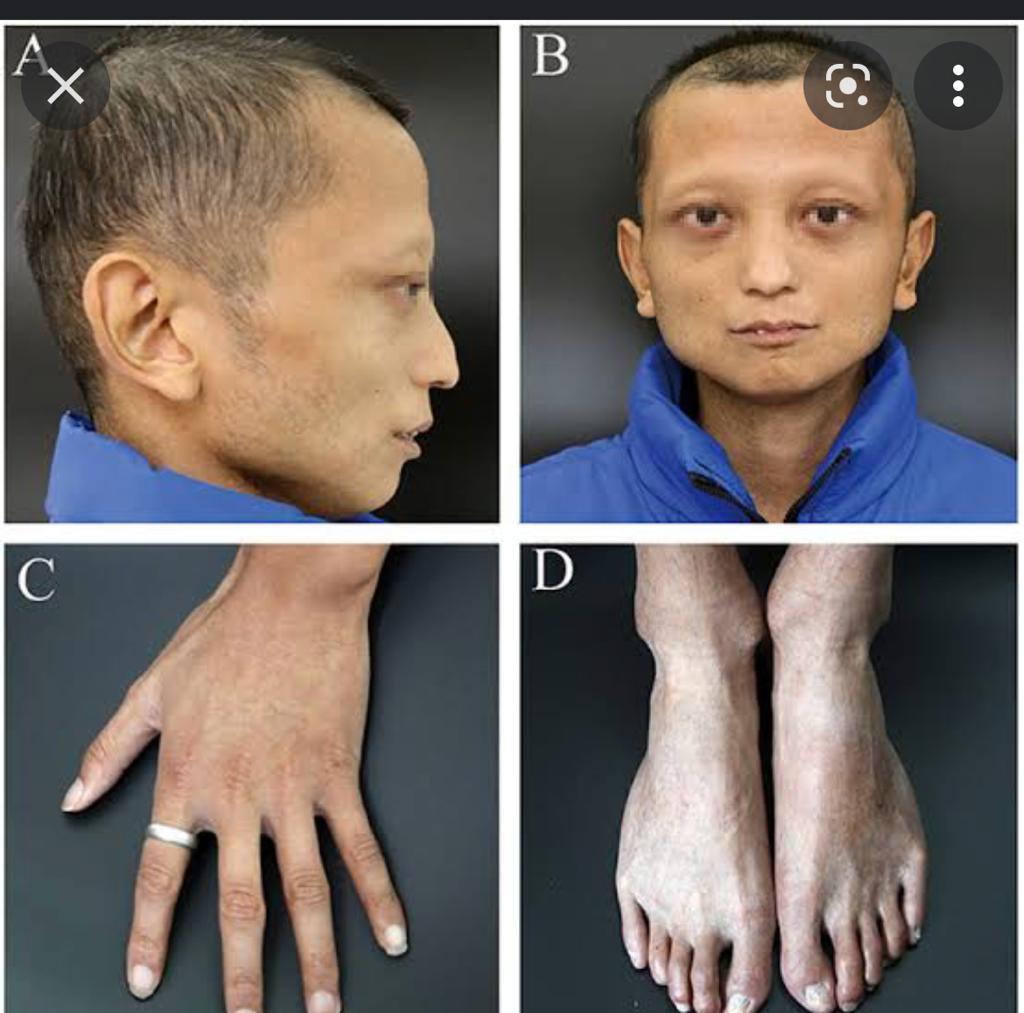
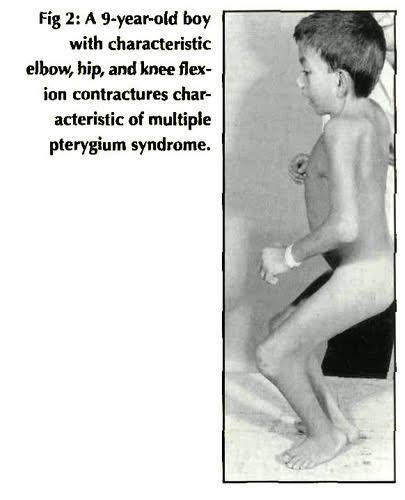
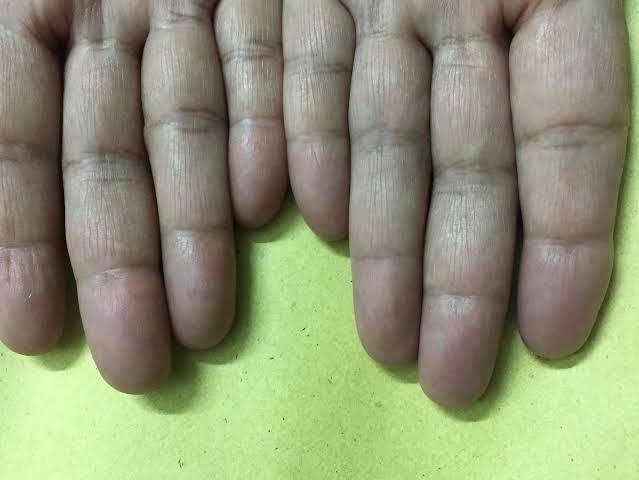
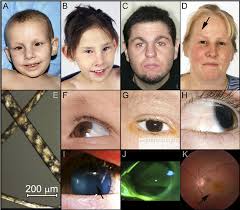
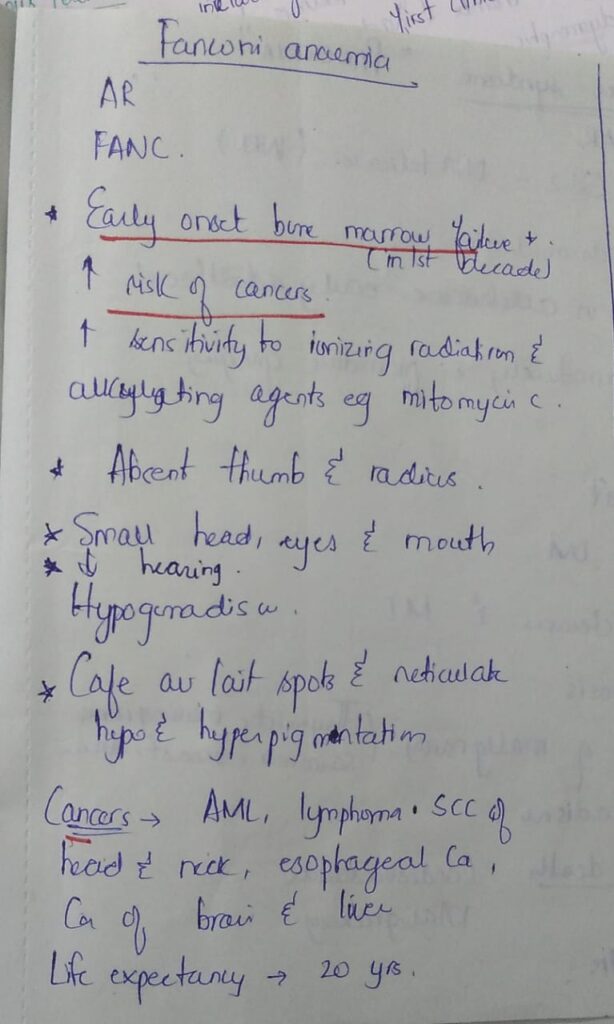
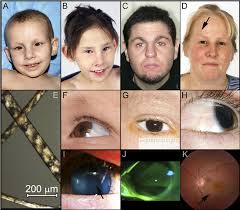
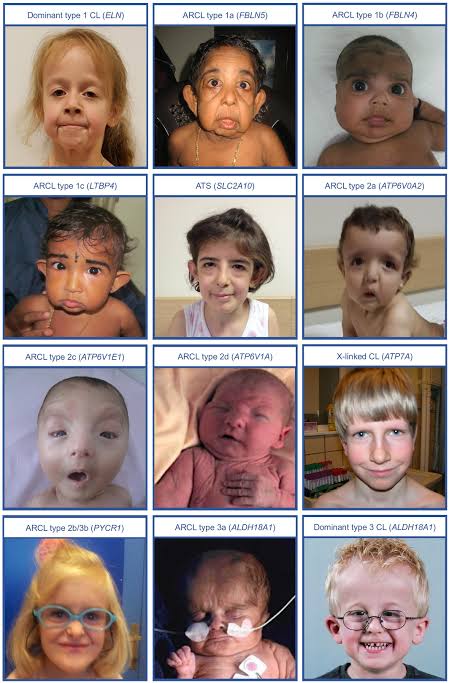
🔰 Important
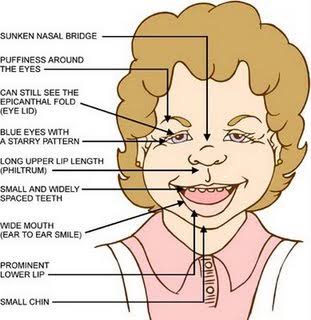
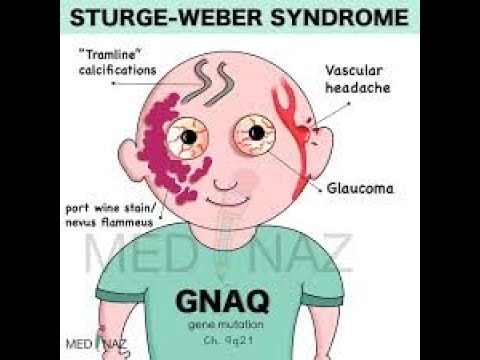
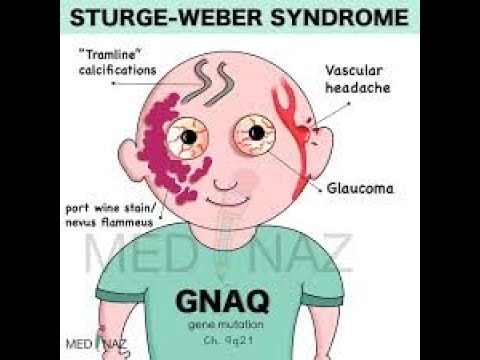
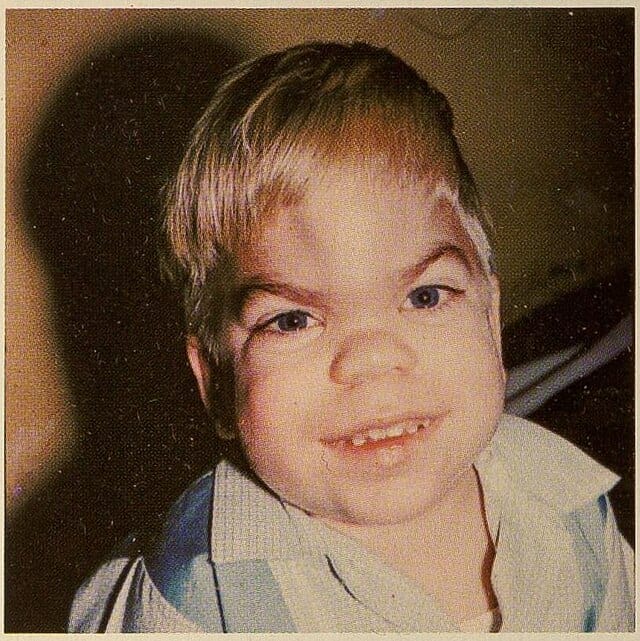
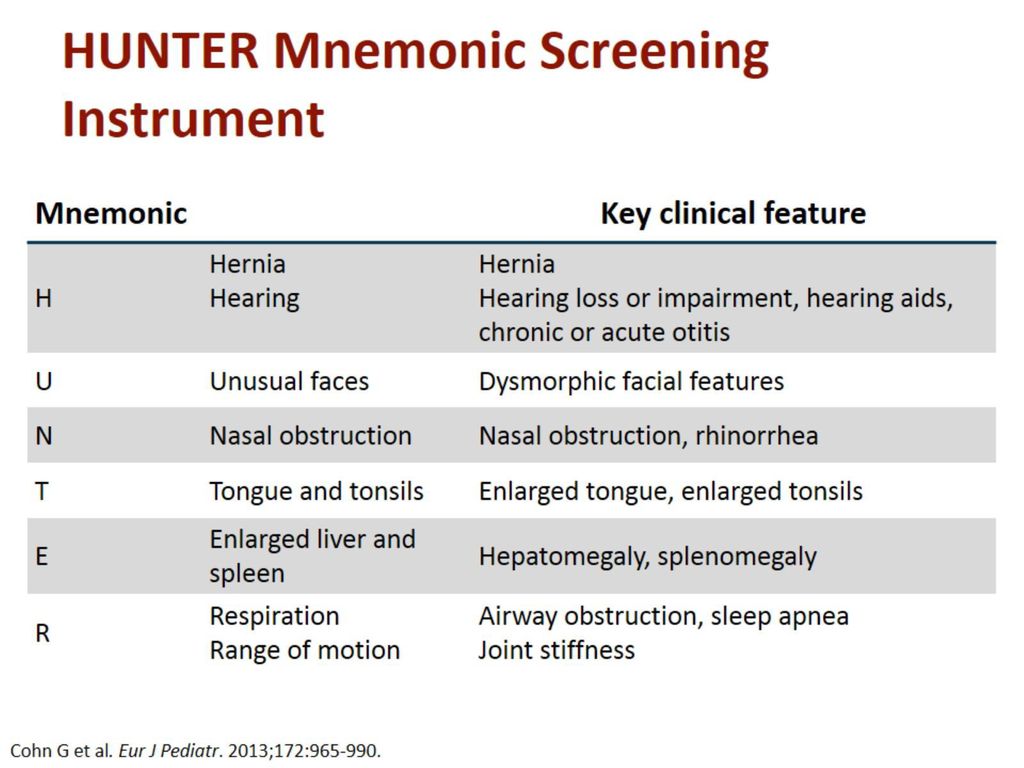
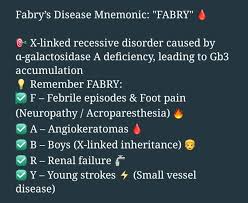
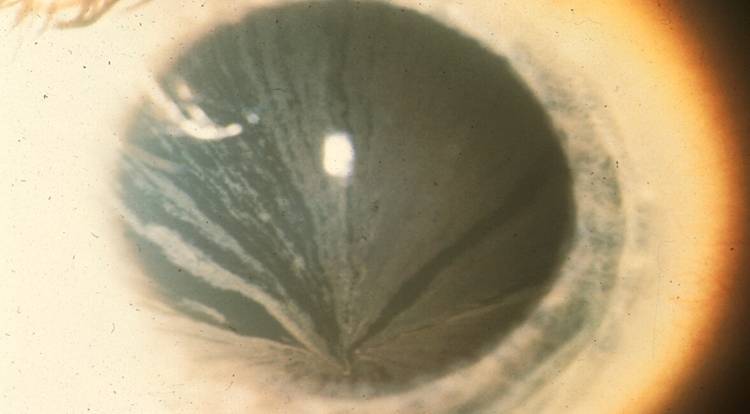
These images of syndromic forms of genetic diseases are really imp from toacs points of view. U may get such images in clinical slides for identification and other related questions.
Sometimes they may give these images along with a scenario in theory exam as well.
So practice them well.
KID syndrome (keratitis-ichthyosis-deafness)🏻

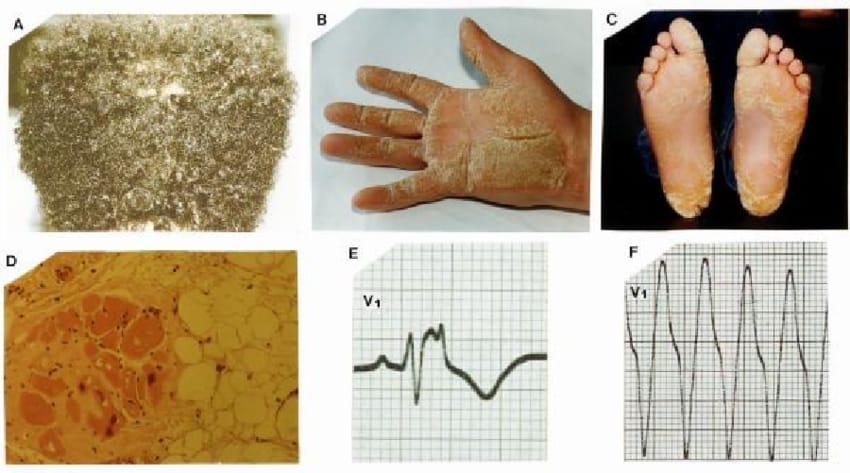
Neutral lipid storage disease with ichthyosis👇🏻

Trichothiodystrophy
Multiple minute digitate hyperkeratosis👇🏻
Keratolytic winter erythema👇🏻

Perforating keratotic disorders👇🏻

🔰 ACQUIRED KERATODERMAS
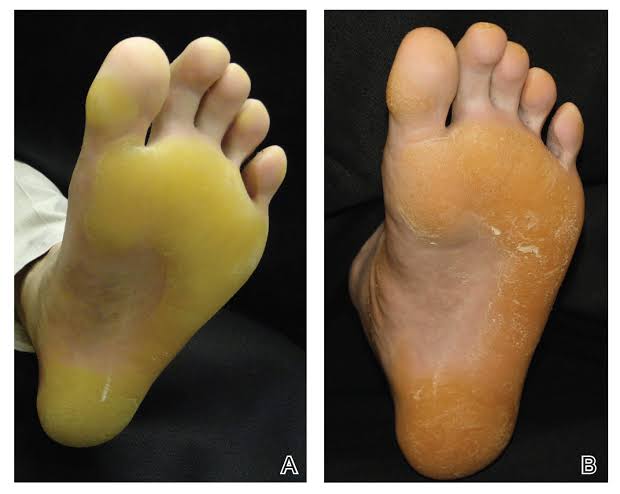
1️⃣ Keratoderma climactericum(Hauxthausen disease)👇🏻

2️⃣ Acquired ichthyosis
3️⃣ Pityriasis rotunda👇🏻


🔰 Veryyy imp topic from exam point of view
Non epidermolytic PPK
Mal de meleda

Loricrin keratoderma
Inherited skin diseases associated with pseudo ainhum
Striate/ focal PPK

Punctate PPK

Spiny keratoderma

Marginal papular keratoderma
Cole disease

Transient aquagenic keratoderma


🔰 Syndromic PPK
🫀PPK and cardiomyopathy
1. Naxos syndrome

🔰 One of the most imp topics of this chap👆🏻
Carvajal Huerta syndrome
🦻🏼 PPK AND HEARING IMPAIRMENT
1️⃣ Vohwinkle syndrome


2️⃣ Bart pumphrey syndrome
3️⃣ Mitochondrial PPK with hearing impairment
🔰 PPK and cancer
1️⃣ Huriez syndrome


2️⃣ Howel Evans syndrome
PPK , sex reversal and cancer
- Odonto-onycho-dermal dysplasia


🔥 PPK in ectodermal dysplasia and related diseases👇🏻
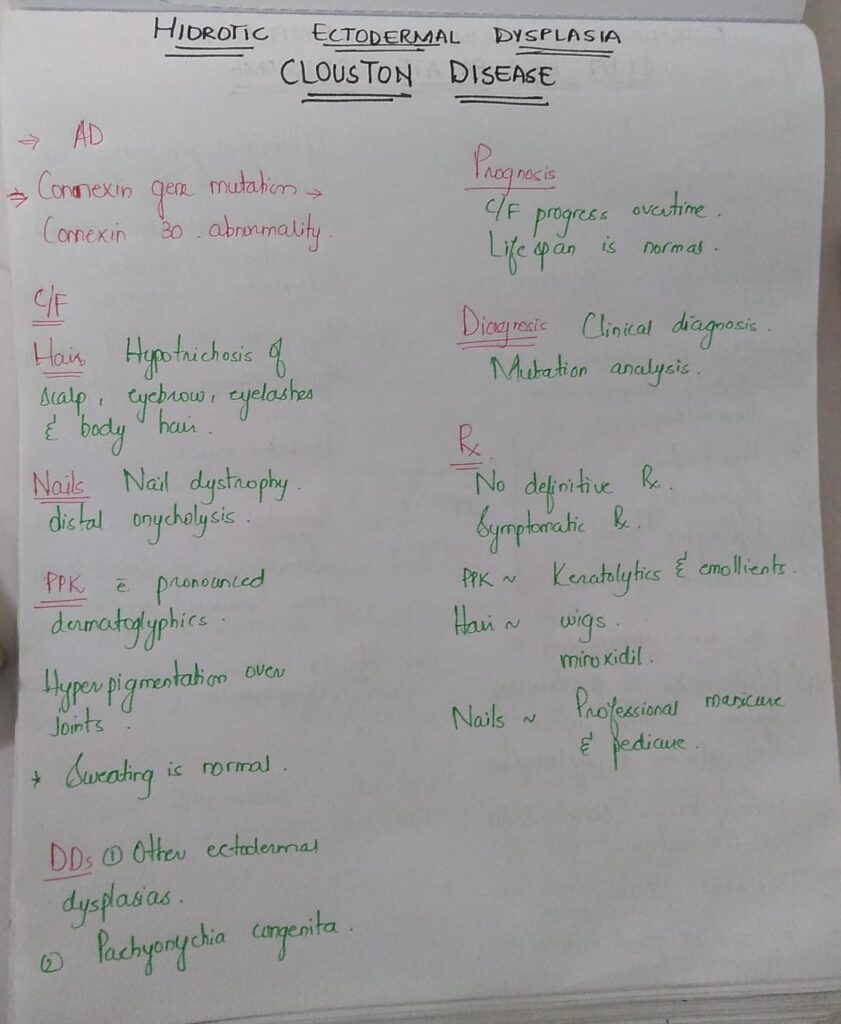
1️⃣ Clouston syndrome(Hidrotic ectodermal dysplasia type 2)

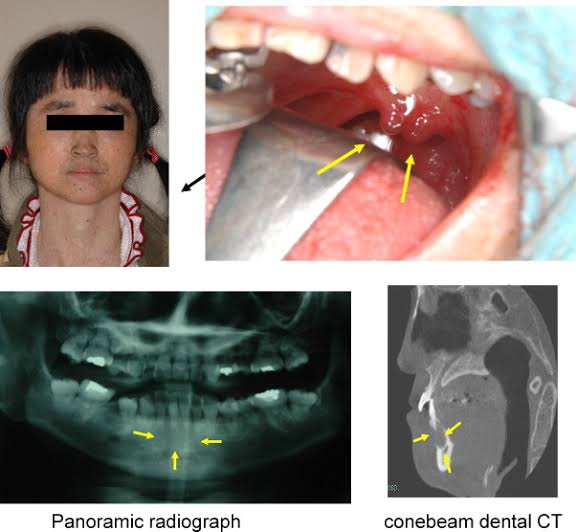
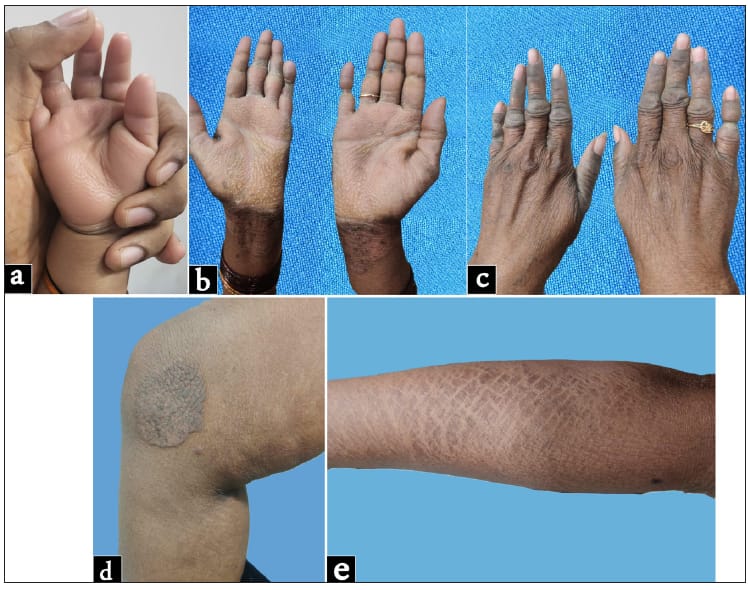
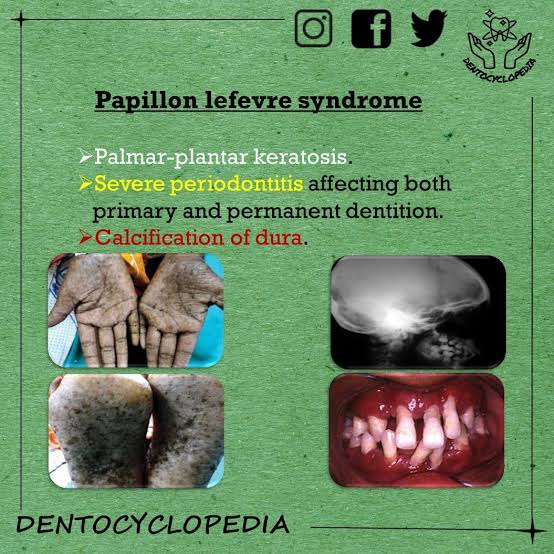
2️⃣ Papillon Lefevre syndrome
Haim munk syndrome*

Olmsted syndrome

PPK WITH OPHTHALMIC MANIFESTATIONS👇🏻
ACQUIRED KERATODERMAS
Flegel disease





🔰 *Important note for today*
Ichthyosis and ppk are 1 of those important chaps which are must to come in theory as well as clinical exam including clinical slides.
Since the chap is very lengthy and needs repeated revision to memorize it, imp tip here is to start reading from rooks and then narrow it down to the tables and flow charts.
I have shared a ppt in which all of it has been summarised beautifully.
U can keep it even for last day revision.
Listen to all the detailed voice notes for concepts and then revise it only from tht ppt.
Happy learning😁
🔰very imp and compact table for ichthyosis and ppk
ichthyosis,syndromes and ppk
Severity assessment
Complications
Disease course, investigations and management
10th edition👆🏻
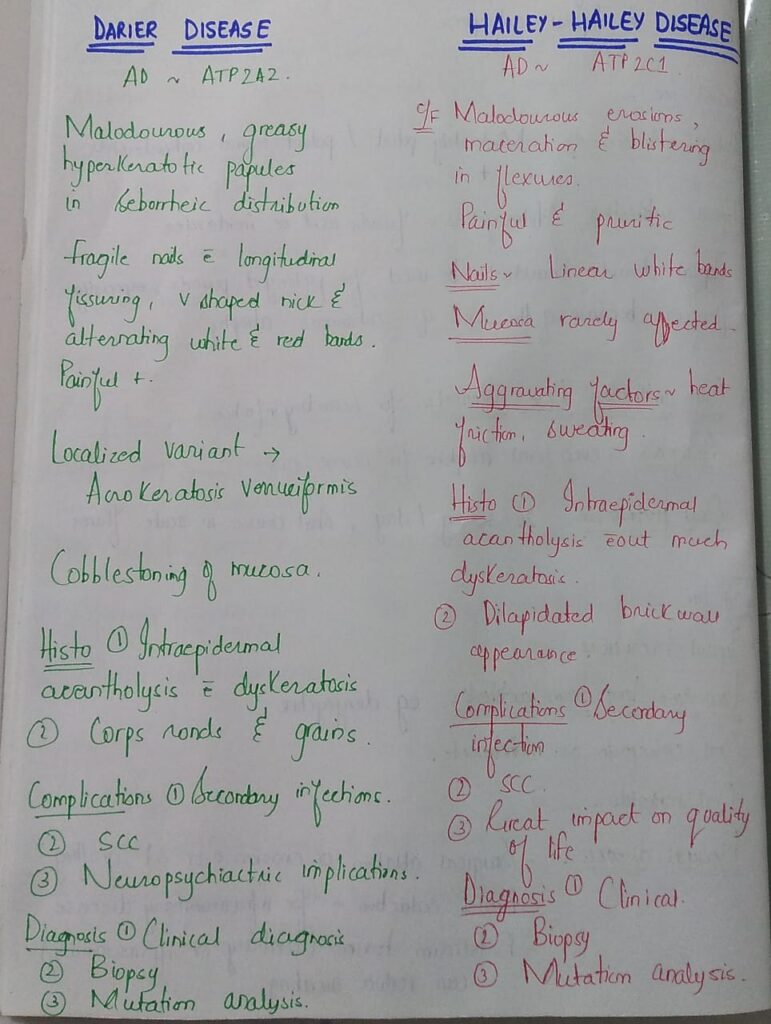
🔰 Hailey hailey disease
Clinical features
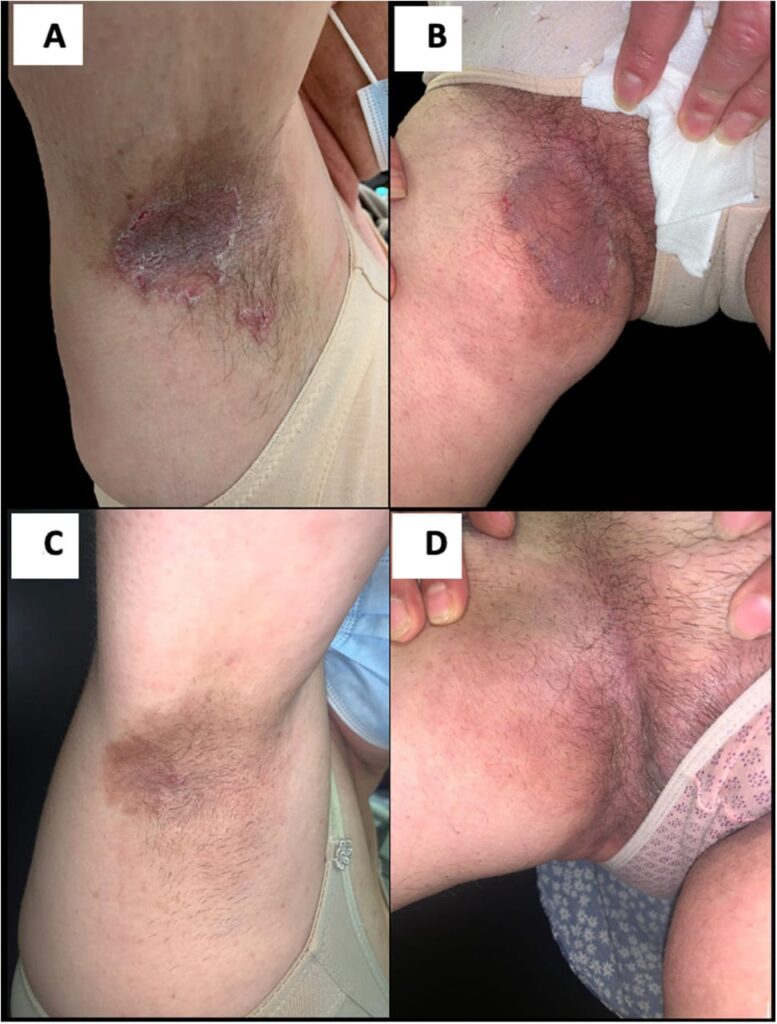

Dds👆🏻
Complications
Inveatigations and treatment
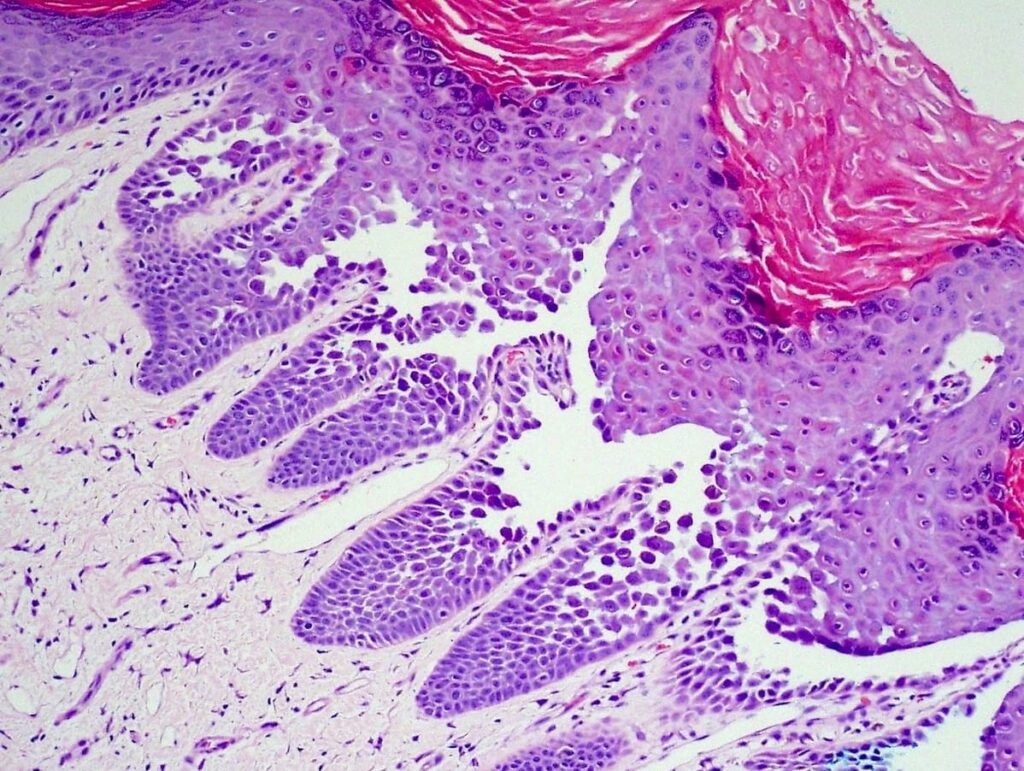
10th edition
🔰 Summary👇🏻
🔰 Important tip for this chap👇🏻
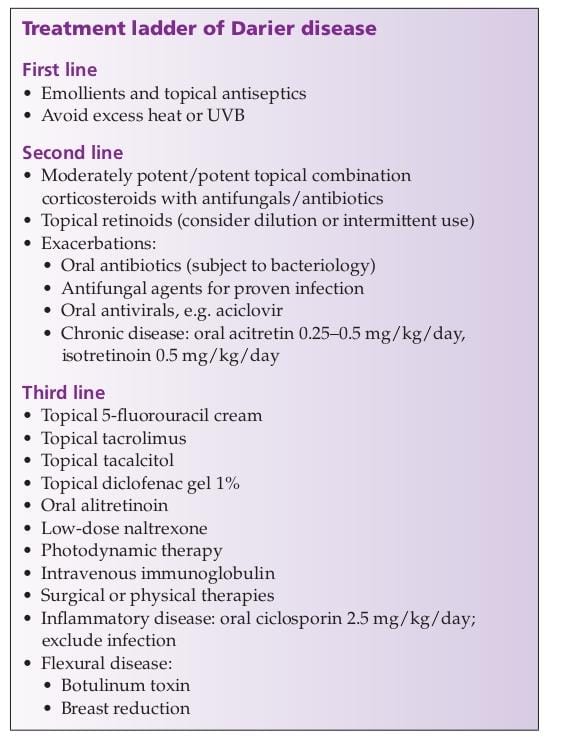
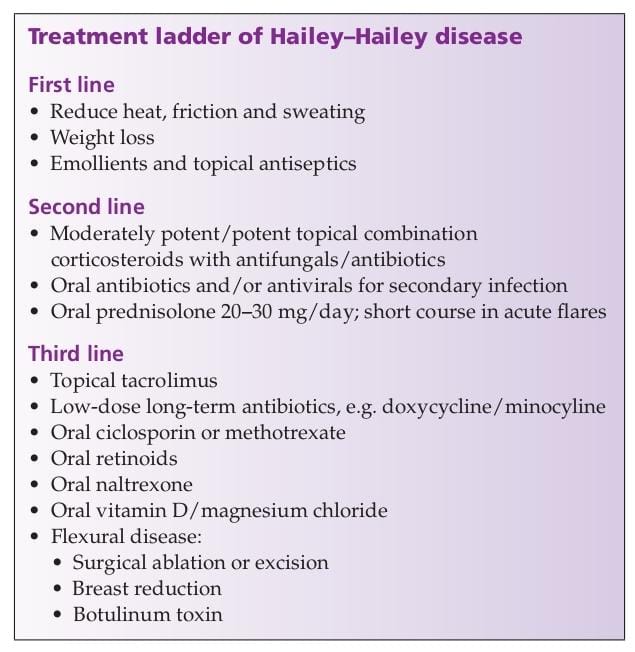
Listen to above voice notes and then revise from above table and treatment ladder from rooks only and simply practice mcqs for this chap
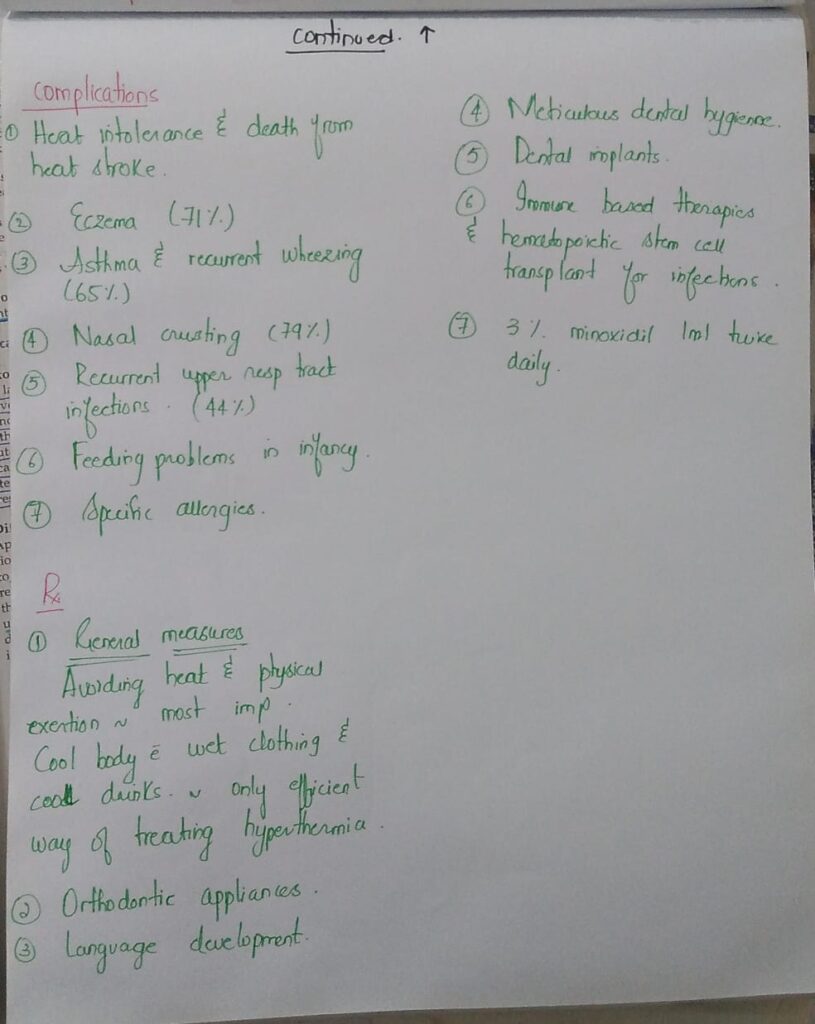
1️⃣ X linked hypohidrotic ectodermal dysplasia with immunodeficiency
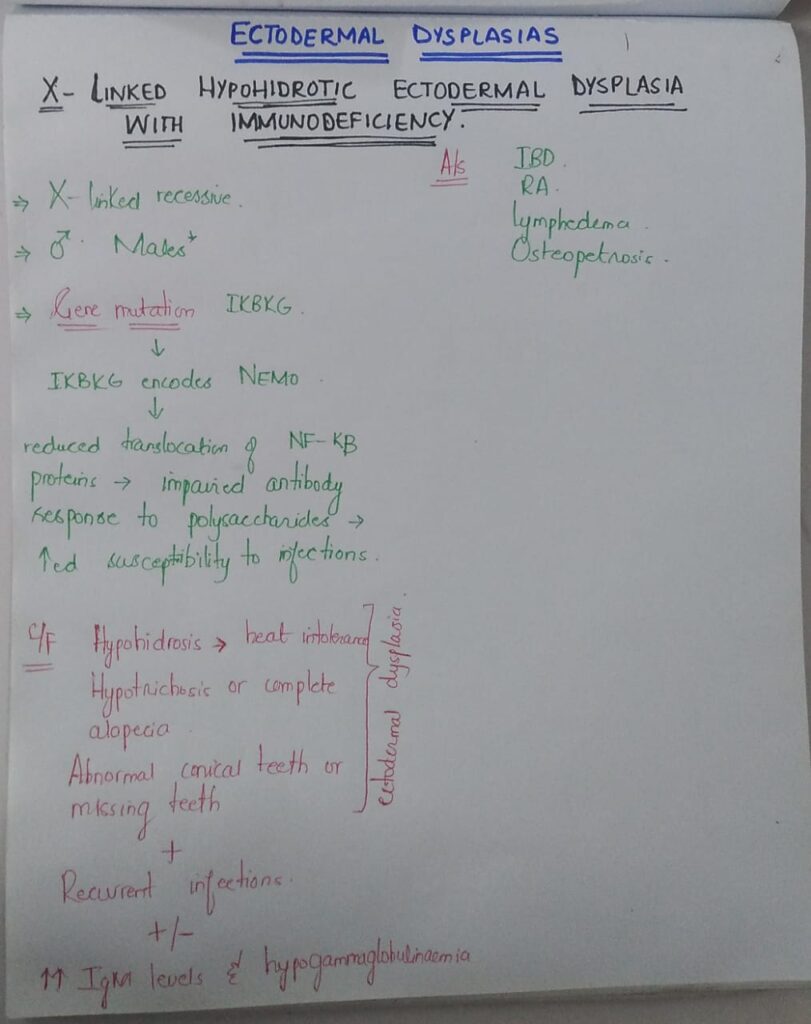
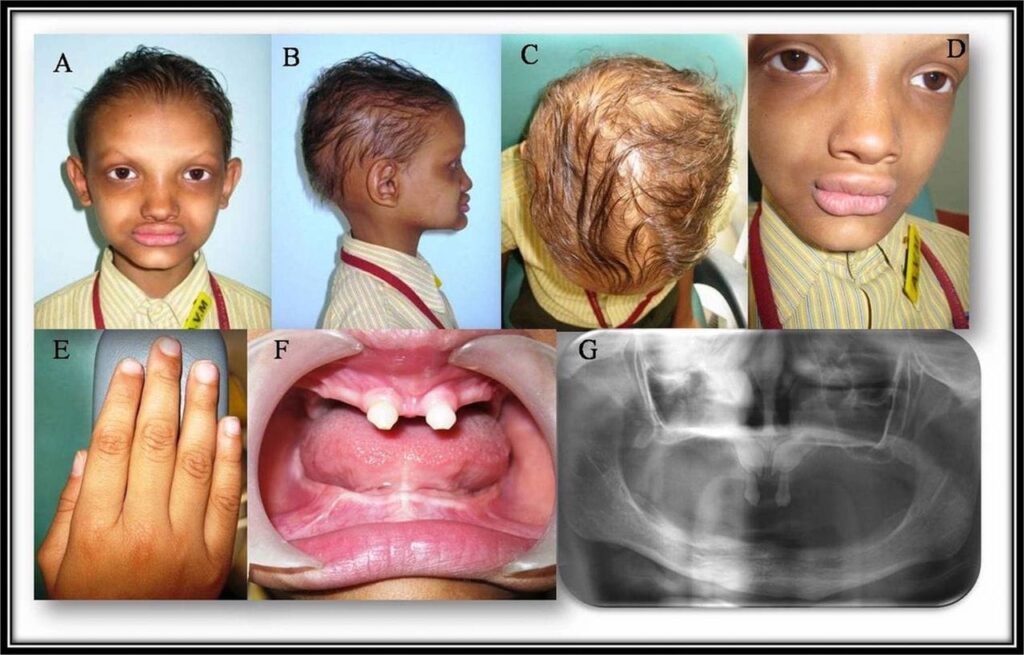
2️⃣ Hypohidrotic ectodermal dysplasia



🔰 for reference, pictures given in rooks are also gud
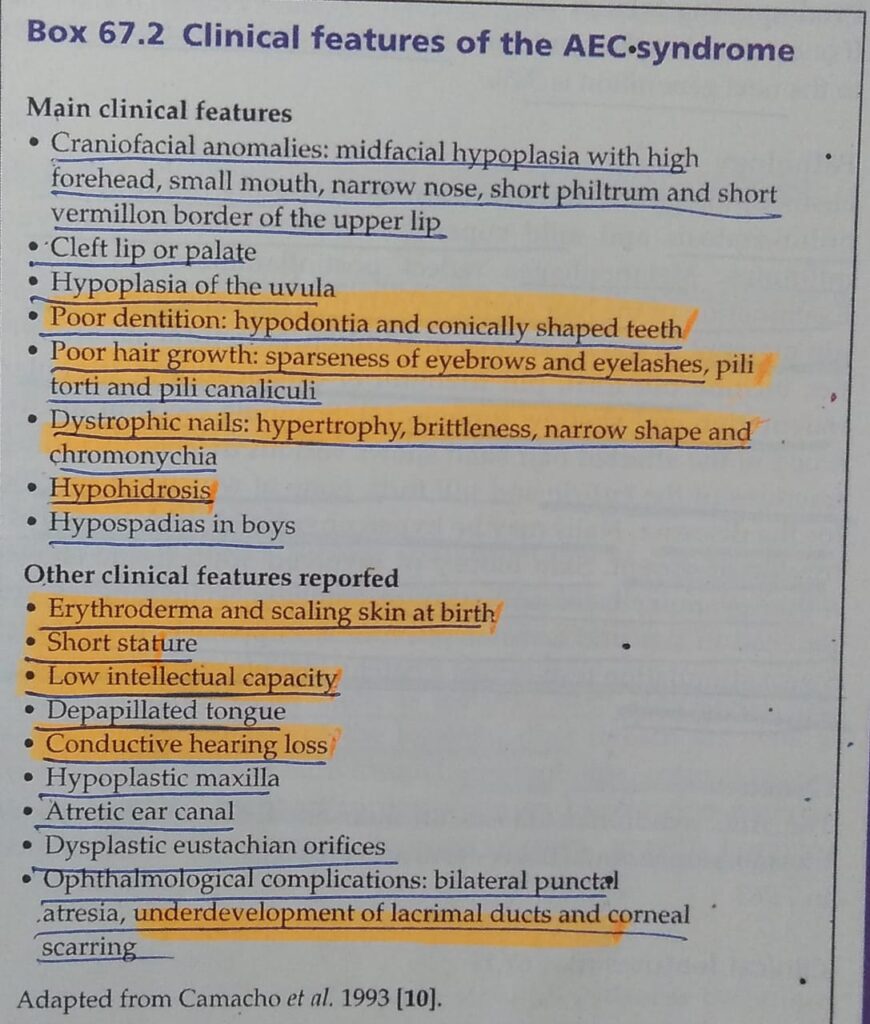
3️⃣ Ankyloblephron- ectodermal defect – cleft lip/palate syndrome



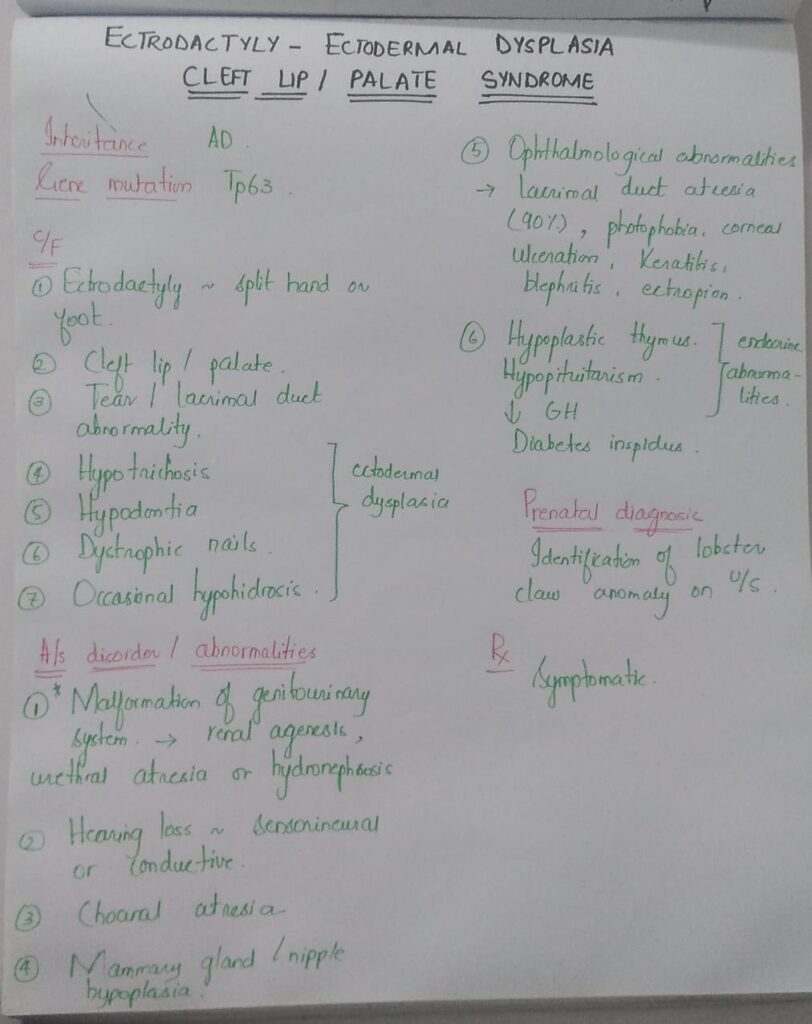
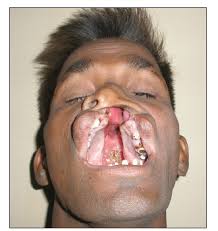
4️⃣ Ectrodactyly – ectodermal dysplasia cleft lip/palate syndrome



5️⃣ Tricho – dento – osseous syndrome

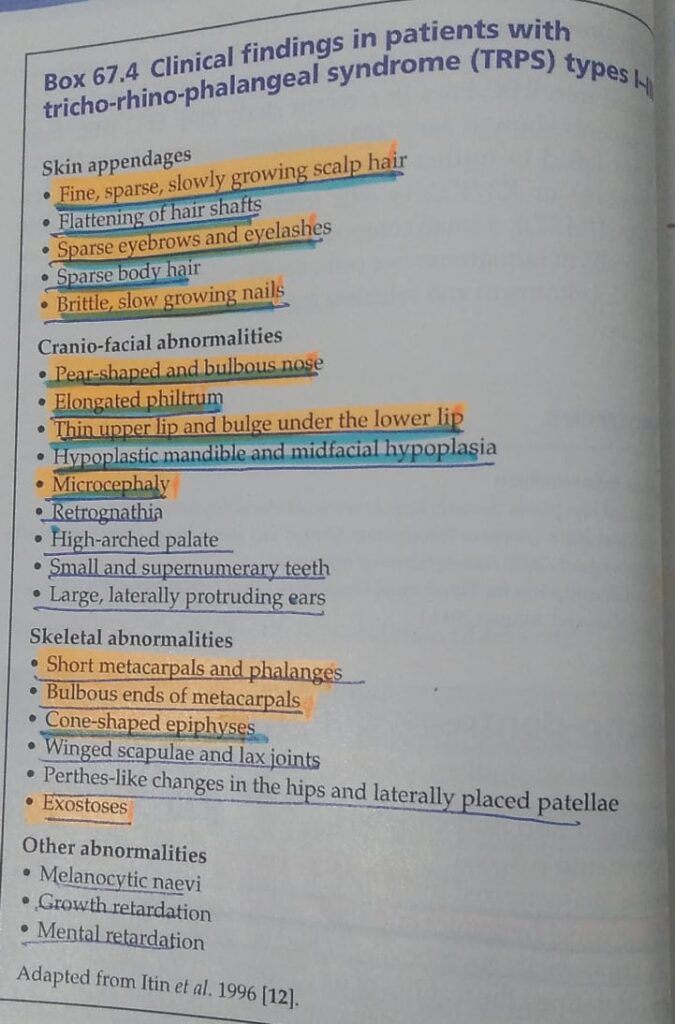
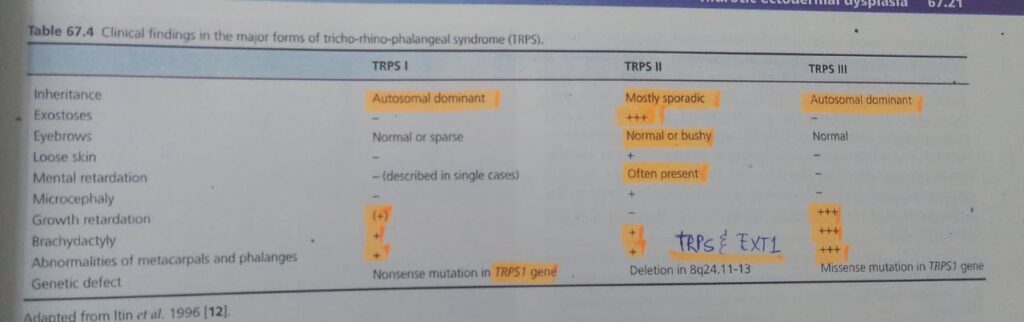
6️⃣ Tricho-rhino-phalangeal syndrome
Only remember highlighted 1s

7️⃣ Hidrotic ectodermal dysplasia / Clouston disease
8️⃣ Focal dermal hypoplasia


9️⃣ MIDAS syndrome
(Microphthalmia, dermal aplasia and sclero cornea)



🔰 Ectodermal dysplasia are an imp genodermatosis which are imp for theory exam.
Simply understand the features of ectodermal dysplasia and specific features of its various types. Revise from above short notes only and skip rooks.
Practicing mcqs will be sufficient in the last days of prep.
Happy learning😊
🔰 Note down these marked 1s and memorize only from the table.
1️⃣ Monilethrix

2️⃣ Woolly hair
3️⃣ Pili torti


4️⃣ Trichorrhexis nodosa

5️⃣ Trichorrhexis invaginata

6️⃣ Trichothiodystrophy

7️⃣ Pili triangulati et canaliculi


8️⃣ Loose anagen syndrome
🔰 Important note for this chap👇🏻
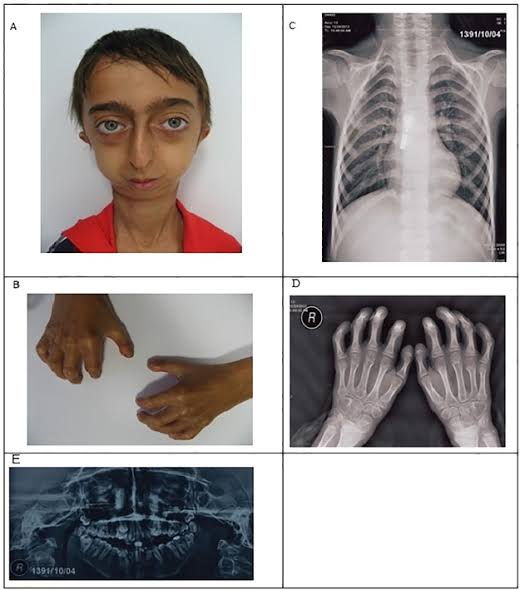
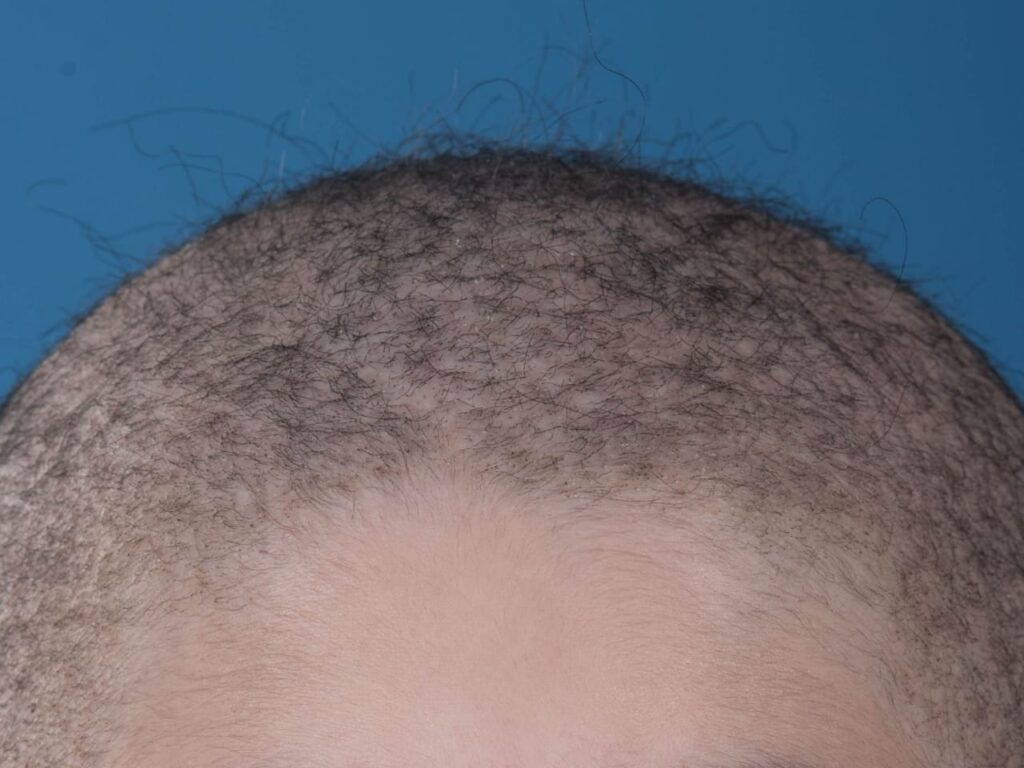
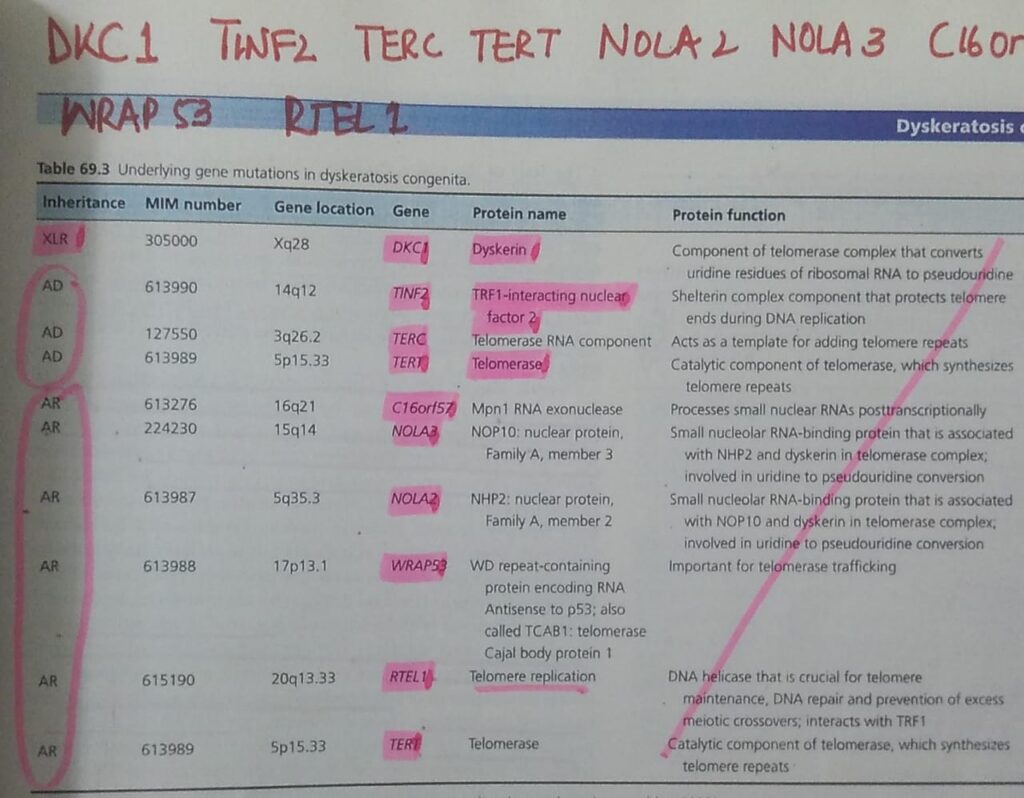
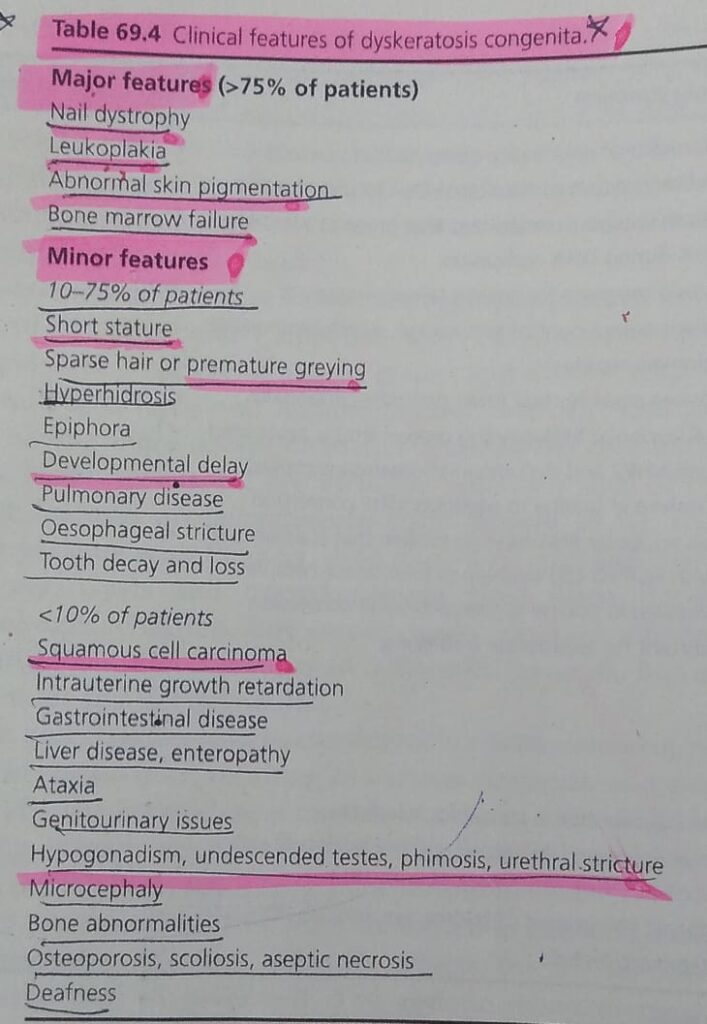
1️⃣ Dyskeratosis congenita
🔰 Go through above mentioned tables and voice notes only and practice with mcqs

2️⃣ Nail-Patella syndrome



🔰 Practice above topics from ETAS and u l not even feel the need to read these topics 👆🏻



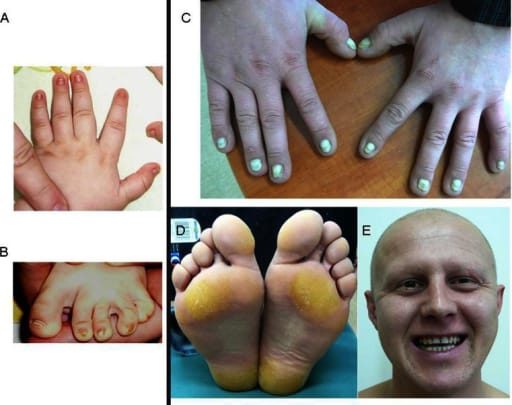
2️⃣ Linear and whorled naevoid hypermelanosis👇🏻

3️⃣ **Naegeli Franceschetti Jadassohn syndrome
Dermopathia pigmentosa reticularis**
🔰 Interesting mneumonic 😊👆🏻

4️⃣ Dowling Degos disease👇🏻


5️⃣ Reticulate acropigmentation of Kitamura

6️⃣ Peutz Jeghers Touraine syndrome


Dyschromatosis symmetrica hereditria

Dyschromatosis universalis hereditaria


🔰 *Important tip for this chap*
Tables shared in the start of this chap are enough for a quick revision. Practice mcqs for exams and revise from tables
Happy learning😊






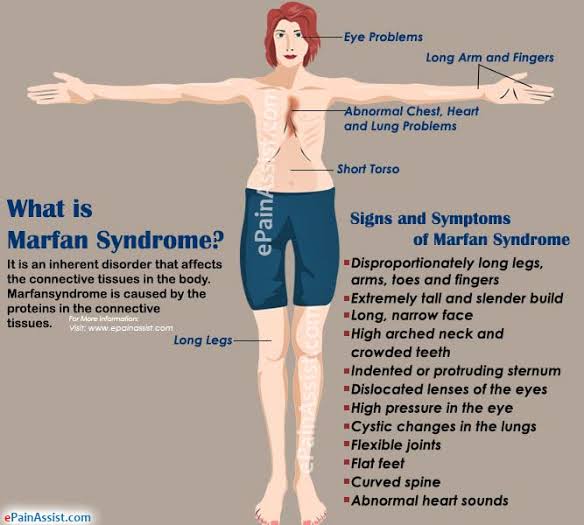
2️⃣ Prolidase deficiency👇🏻


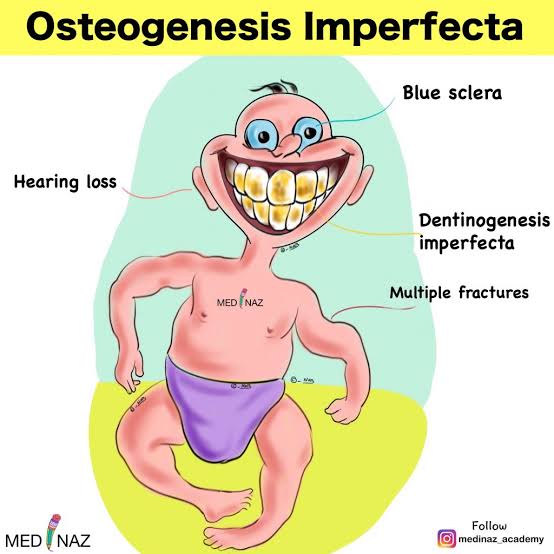
3️⃣ Osteogenesis imperfecta 👇🏻




2️⃣ Williams Beuren syndrome 👇🏻





















🟩AD
🟩TSC1 TSC2
🔰Hamartomas in any tissue
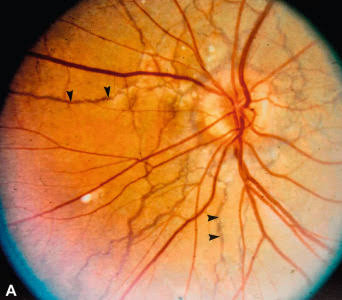
🔰Eyes: Retinal phacomas (white streaks along the vessels or as small, rounded tumours near the disc)
scotomas
Hypopigmented spots in the iris
*CNS* :
Subependymal nodules,
Obstructive hydrocephalus,
Mental retardation.
*Cardiac* :
Cardiac rhabdomyomas,
Cardiac arrhythmia
*Renal* :
angiomyolipoma,
Renal cysts,
Renal cell carcinoma.
*Pulmonary* :
Recurrent spontaneous pneumothorax,
Lymphangioleiomyomatosis gives rise to chylothorax.
*GIT* :
hamartomatous colonic polyps
*Endocrine and other metabolic disturbances* :
pituitary–adrenal dysfunction,
thyroid disorders
and premature puberty.
🔰Investigations:
Woods lamp examination for ash leaf macule
Eye: Slit lamp examination and fundoscopy
ECG: conduction defects
Echo:Cardiac rhabdomyomas
_CT brain:_ calcified periventricular nodules that project into the lateral ventricles and hypoattenuated parenchymal lesions.
**_MRI Brain.*_*
more sensitive in the detection of parenchymal lesions
U/s abdomen: for renal hemartomas.
Chest X RAY: irregular reticulation of the lung field
X ray skull:
Calcification on plain xray
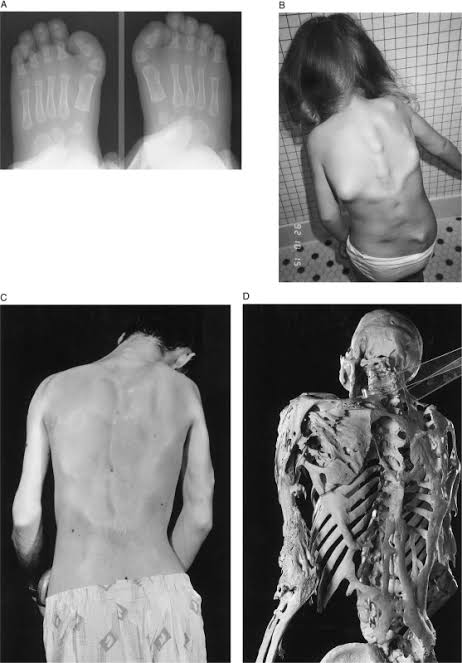
X RAY Hands and feet :
Cyst‐like lesions of the phalanges and irregular thickening of the cortex of the metatarsals and metacarpal.
Colonoscopy:
hamartomatous colonic polyps.
Family screening and DNA testing.
🔰Management:
Angiofibromas: pulsed dye vascular laser (wavelength 595 nm)
Co2 laser
Topical rapamycin at 1% or 2% concentration for cutaneous angiofibromas
Systemic rapamycin may be useful in the therapy of visceral tumours and neurological complication
Neurosurgery : for obstructive hydrocephalus
Or microsurgical removal of brain neoplasm.
🔰Prognosis
3% die in 1st yr
28% < 10 yr
75% die before 25 yrs
🔰Most common cause of death??
Epilepsy and infections
🔰 For revision, only read these keys and table from rooks in which diagnostic criteria is given.






Mnemonic: COOL FAN
Calms 6 or more > 5 prepubertal > 15 postpubertal
Optic glioma
Osseous lesion i.e. sphenoid dysplasia or thinning of long bones
Leish nodules 2 or more
Family history (1st degree)
Axillary/ inguinal freckiling
Neurofibroma 2 or more or one plexiform neurofibroma
🟩what malignancies can b associated with NF1?Intracranial tumors:
Optic glioma
Astrocytoma
Shwanoma
Sarcomatous change in NF:
Malignant peripheral nerve sheath tumor (MPNSTs)
Others:
Wilms, rhbdomyosarcoma, leukemia, retinoblastoma, malgnant melanoma
🟩Bad prognostic factors
- Git, cns, urinary involvement
- Prepubertal increase in calms
- Development of malignany, HTN and endocrine abnormalities especially pheochromocytoma
🟩Selumitinib new drug to treat neurofibromas
It’s a mitogen activated protein kinase inhibitor,FDA approved
🔰Important note.
Such kind of keys are a great help.
Save these and thank me later.
Make a watsapp grp and keep on saving these keys with pictures.
1 month before exam close ua books and juz revise these keys. It ll not only save ua precious time but also keep u away from anxiety and tension near the exam





Follow up for malignancies👇🏻
>30 yrs Breast
>35 yrs Colon
>40 yrs. Kidney


















Management
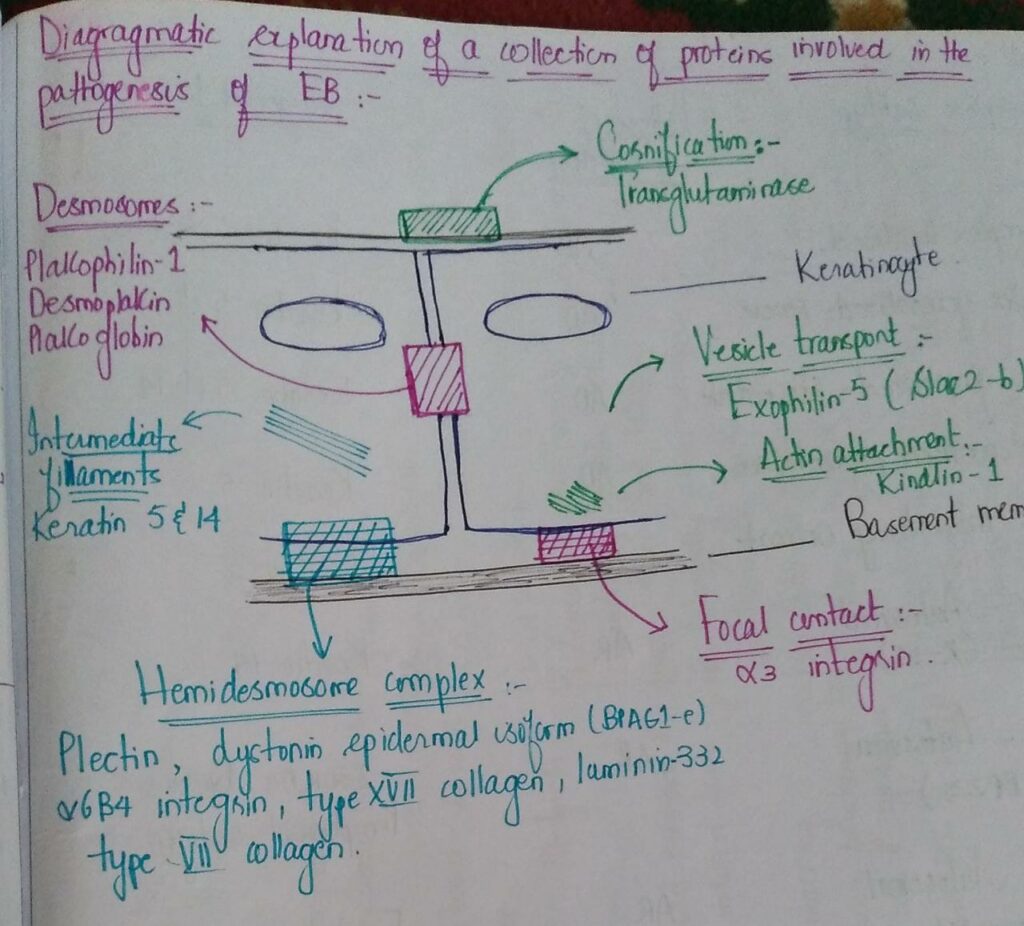
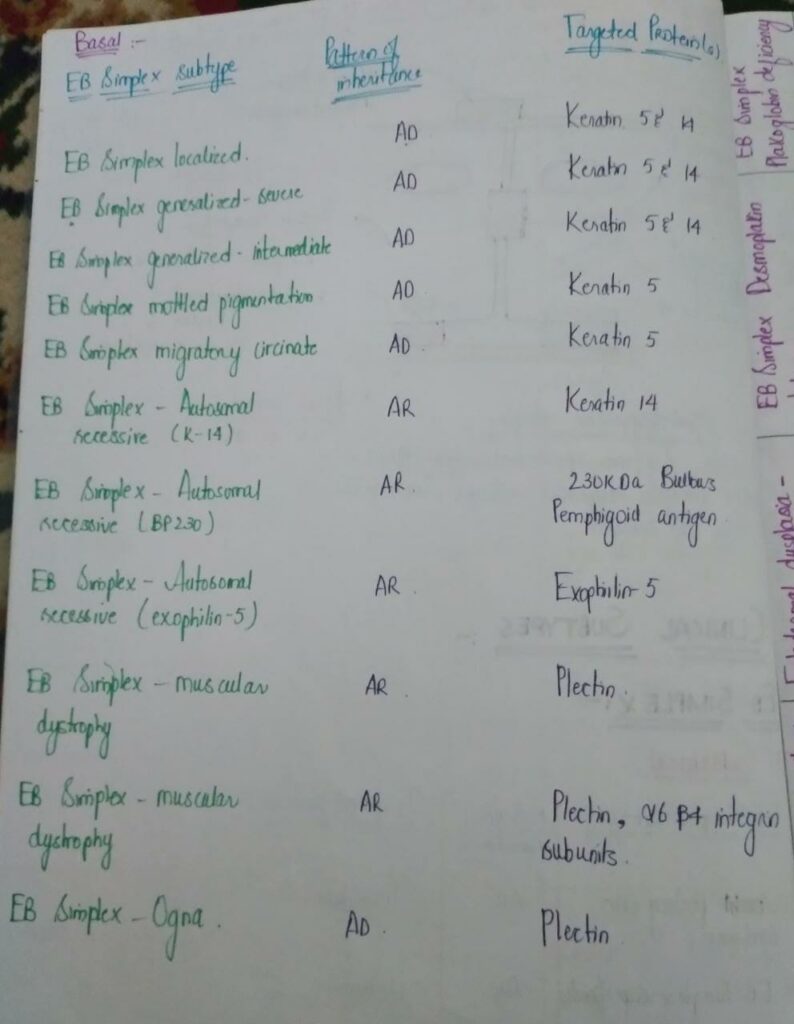
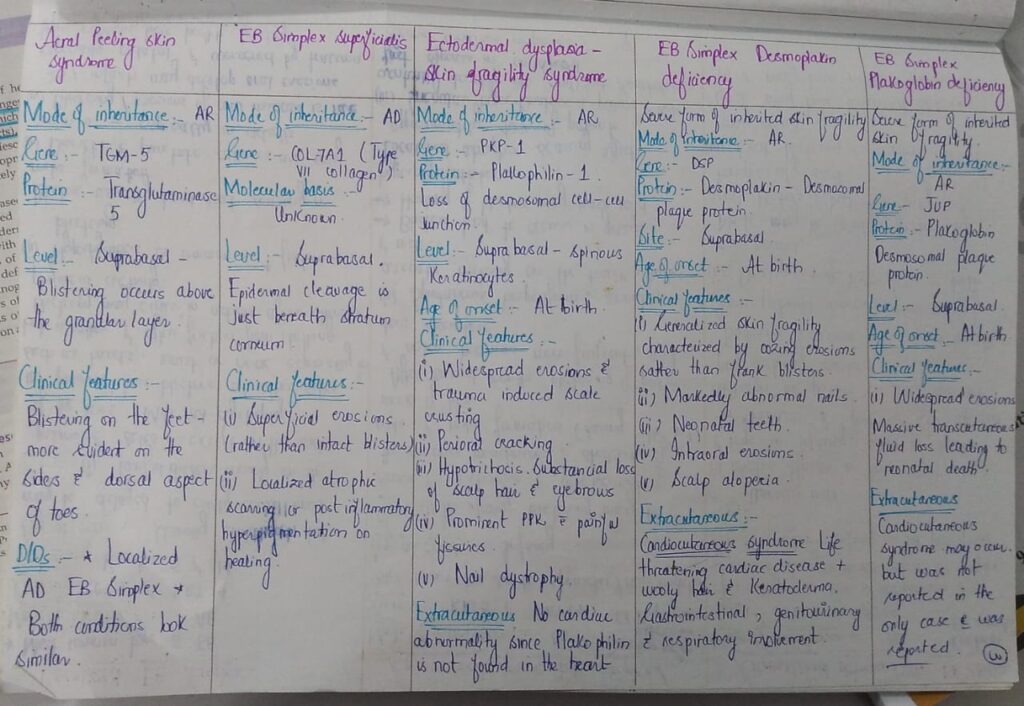
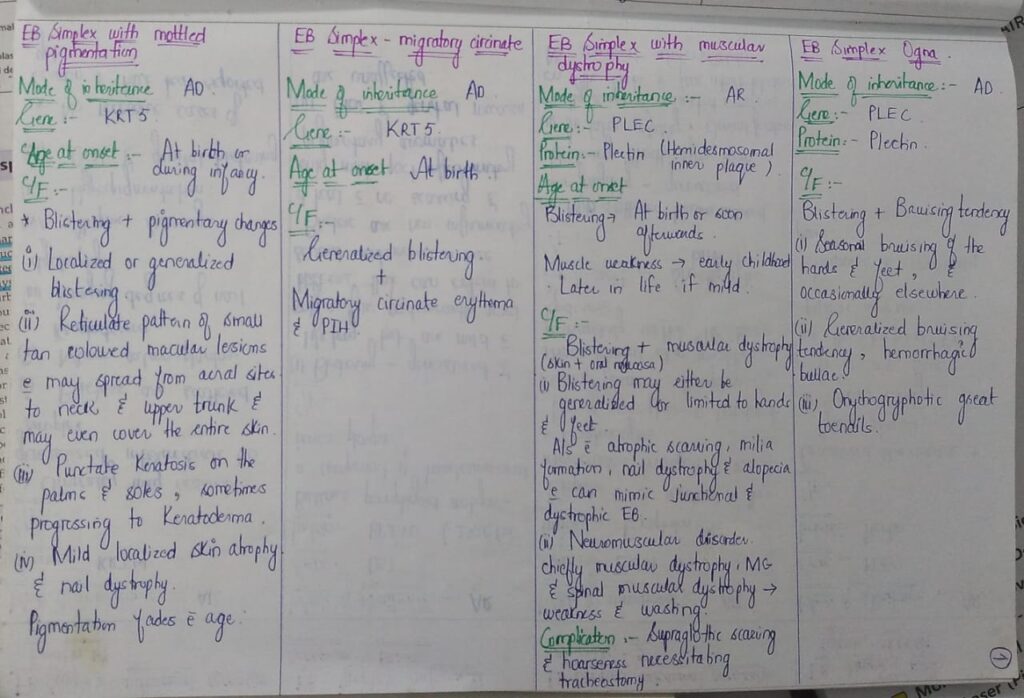
🌟🌟🌟EB counselling🌟🌟🌟🌟

 *Important note* EB is a really imp chap from both theory and viva exam point of view. U must revise it again n again to become fluent in answering the questions. Listen to above voice notes and then revise from tables which i have shared and then practice by solving mcqs. ETAS has a very useful mcq pool esp genetics, which makes concept clear.
*Important note* EB is a really imp chap from both theory and viva exam point of view. U must revise it again n again to become fluent in answering the questions. Listen to above voice notes and then revise from tables which i have shared and then practice by solving mcqs. ETAS has a very useful mcq pool esp genetics, which makes concept clear.


























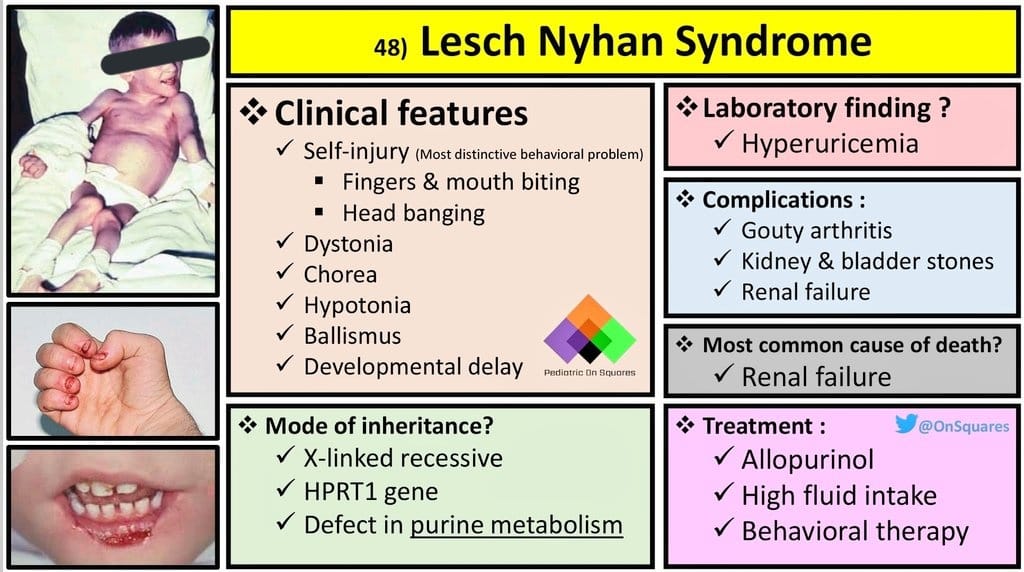
🔰 *Excellent mneumonic of Lesch nyhan by Dr Mehran 👇🏻*
Leisch Nahyan ek pagal insaan hai, jo dance karta (chorea) , gata haklata (dysarthria), cd70 motorocycle (60-70 iq) per charh k sheher mein ghoomta hai, khud ko aur sab ko kat’ta phirta hai (self harm and aggresiveness) Urine bhi kardeta hai unpe (inc Uric acid), hairat angez (HRPT1 gene) aur khoonkhaar (in erythrocytes) admi hai
Alloo pulao (Allupurinol) khilao usko, to he stop urinating (nephropathy improves) but a pagal remains a pagal (no neurological improvement)
Dant nikalay to tor dijiye (teeth extraction helps self harm)




🔰 Following topics are covered much better and in detail in other chaps so dun waste ua time reading it from this chap👇🏻
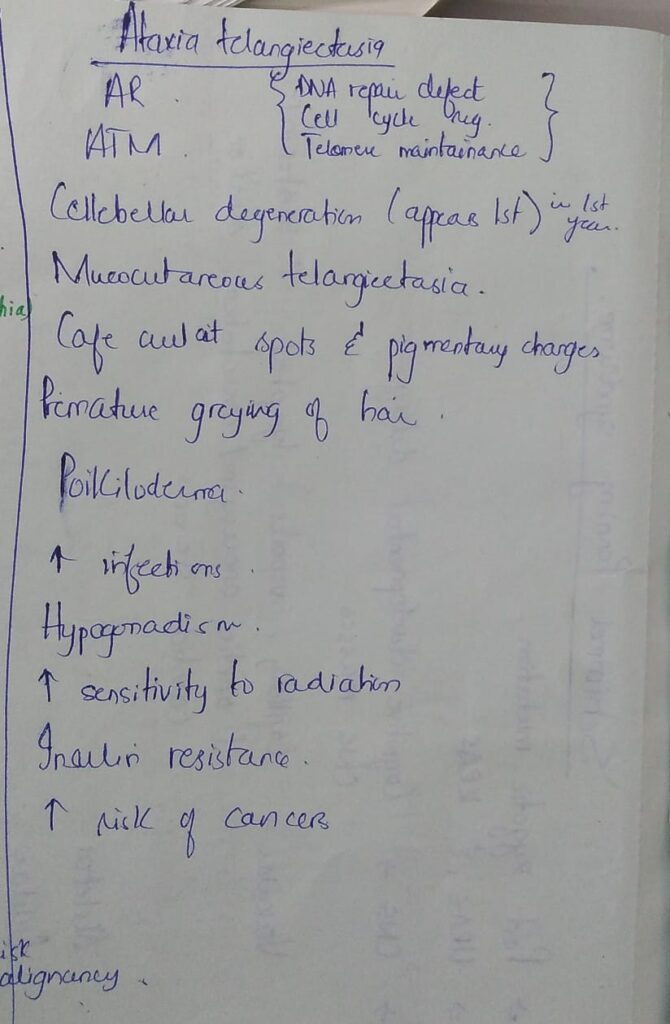
- DNA repair defects
- Comel Netherton syndrome
- DKC
- Fanconi anemia
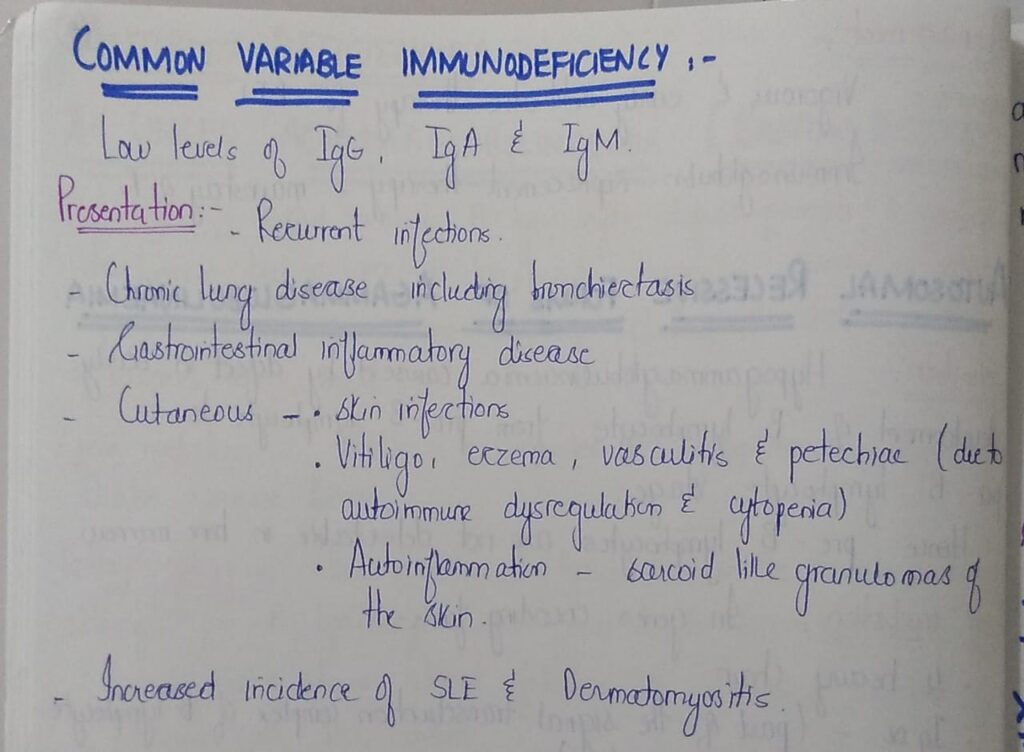
🔰 Antibody deficiencies
1️⃣ X linked agammaglobulinaemia / Bruton disease 👇🏻
🔰 DISEASES WITH IMMUNE DYSREGULATION
1️⃣ *Primary immunodeficiency with hypopigmentation*
- Chediak Higashi syndrome
- Griscelli syndrome type II
- Hermansky Pudlak syndrome
Already discussed in disorders of pigmentation. So no need to repeat from here.
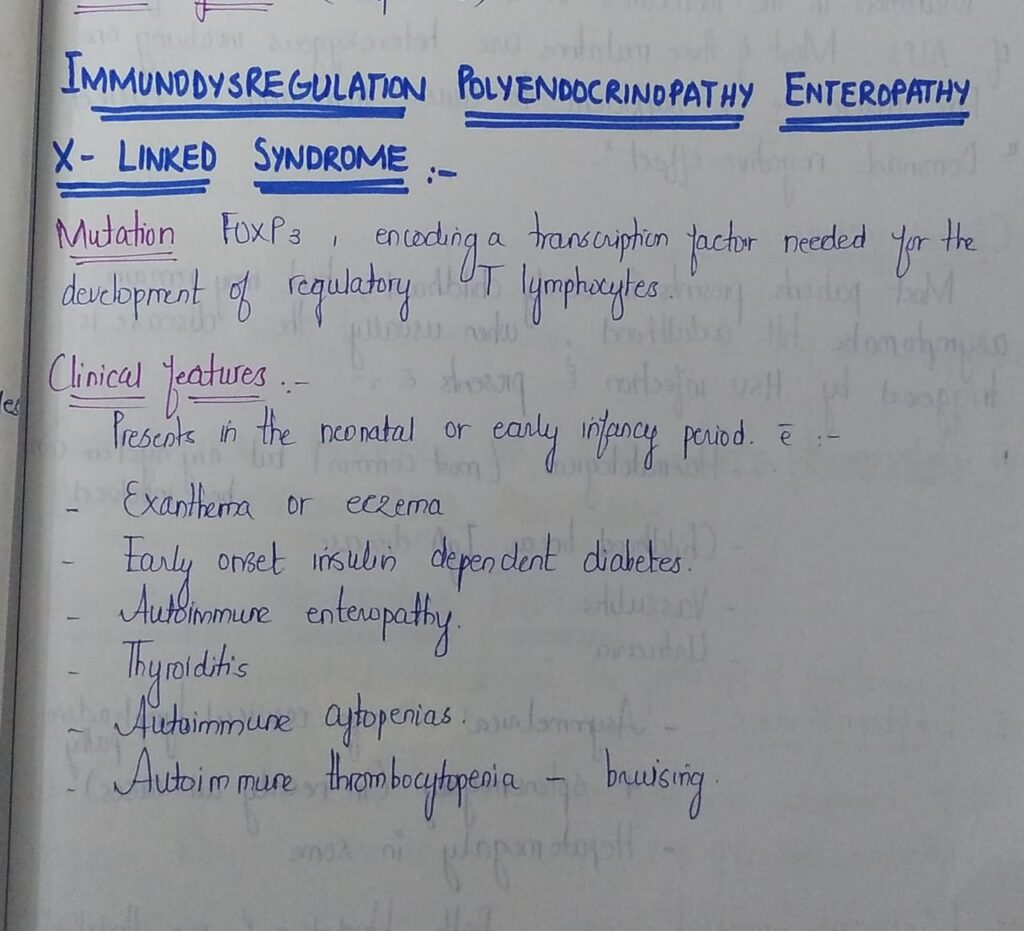
2️⃣ *Immunodysregulation Polyendocrinopathy enteropathy X- linked syndrome*
3️⃣ Autoimmune lymphoproliferative syndrome
🔰 CONGENITAL DEFECTS OF PHAGOCYTE FUNCTION
1️⃣ Functional neutrophil defects
2️⃣ Defects of Neutrophil differentiation

3️⃣ Defects of Neutrophil adhesion
3️⃣ Defects of Neutrophil adhesion
1️⃣ NF-KB pathway related primary immunodeficiency
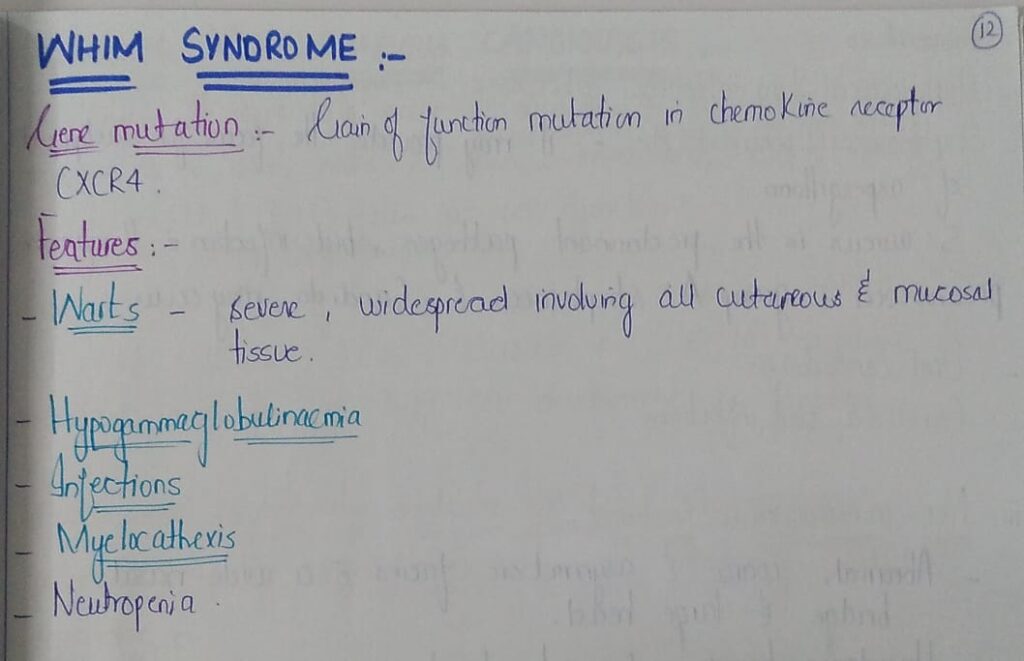
2️⃣ WHIM syndrome


3️⃣ Hyper IgE syndrome



4️⃣ Chronic mucocutaneous candidiasis


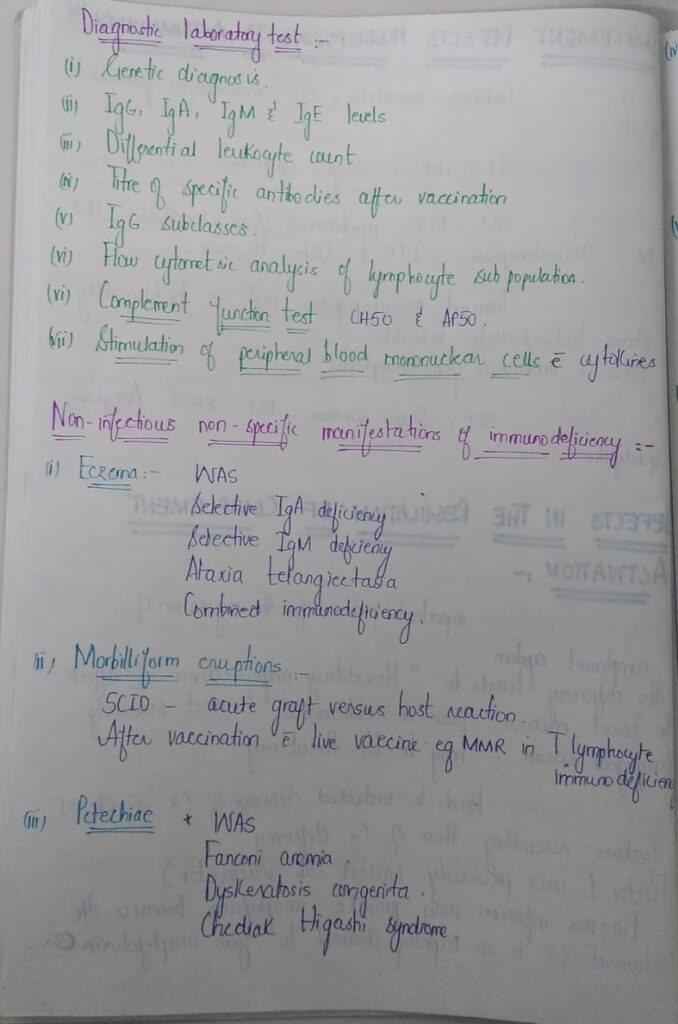
🔰 Complement disease
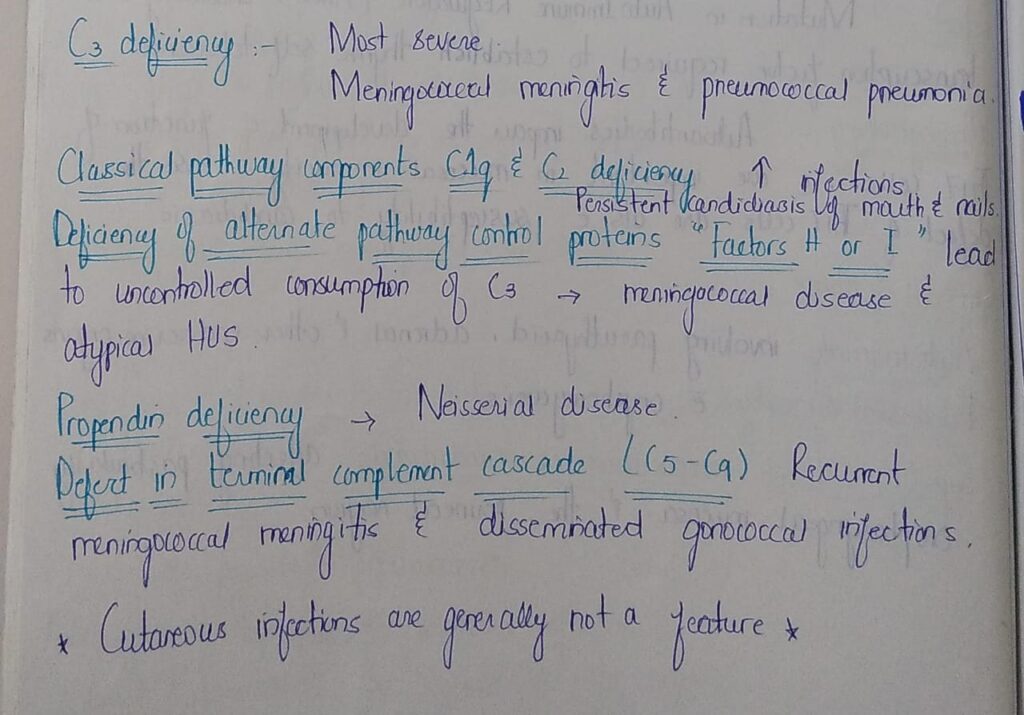
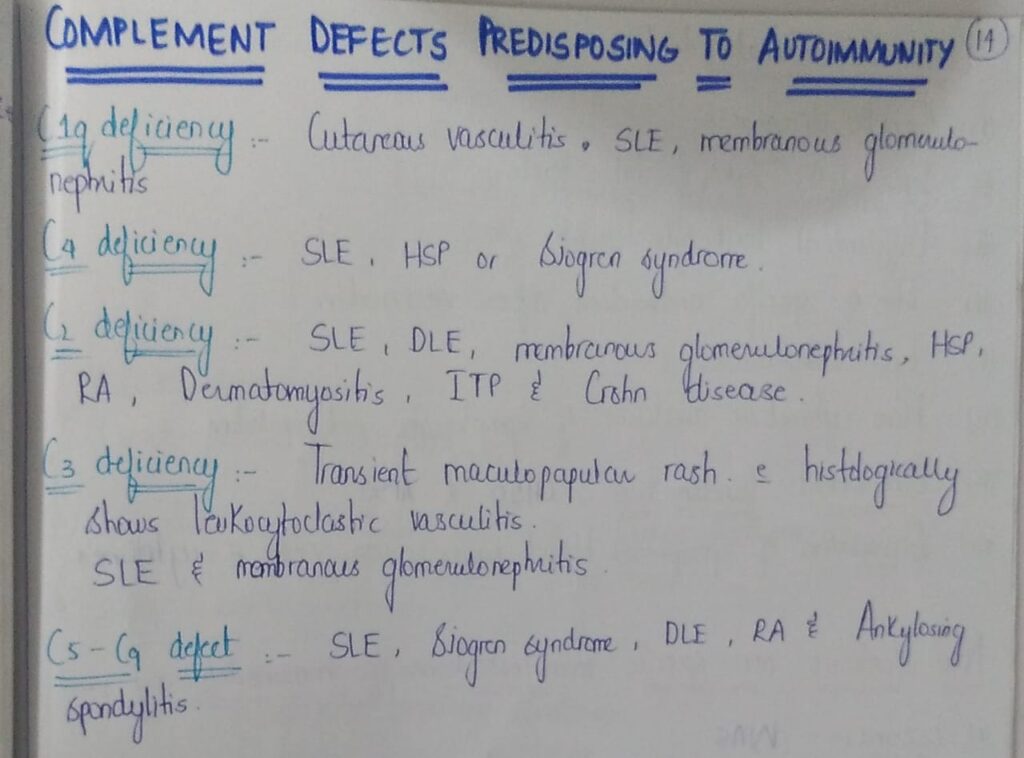
🔰 Complement disease
Important additions 👇🏻

🔰 *IMPORTANT NOTE*
For this chap, only listen to above voice notes and practice mcqs.
Reading from rooks only creates confusion.
Topics and material given above is all u need for the theory exam.
Rest of the reading should be for self pleasure only😂