- Arthropods
Arthropods:
Myiasis

Fleas:

Tungiasis:


Lice/ Pediculosis/ Phthiraptera:
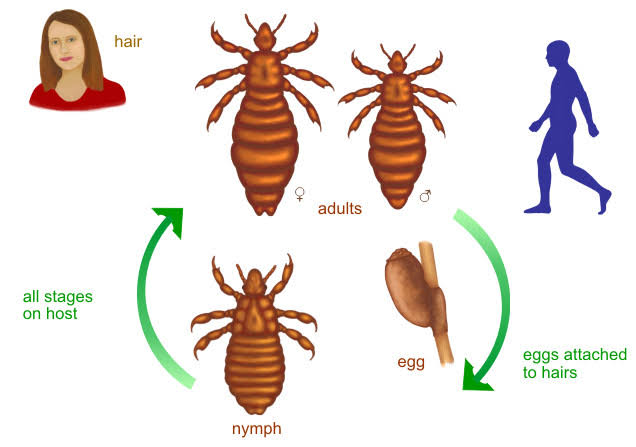

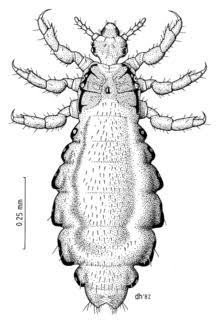
Clothing/body louse


Crab lice/Phthririasis pubis


Bed bugs:

Sarcoptidae: Human Classical Scabies:


Crusted/ Norwegian scabies

House-dust mite:
Follicle mites/ Demodicidae

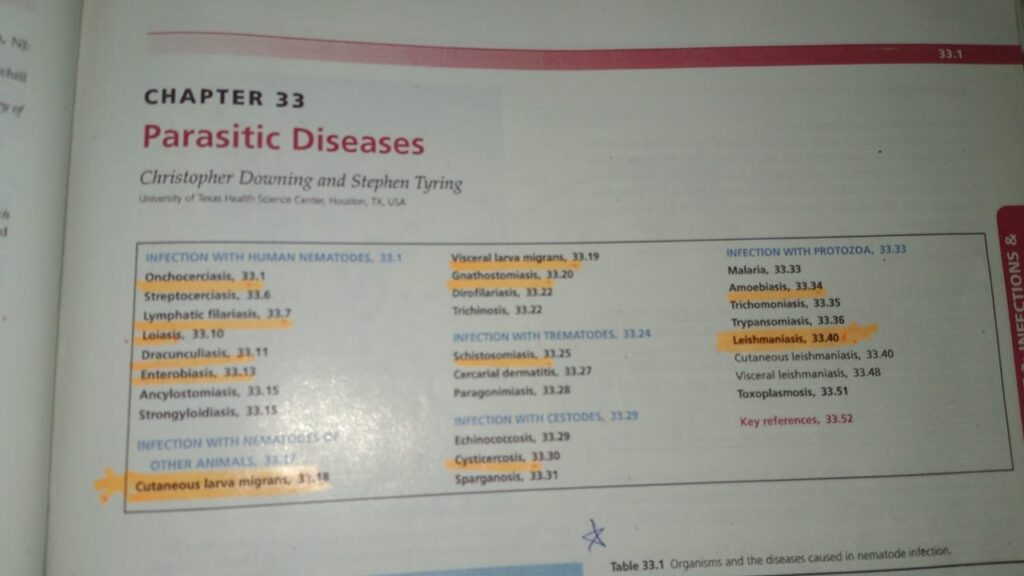
American trypanosomiasis Larva Curens Anklyostomiasis, Strongyloidiasis Trypanosomiasis,
These are very imp too and comes frequently in theory exam

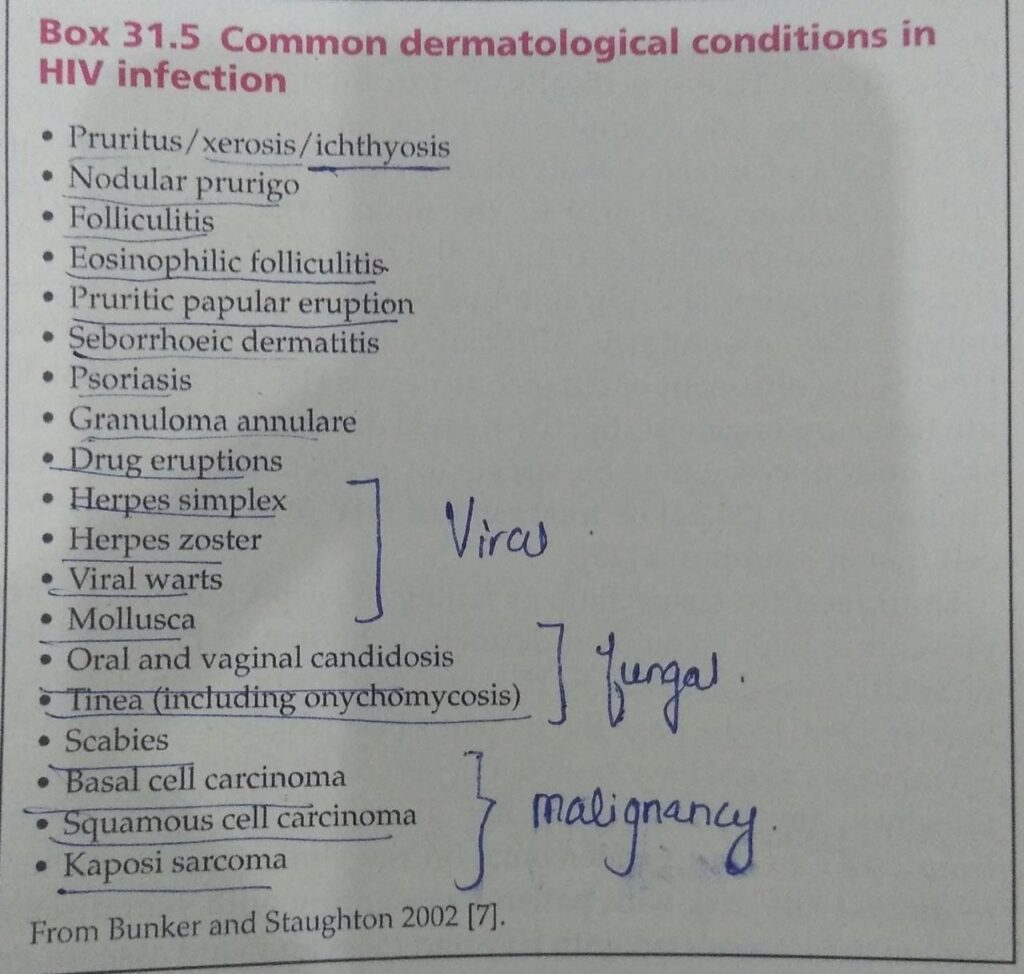
HIV AND THE SKIN:
Pigmentary disorders
Coagulopathies
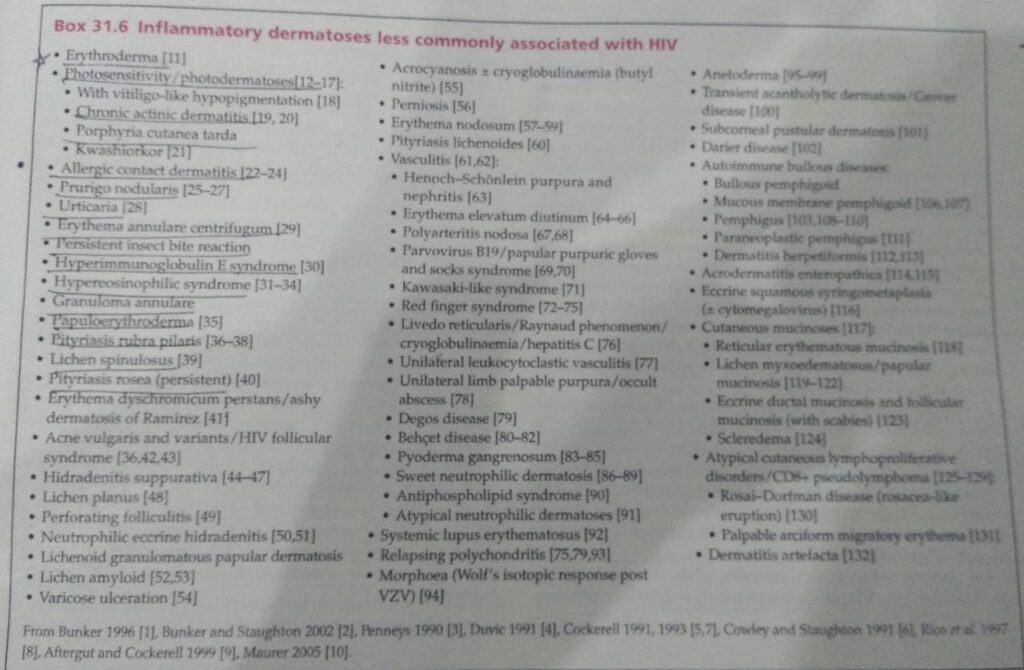
Inflammatory dermatosis
Seborrhoeic dermatitis
Erythroderma
Atopic eczema
Psoriasis
Eosinophilic folliculitis
Pruritic papular eruption
Granuloma annulare
Porphyria cutanea tarda
Bacterial infections
Viral infections
Fungal infections
Protozoal infections
Scabies
Miscellaneous
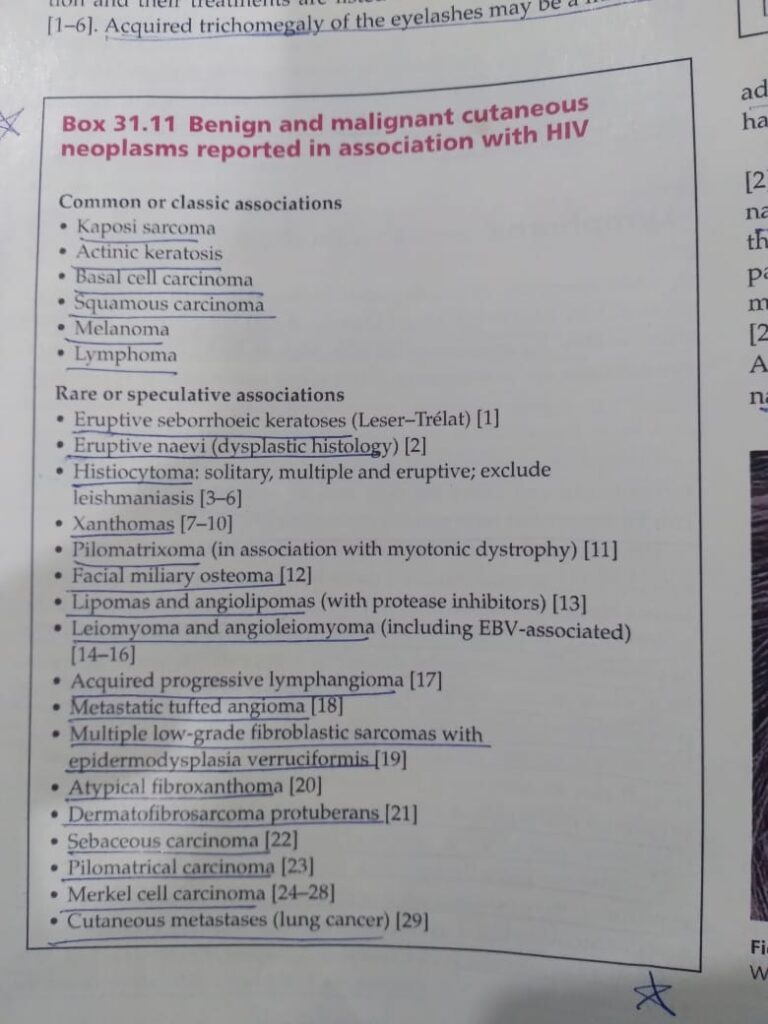
Neoplasms
KAPOSI SARCOMA
MELANOMA AND NON MELANOMA SKIN CANCERS
LYMPHOMA
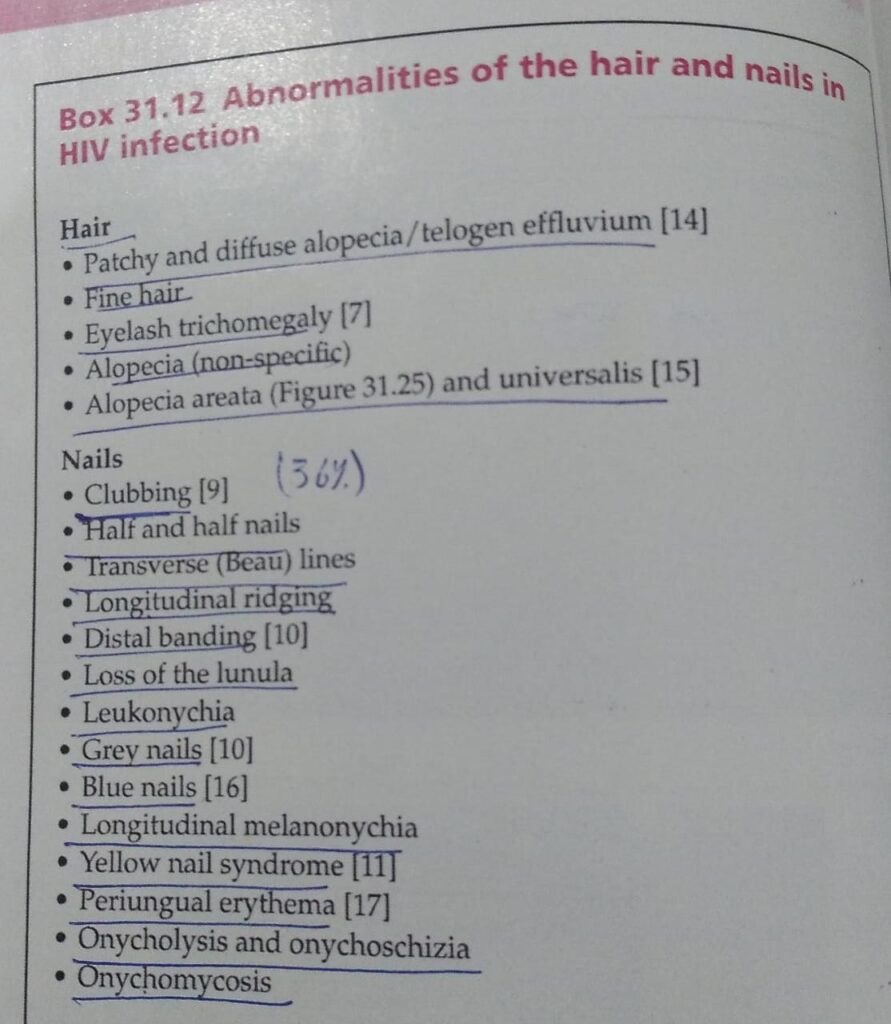
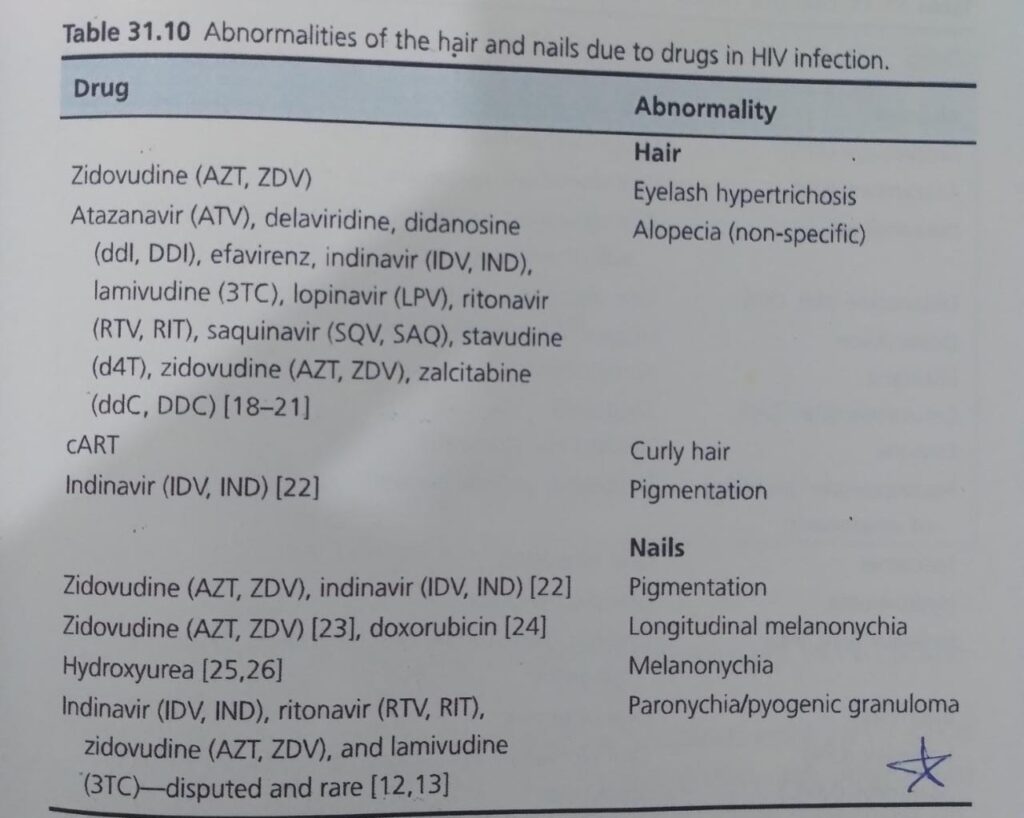
HAIR AND NAILS
ORO-PHARYNX
HIV IN CHILDREN
IRIS/IRD/IRAD
Indicator conditions in case definition of AIDS
Investigations
Dds of primary HIV infection
#pearls topic is HIV.
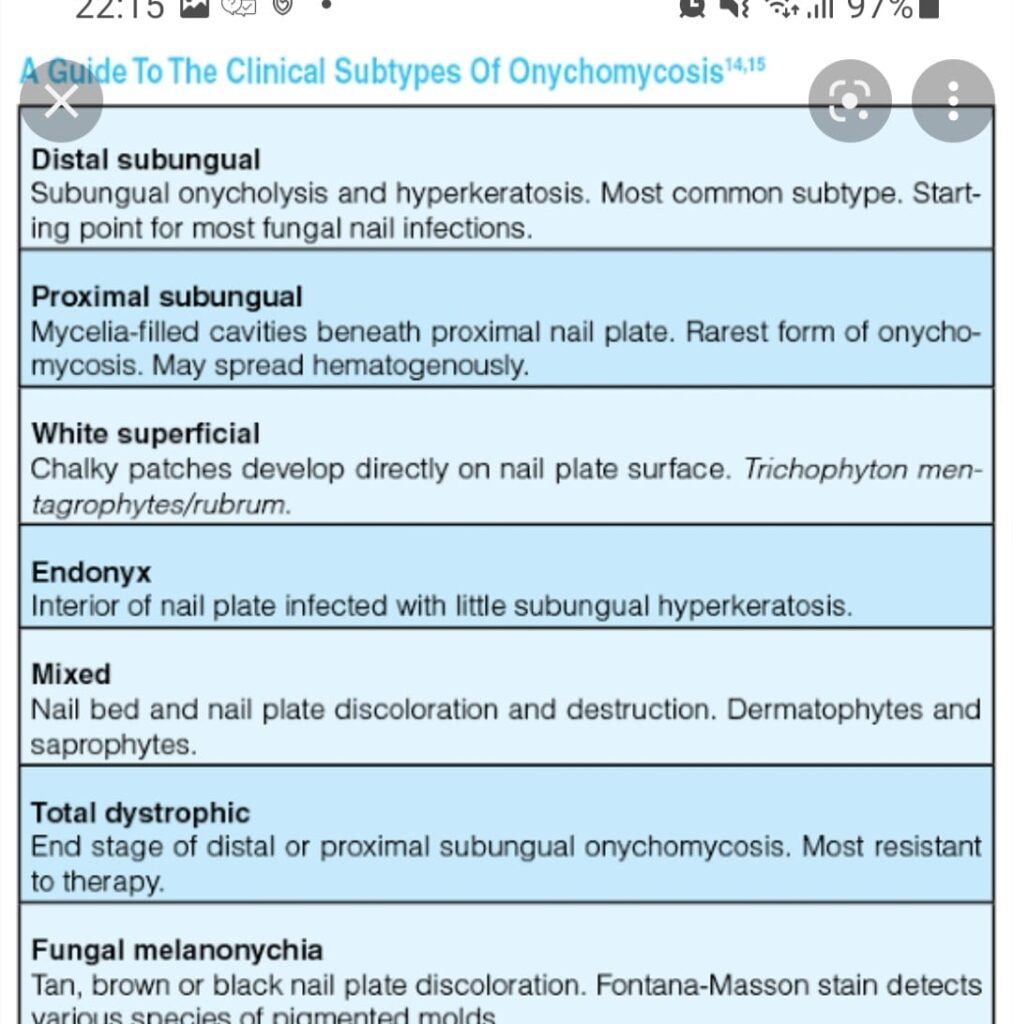
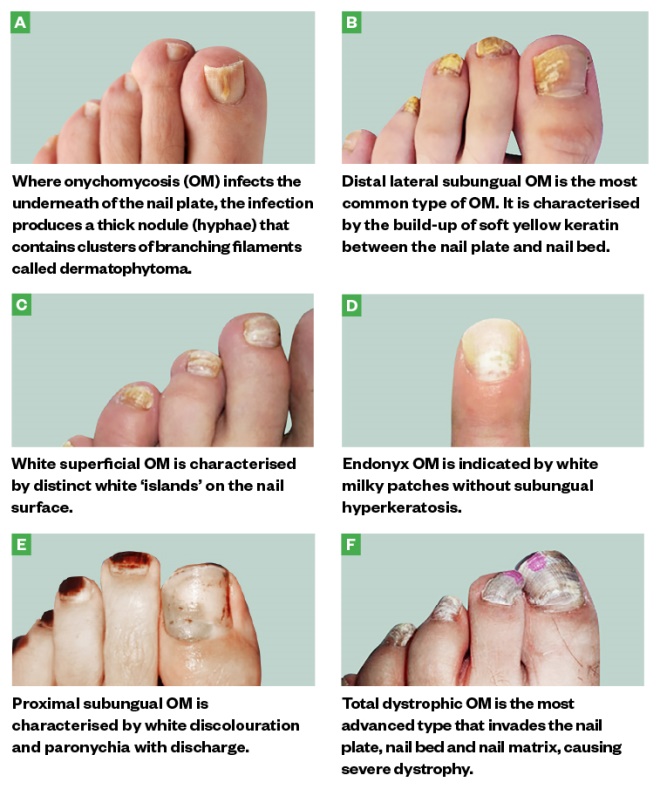
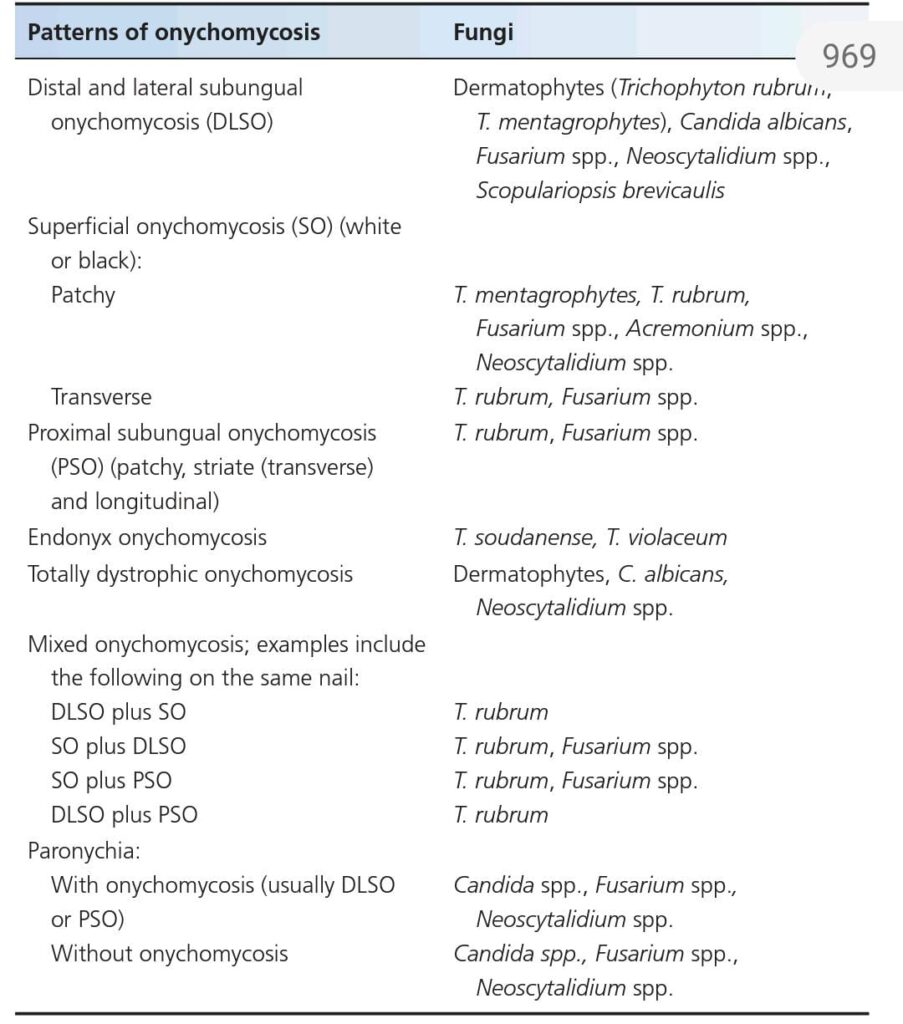
1-Most common pathogen to cause onychomycosis…..T.ruburm
Treatment of fungal infection… Same as in Non HIV. Oral terbinafine is safe.
2-Stain used for cutaneous histoplasmosis is Gomori methenamine silver stain
Stain used for systemic histoplasmosis is wright stain.
3-Cryptococcal infection …stain used is mucicaramine or tznack smear
Poor progsis if CNS involvement .
4-Leishmaniasis is difficult to treat compared to the one in normal person.it is associated with rheumatoid nodulosis.
5-Crusted scabies may b localized to sole or genitalia. On histo , eccrine ductal and follicular mucinosis can be seen.
6-kaposi sarcoma,a spindle cell tumor,risk increase if topical tacrolimus used in HIV.In children or non HIV person transmission is by saliva.
7-ratio of SCC:BCC 1:7
8- long term voriconazole therapy ,associated with multiple BCC.
9-melanoma ,a non AIDS defining cancer, has poor prognosis if CD4 count is low
10-most common BCC is superficial spreading type,treated with topical imiquimod
11- hodgkin disease with mixed cellularity and lymphocyte depleted ,more common in HIV.
12-most common lymphoma is NHL.
13 T.ruburm ,most common cause of onychomycosis
14- grey nail seen at CD4 count< 200 ×10⁶/L.
15-Oral hyperpigmentation is sign of low CD4 count (<200) .
16-If pt has hairy cell leukemia, 75% chance to develop AIDS with in 2 to 3 years.
17-concrum oris(noma), seen in malnourished HIV infected children.
18- hydroxyurea , cause melanonychia.
19- indinavir and zidovudine cause hair and nail pigmentation
20- foscarnet … side effect :Penile ulceration and eosinophilic folliculitis
PITYRIASIS RUBRA PILARIS:

LICHEN PLANUS AND LICHENOID DISORDERS:

Clinical features



Annular atrophic LP 👇

CLINICAL VARIANTS👇🏻
1️⃣ LP principally involving mucous membranes



Oral LP
Oral LP with reticulate pattern and Wickham’s striae
Erosive LP



Vulval LP
Vulvo vaginal gingival syndrome
Penile LP
2️⃣ Lichen plano pilaris


Lichen planopilaris
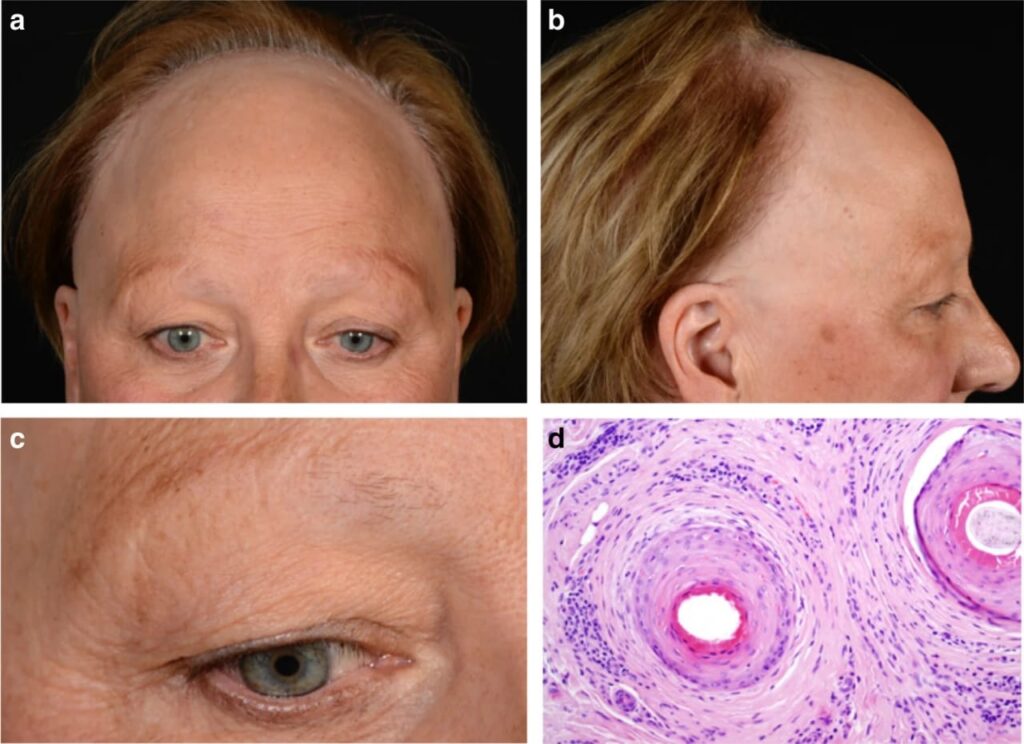
Frontal fibrosing alopecia
Graham Little Picardi syndrome

3️⃣ Hypertrophic LP


4️⃣ LP of palms and soles

5️⃣ Actinic LP
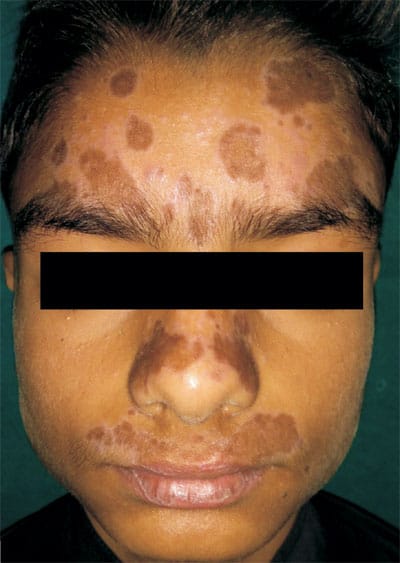

6️⃣ Lichen planus pigmentosus


7️⃣ Annular lichen planus

8️⃣ Guttate LP

9️⃣ DLE/LP overlap
🔟 Bullous LP and LP pemphigoides


Bullous LP
LP pemphigoides
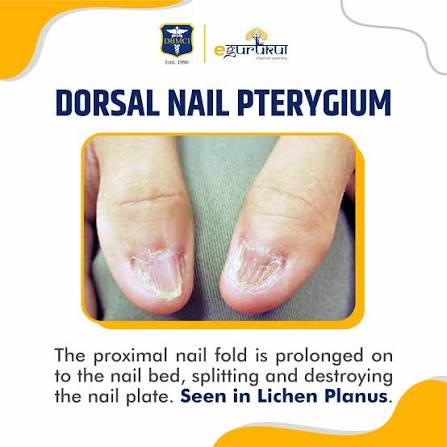
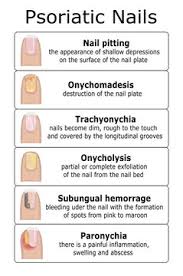
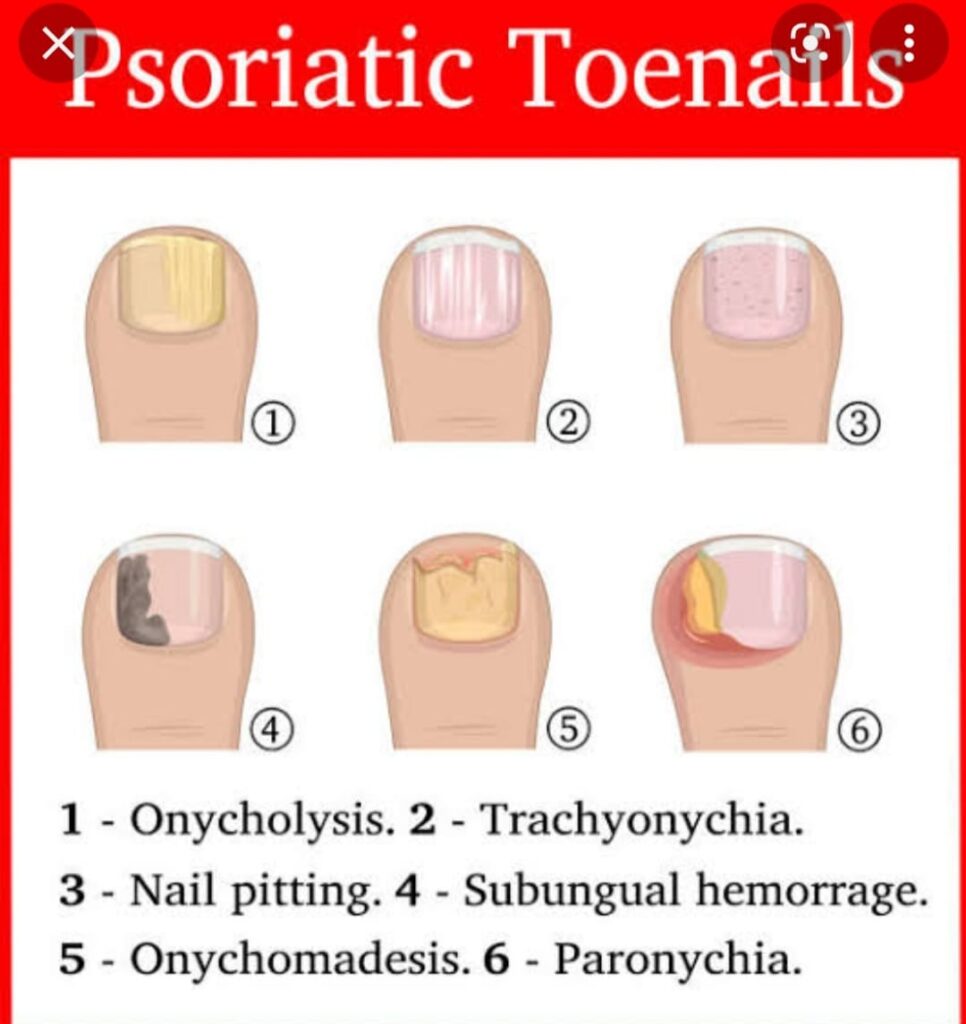
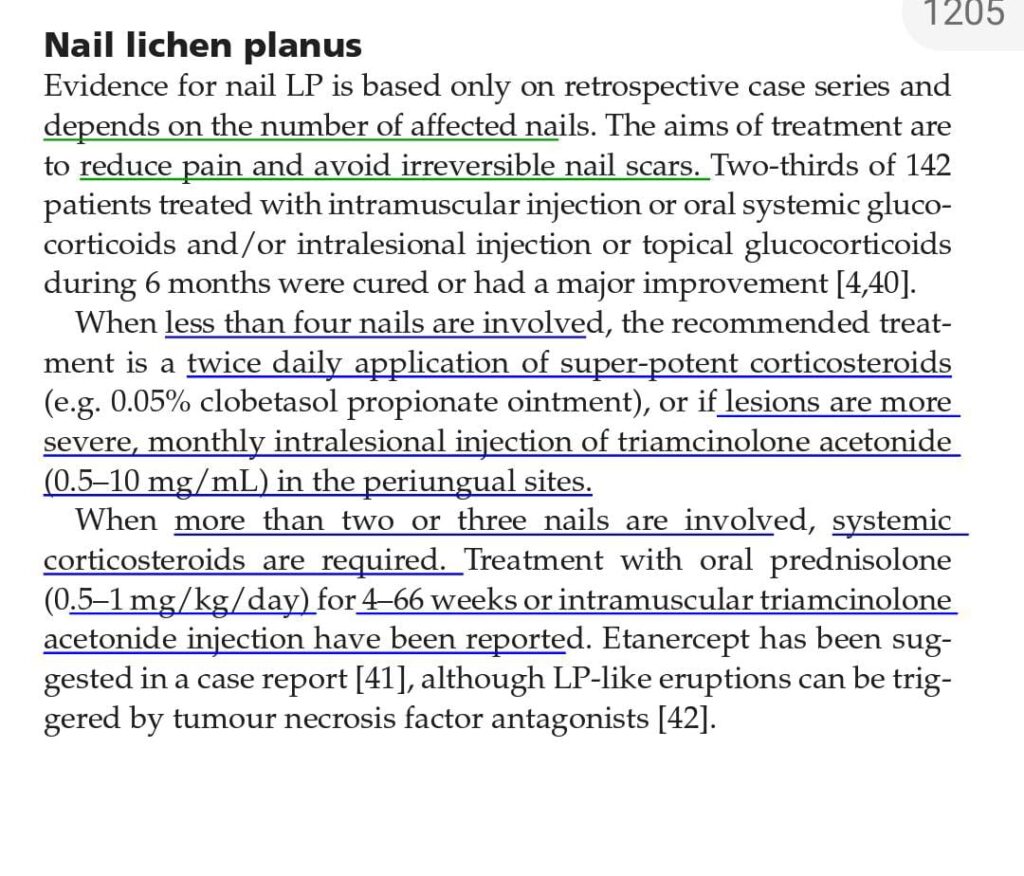
NAIL CHANGES IN LICHEN PLANUS 👇🏻
- longitudinal ridging
- Nail plate thinning
- Distal splitting of the nail plate
- onycholysis
- Subungual hyperkeratosis
- Pterygium formation
- complete nail loss, appearing as irregular grooves and pitting on the nail surface



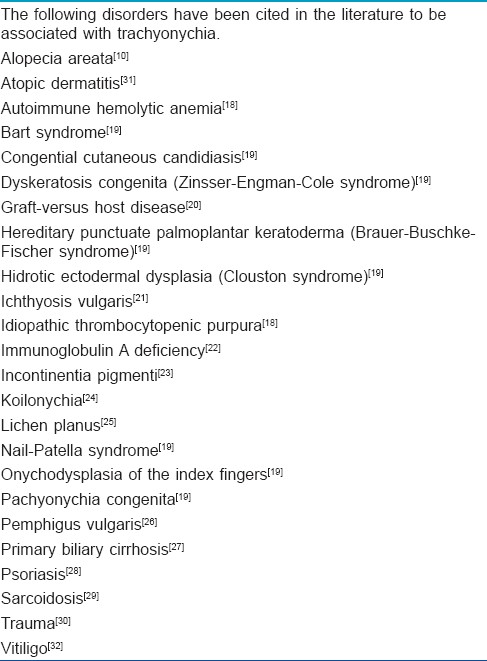
Trachyonychia
Trachyonychia is rough nail(s) with excessive longitudinal ridging due to proximal nail matrix damage.
is characterised by brittle nails that show diffuse longitudinal ridging and can be accompanied by pitting, loss of lustre, or a roughened nail plate.
Trachyonychia, also known as ‘rough nails’ or ‘sandpaper nails’, can involve any number of nails. Twenty-nail dystrophy refers to trachyonychia that affects all 20 nails.
Causes of trachyonychia
It can be idiopathic or associated with:
Alopecia areata/alopecia universalis
Lichen planus
Psoriasis
Ichthyosis vulgaris
Atopic dermatitis
Vitiligo.
🌹 LICHEN NITIDUS 🌹

NEKAM DISEASE

Associations of LP
Disease course and prognosis
Investigations
Management
Lichen striatus:

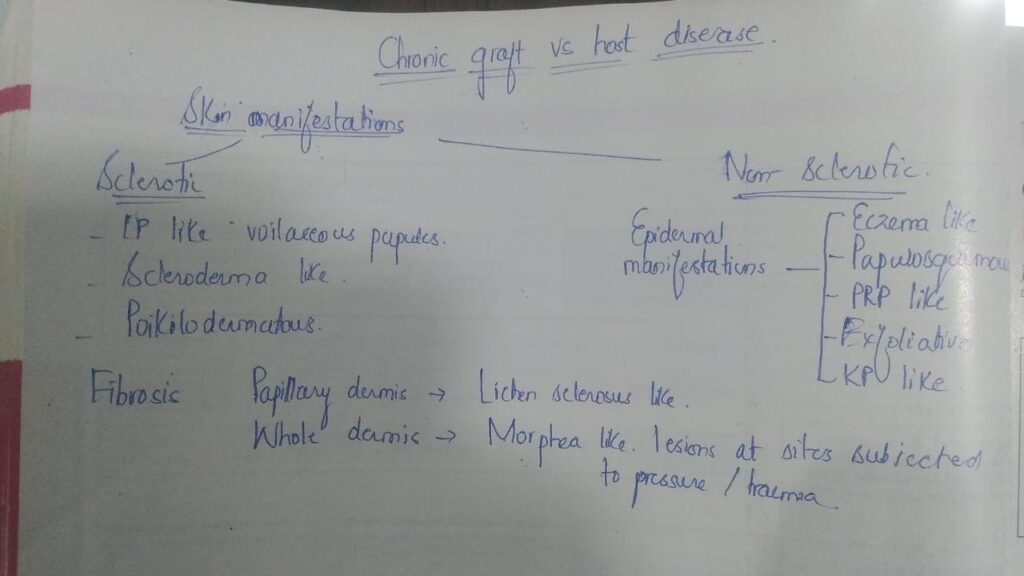
GRAFT VERSUS HOST DISEASE:
Definition
Risk factors
Pathophysiology
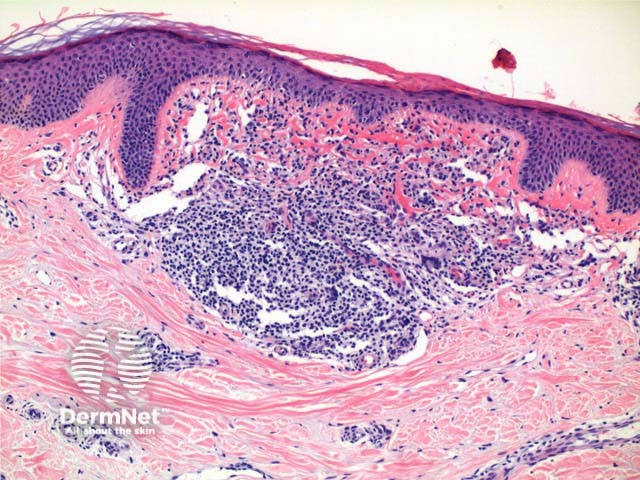
Pathology
Markers
🔰 ACUTE GVHD
Clinical features👇🏻
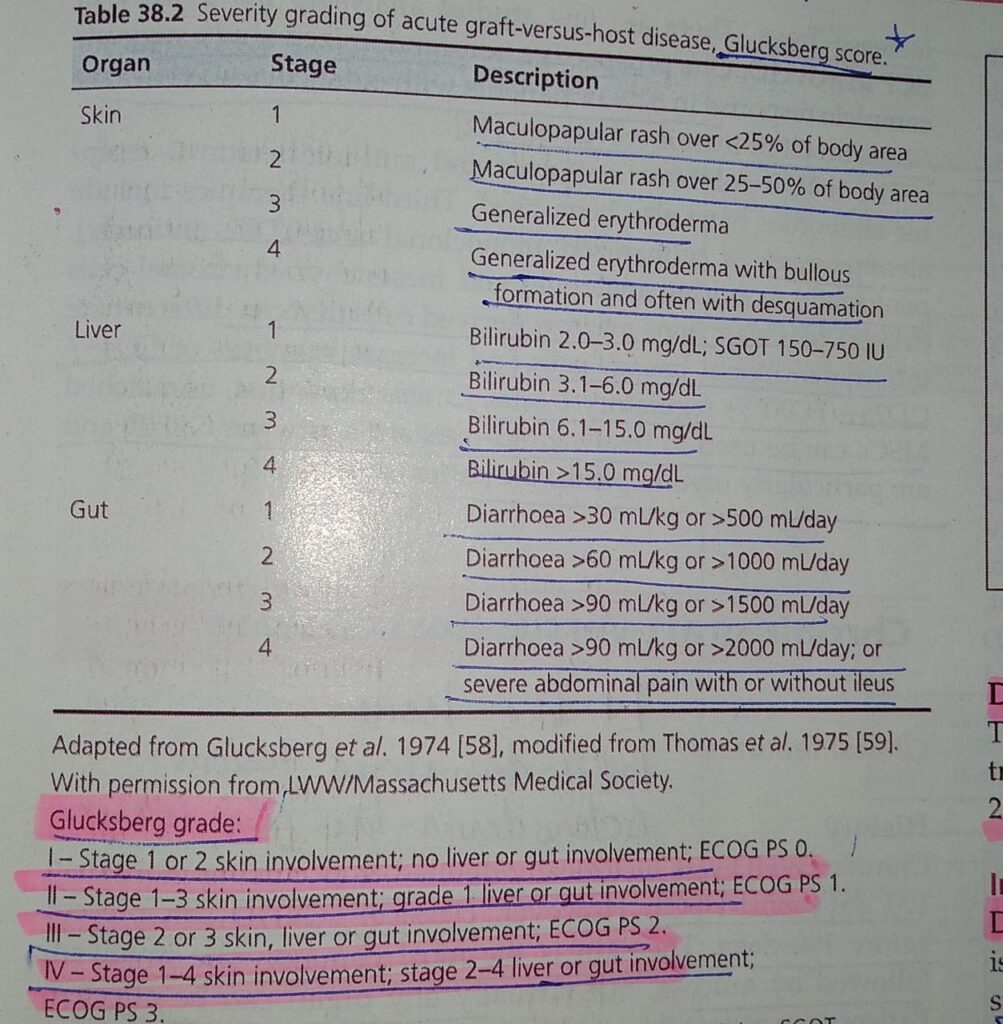
Disease course and prognosis👇🏻
Investigations
Management

🔰 CHRONIC GVHD
Management
Acute is within 90 days and chronic after 90 days
Acute tens like pic,<100days
Chronic lichenoid >100days
Acute
Maculopapular morbiliform rash
Palmo planter erythema
Ten like
Chronic
Sclerodermoid
Lichenoid
Morheaform
🔰 Acute GVHD


🔰 Chronic GVHD


🔰 *IMPORTANT*🔰
For this chap too, listen to voice notes for quick revision, memorize the tables from rooks and practice mcqs only.
🔰 Eczema can be covered well from mcqs.
Juz solve the mcqs for the safe side.
U all have managed so many pts in the opd and know well how to manage them. Dun waste ua time reading this chap from rooks.
Seborrheic dermatitis:
URTICARIA:
Subtypes of Urticaria👇🏻
Age and gender incidence 👇🏻
Associated diseases👇🏻
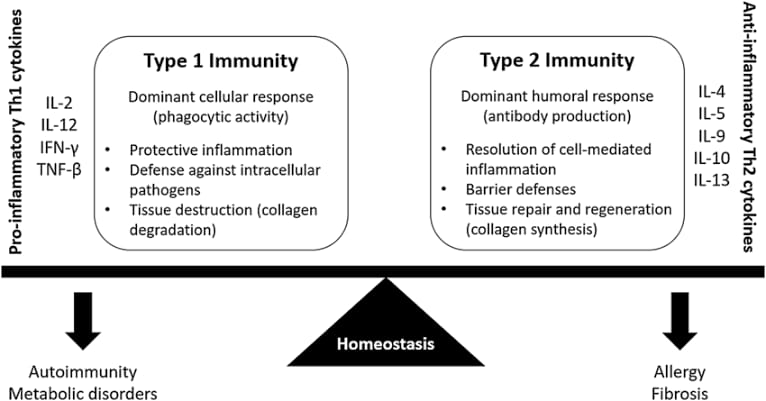
Pathophysiology 👇🏻
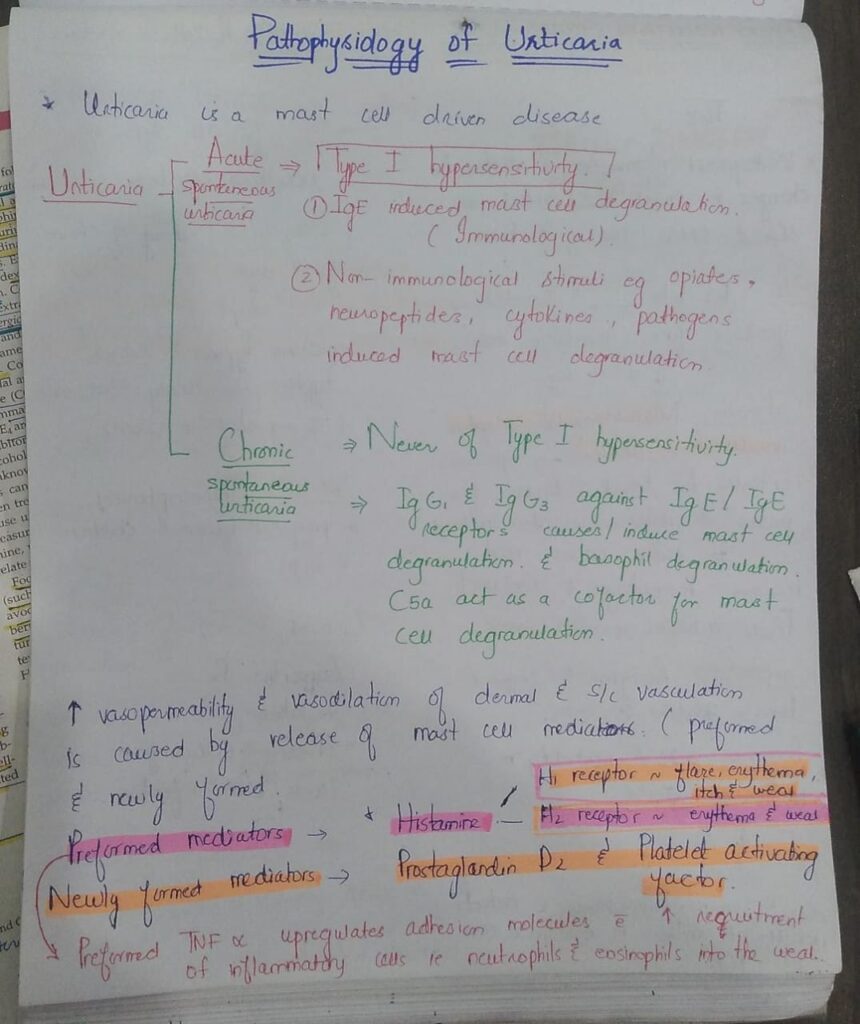

Acute spontaneous urticaria
1️⃣ Allergic / Immune mediated histamine release 👇🏻
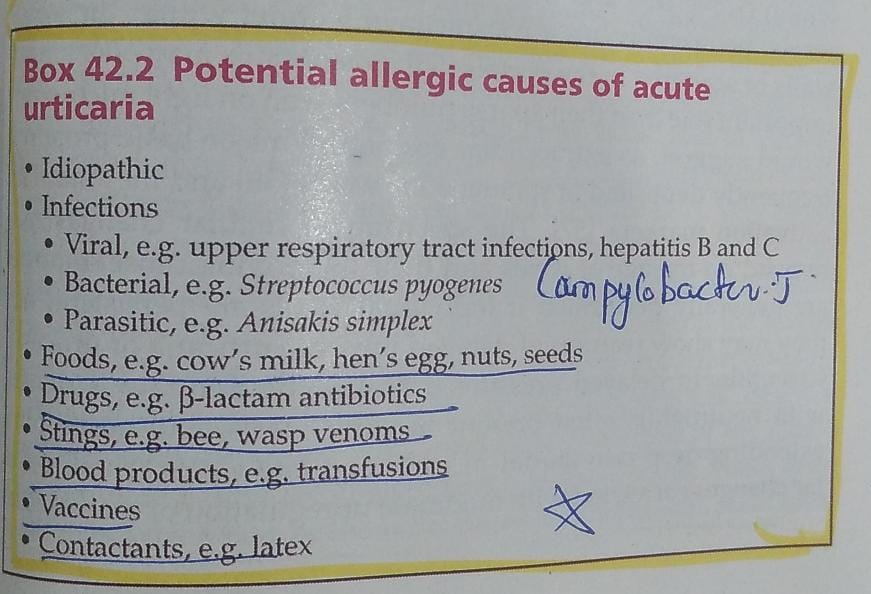
2️⃣ Non allergic/Non immune mediated histamine release👇🏻
*Chronic spontaneous urticaria*
Idiopathic
Food additives
Natural salicylates
Amines
Spices
Green tea
Alcohol
- Pylori infection
Parasitic infestation with Ancylostoma and Strongyloides

Histopathology👇🏻

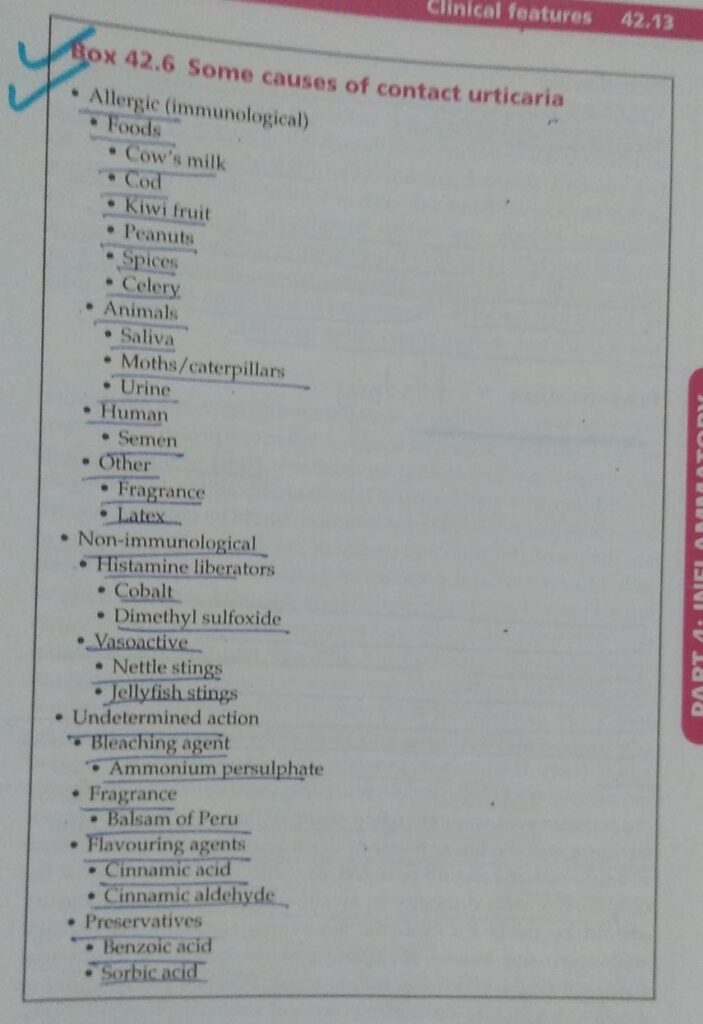
🔰 INDUCIBLE URTICARIAS 👇🏻

1️⃣ Dermographism



2️⃣ Delayed pressure urticaria

3️⃣ Vibratory angioedema
4️⃣ Temperature dependent urticaria
5️⃣ Cholinergic urticaria
6️⃣Other types of inducible urticaria
Differential diagnosis👇🏻
Course and prognosis👇🏻
Investigations 👇🏻

Management👇🏻
🔰 *Important*
For this chap “Urticaria” only listen to above voice notes and u ll never need to go through rooks for this chap.
Revise by solving mcqs from different books
Happy learning😊
URTICARIAL VASCULITIS:
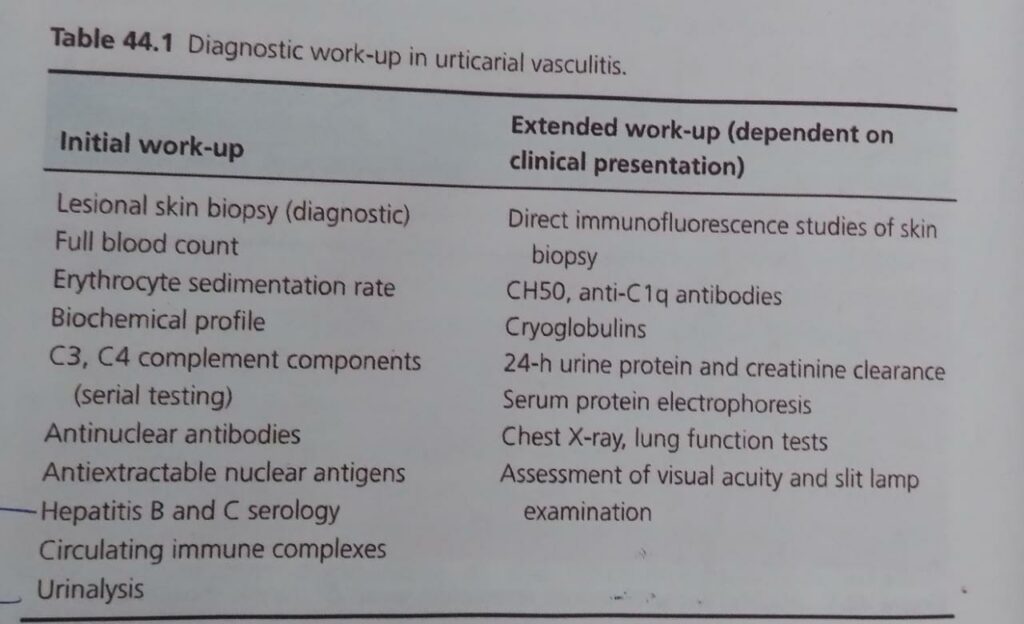
🔰 Important 🔰
For this chap👆🏻, listen to voice notes for concept and revision, then only practice mcqs
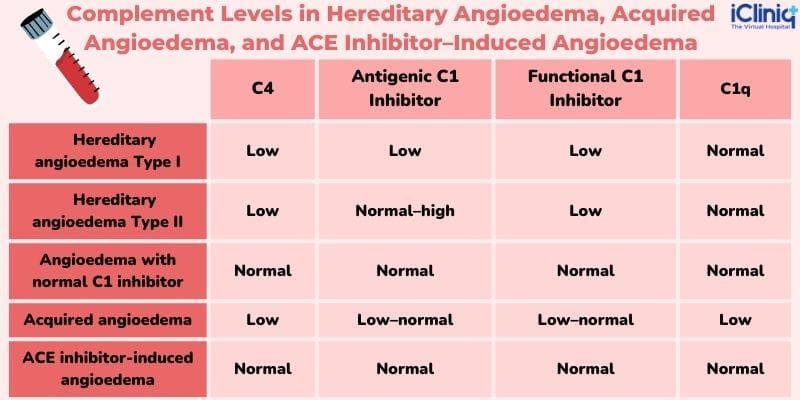
RECURRENT ANGIOEDEMA WITHOUT WEALS:
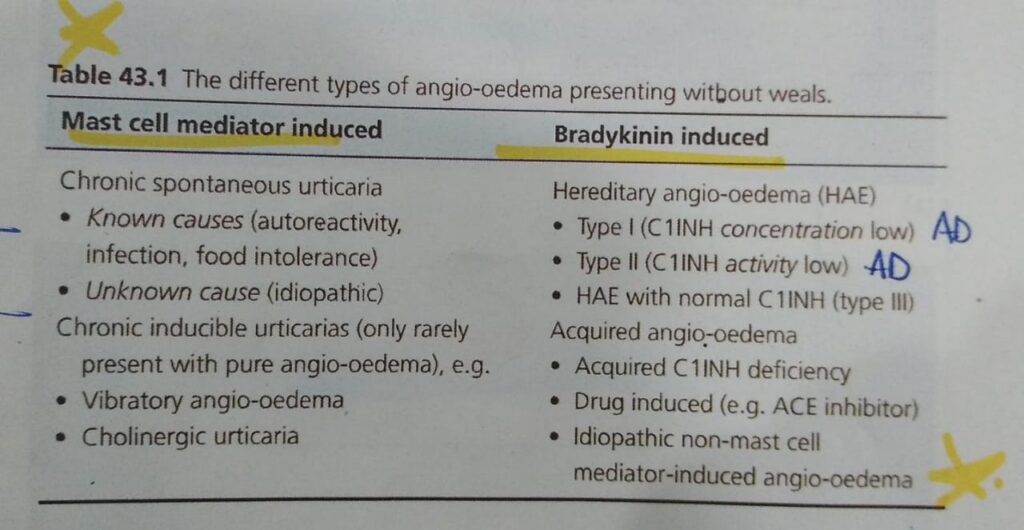
🔯 C1 esterase inhibitor,
Imp thing to memorize in this chap




Differential diagnosis👇🏻
Course and prognosis
Managment
🔰 IMPORTANT 🔰
Listen to above voice notes and solve mcqs only.
AUTOINFLAMMATORY DISEASES OF SKIN:
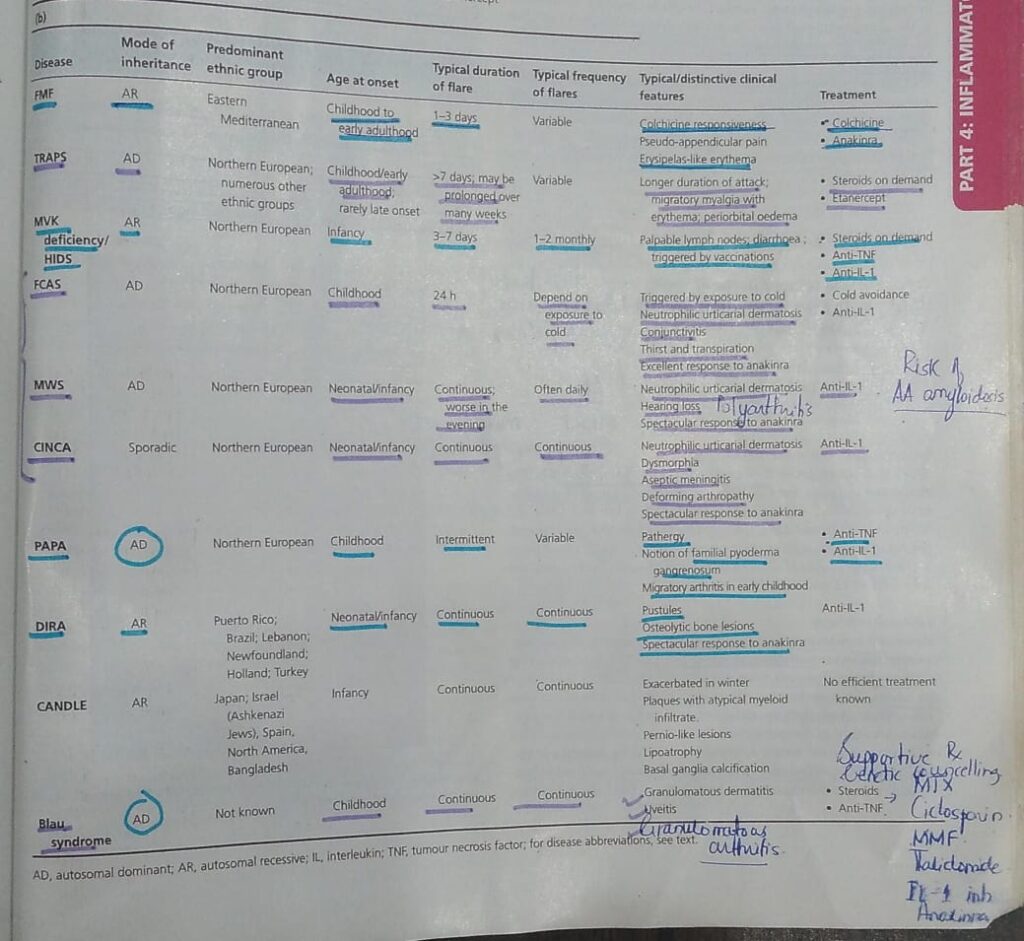
1️⃣ Familial Mediterranean fever

🔰Imp points to remember👇🏻

2️⃣ Cryopyrin associated periodic syndrome / Familial cold autoinflammatory syndrome / Muckle Wells syndrome
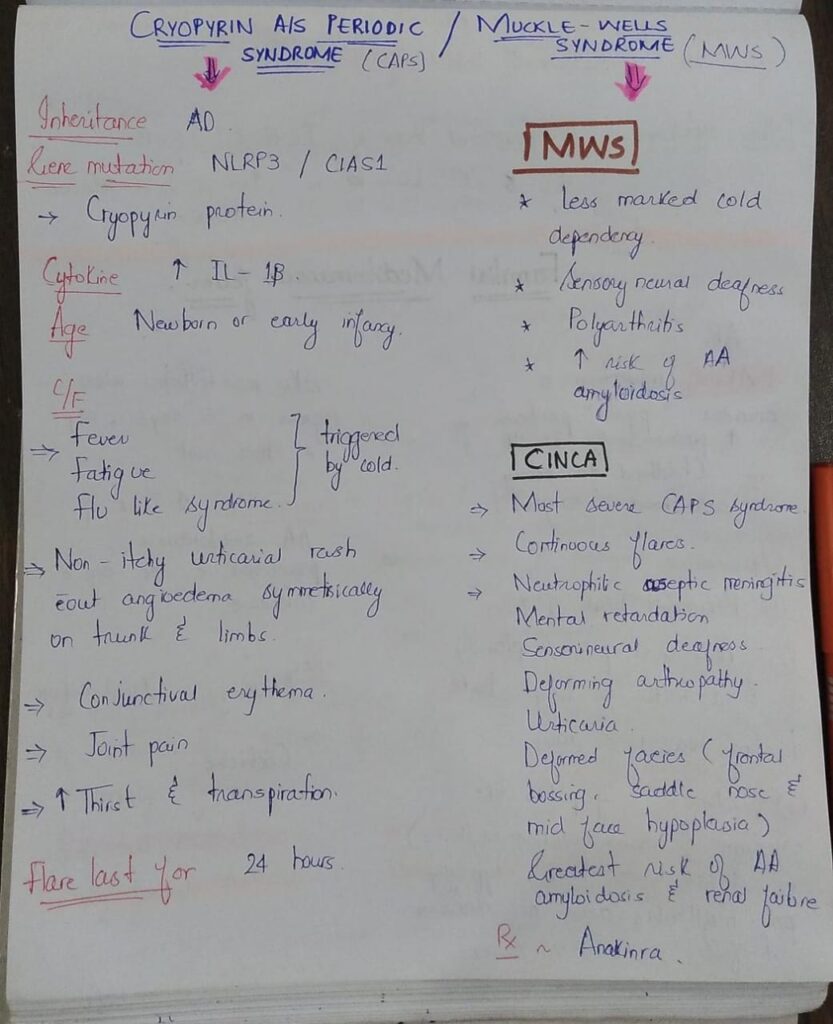
🔰Mneumonic for CAPS and Muckle Wells👆🏻

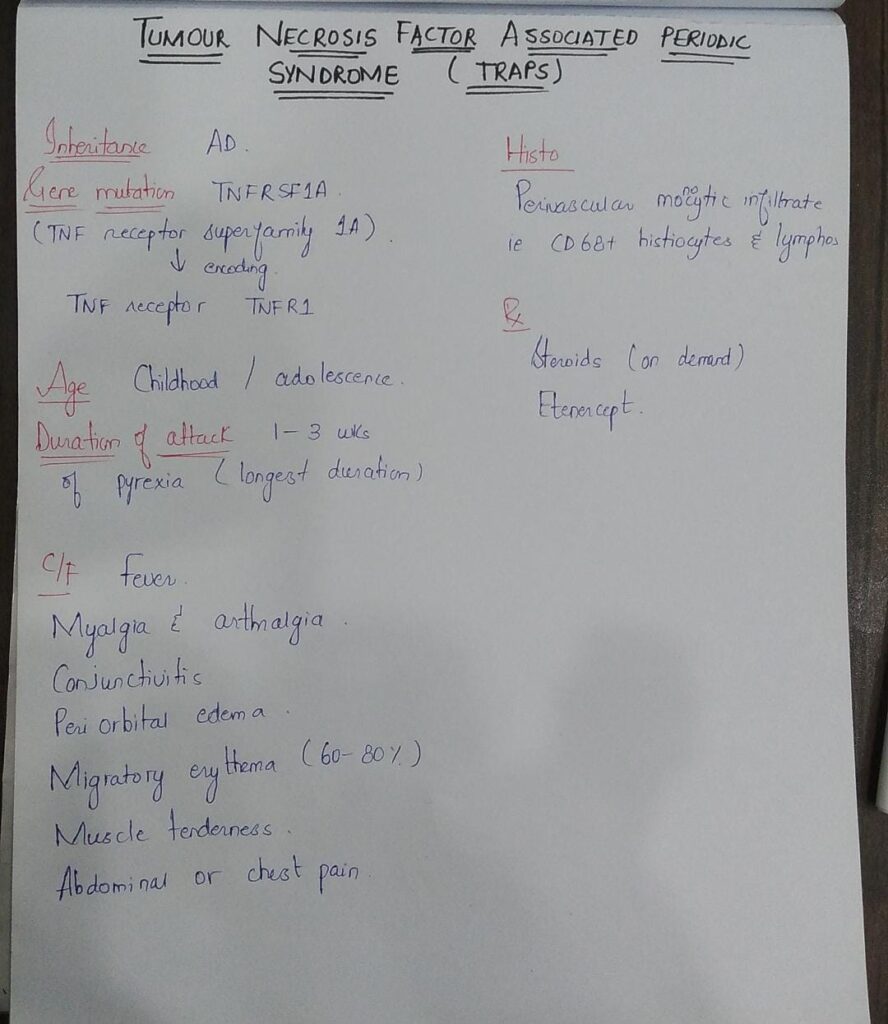
3️⃣ Tumour necrosis factor associated periodic syndrome (TRAPS)
🔰 Mneumonic👇🏻

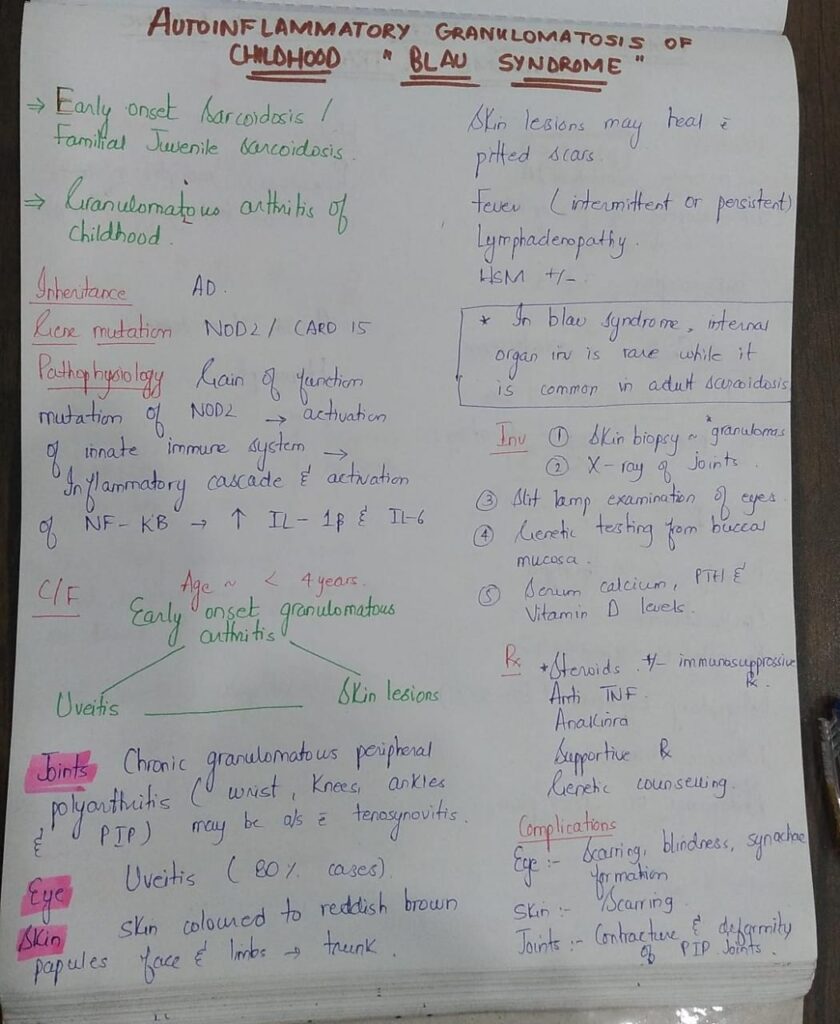
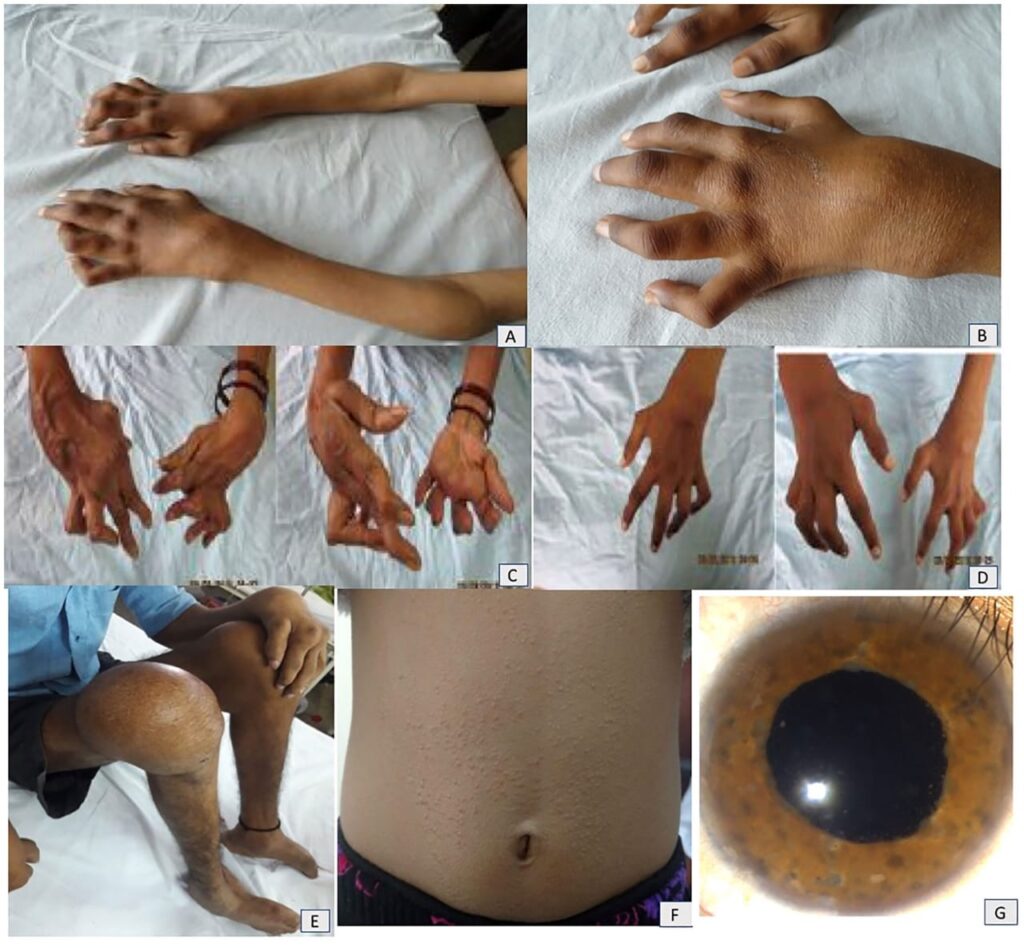
4️⃣ Blau syndrome/ Familial juvenile sarcoidosis


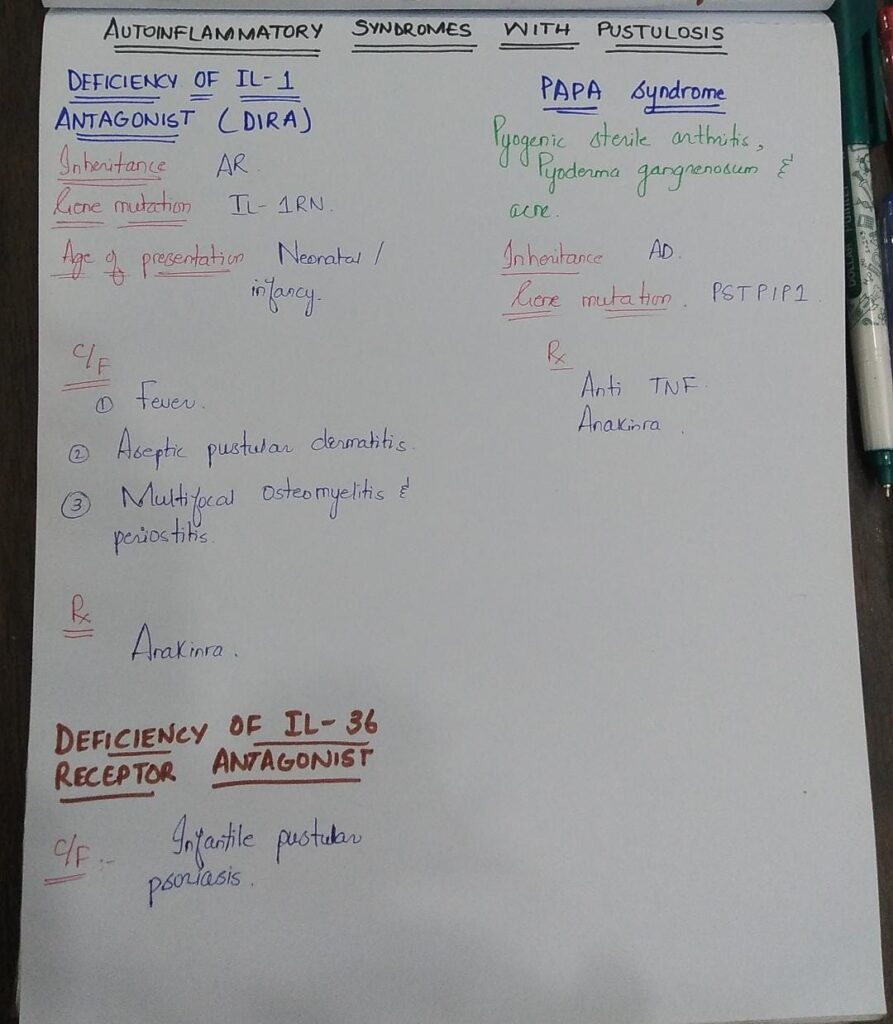
5️⃣ Autoinflammatory syndromes with pustulosis


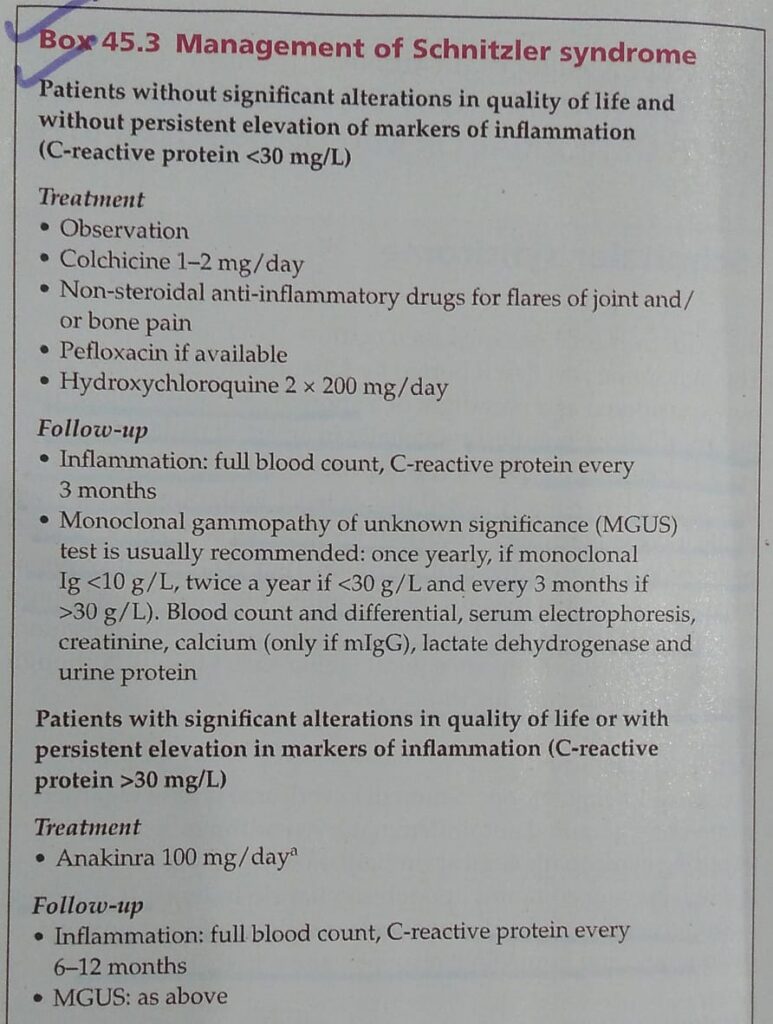
6️⃣ Schnitzler syndrome
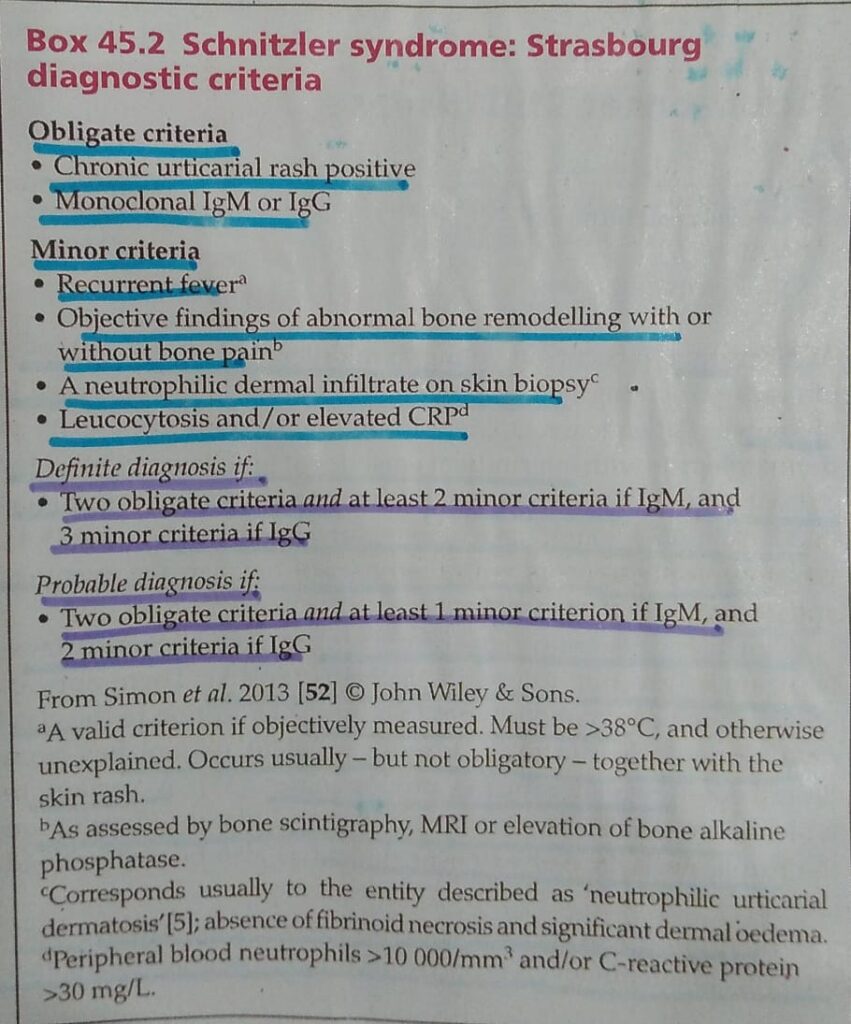
Dds👇🏻
- Adult onset Still disease
- Hypocomplementaemic urticarial vasculitis
- Cryoglobulinaemia
- SLE
7️⃣ Adult onset Still disease

🔰Summary👇🏻
DERMATOLOGICAL MANIFESTATIONS OF RHEUMATOID DISEASE:
1️⃣ Rheumatoid arthritis
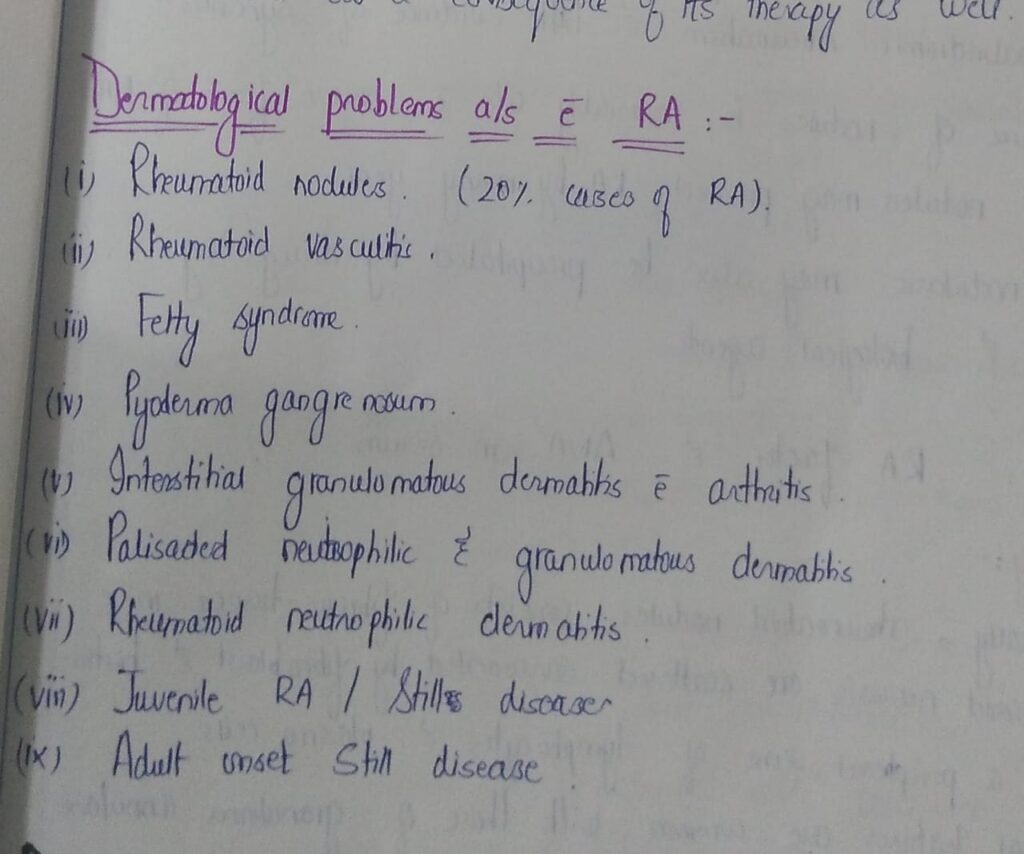
🔰Rheumatoid nodules


🔰Linear subcutaneous bands and interstitial granulomatous dermatitis

🔰 Rheumatoid neutrophilic dermatosis👇🏻

🔰 Vascular lesions in RA👇🏻
🔰Important tip to remember👇🏻


🔰 Leg ulcers👇🏻
Felty syndrome
2️⃣ Sjogren syndrome 👇🏻

Clinical features
Dds, complications and disease course/prognosis
Investigations
Management
Associations
🔰 For this chap, no need to read rooks.
Above voice notes are enough, listen and practice by solving mcqs
Happy learning😊
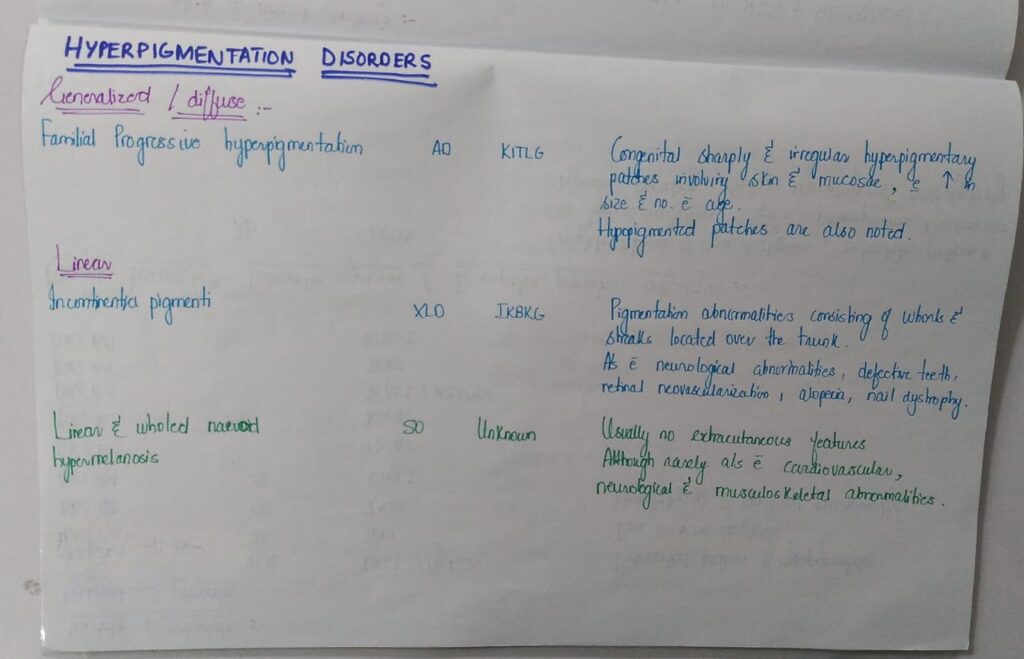
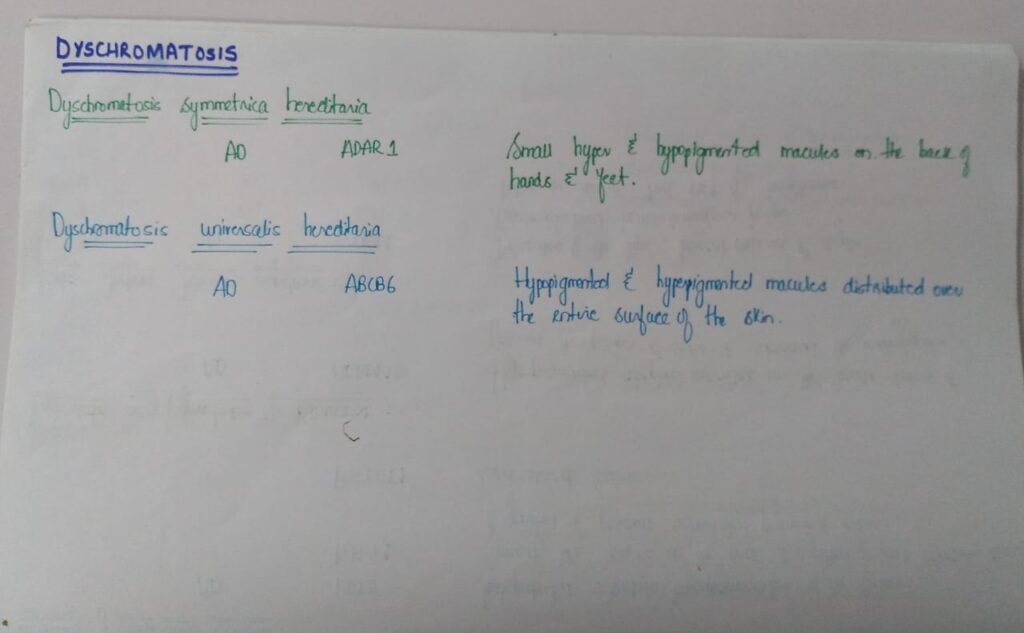
GENETIC DISORDERS OF PIGMENTATION:




🔰 Quick fix for this chap👆🏻
🔰 Important note
Above shared tables are really v helpful for a quick revision before exams.
Practice mcqs again n again fron etas and other books.
For 1st time readers listen to detailed voice notes of this chap👇🏻
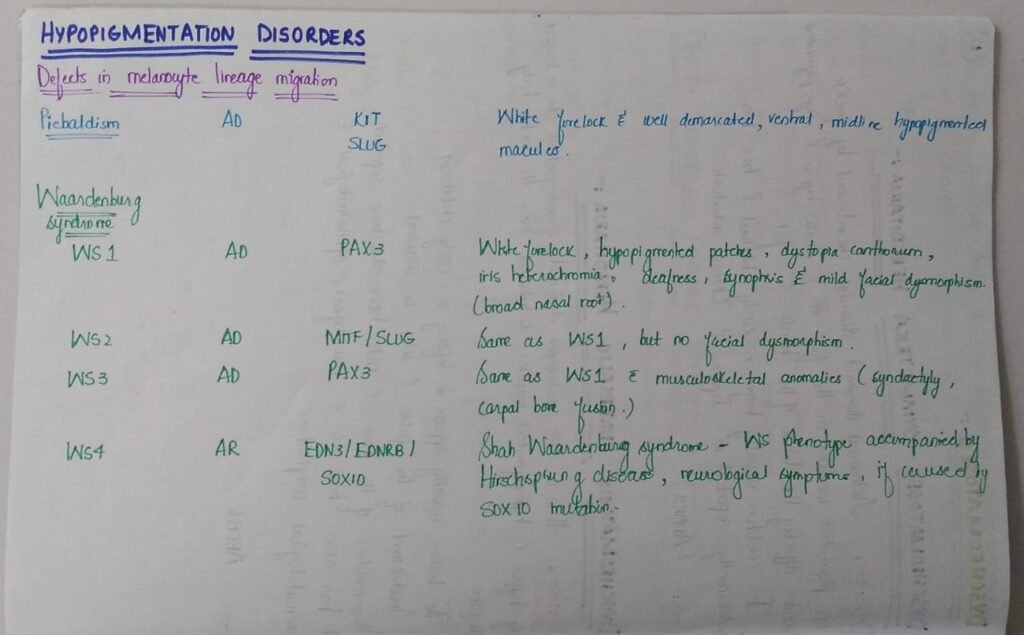
🔰 HYPOPIGMENTATION DISORDERS
1️⃣ Piebaldism 👇🏻


Waardenburg syndrome👇🏻
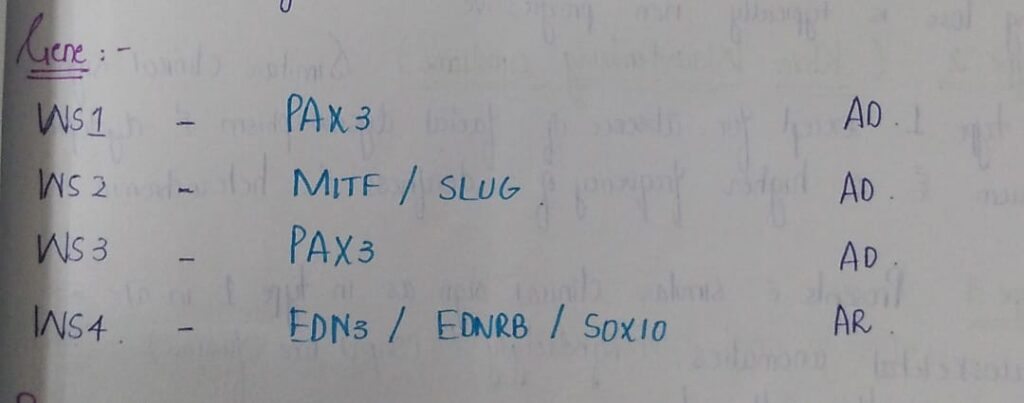

🔰 *Mneumonic* 👇🏻
Type IV is Shah sahb ( Shah wardenburg synd ) who is a bit mental (neurological symptoms ) deaf and play with Spring (hirshprungs) he buys SOX (SOX10) from Edenrobes (EDNR8)
3️⃣ Oculocutaneous albinism 👇🏻


4️⃣ Hermansky -Pudlak syndrome 👇🏻

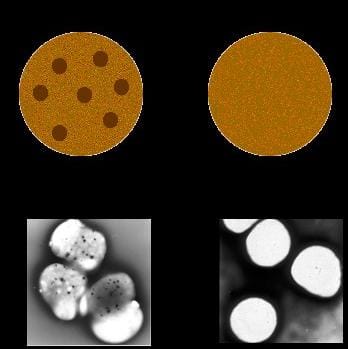
Platelets with absent dense bodies on the right side vs normal on the left
5️⃣ Chediak Higashi syndrome👇🏻
🔰 Imp for identification in toacs

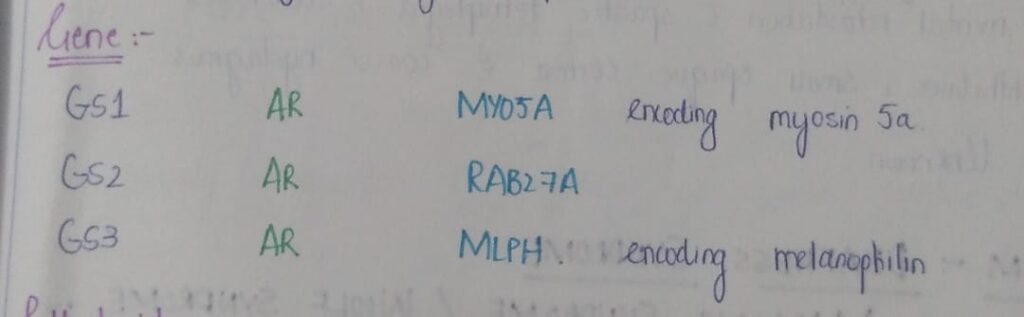
6️⃣ Griscelli Prunieras syndrome


7️⃣ Hypomelanosis of Ito👇🏻


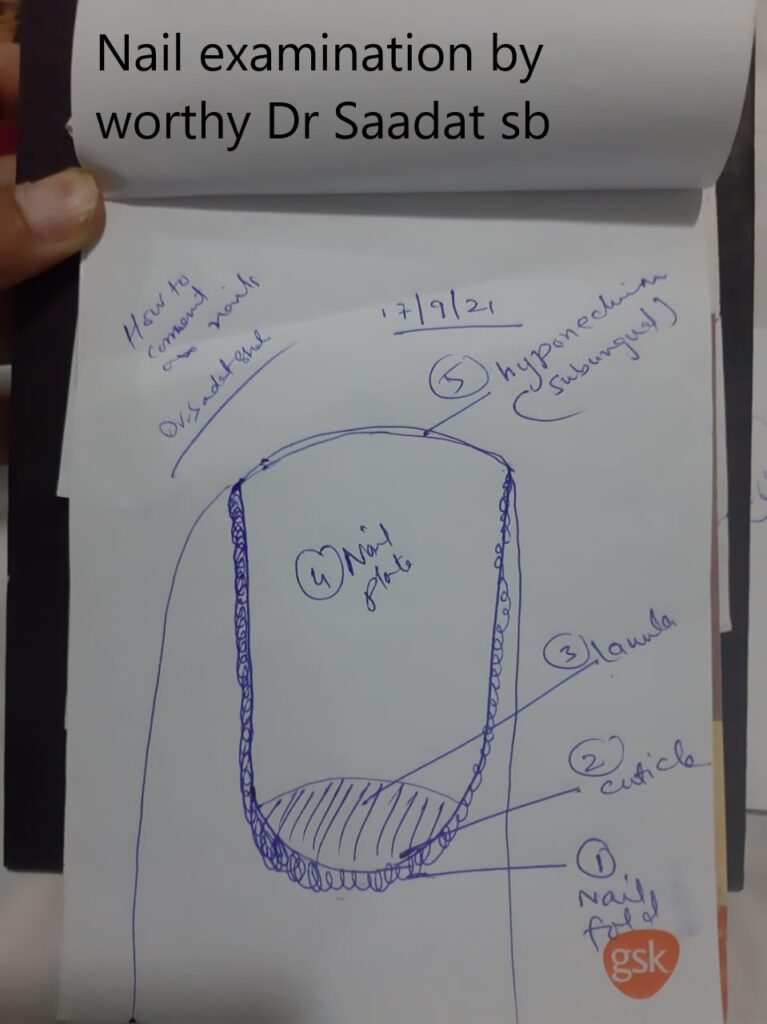
ACQUIRED DISORDERS OF NAILS AND NAIL UNITHypomelanosis of Ito:
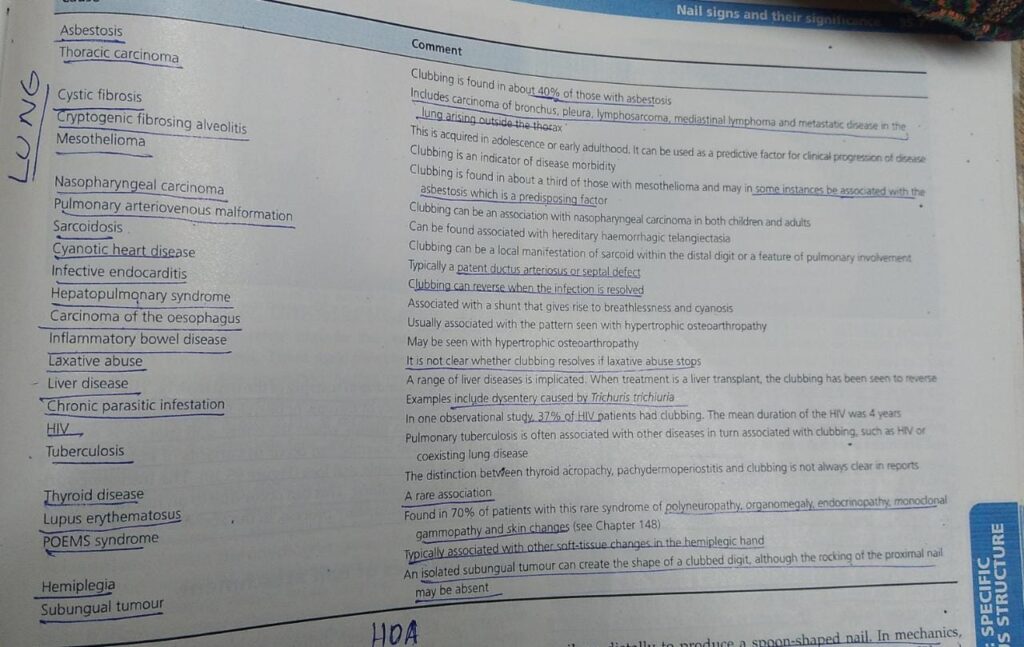
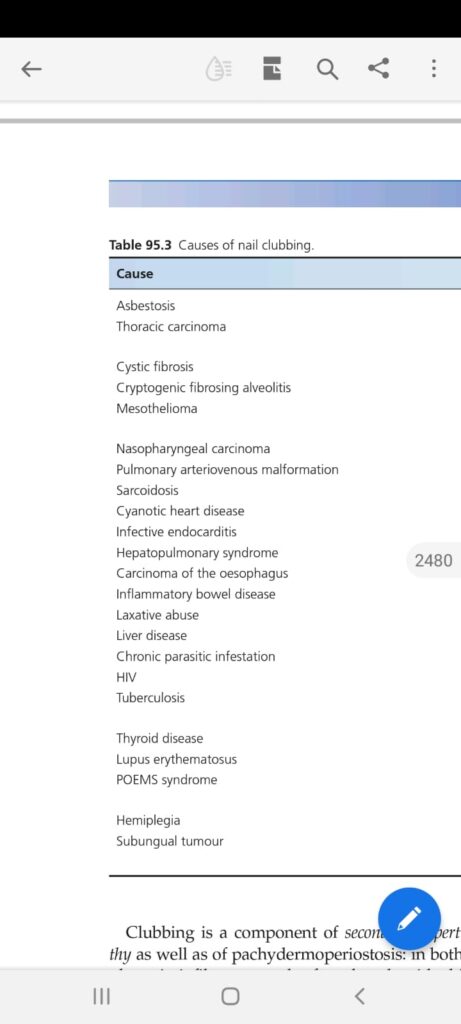
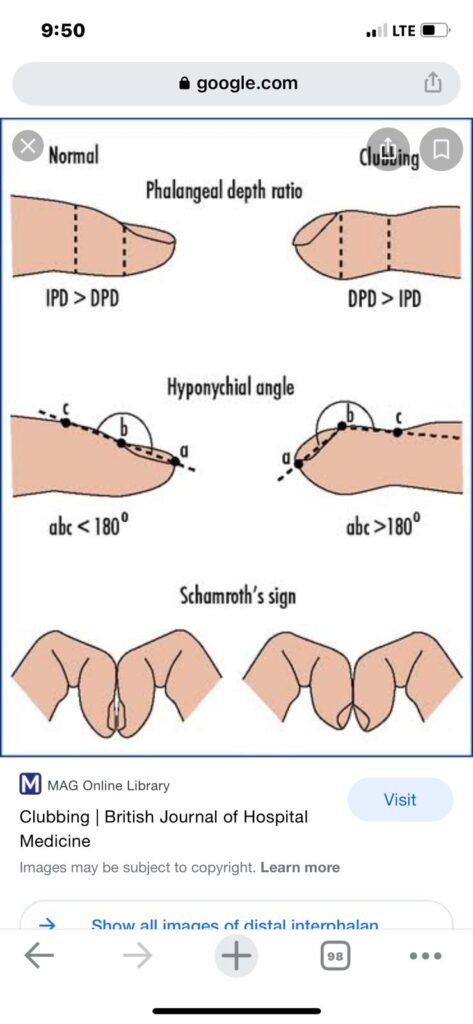
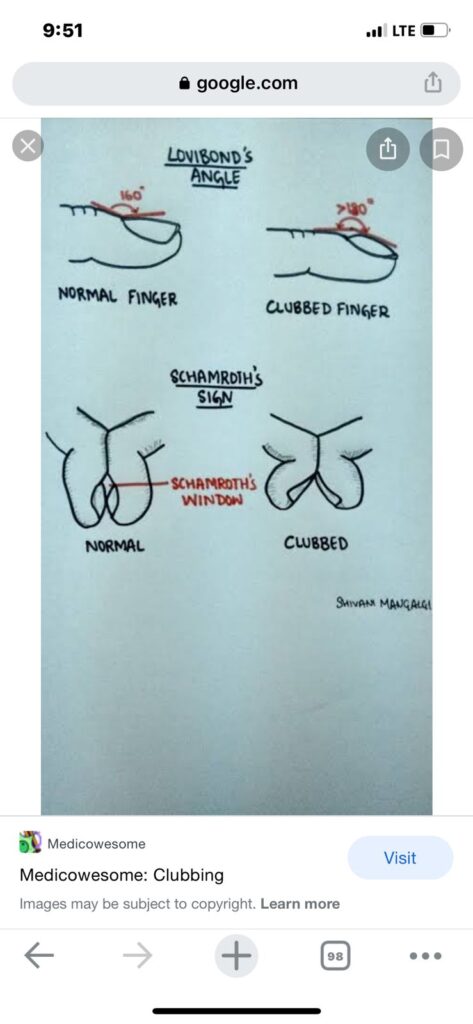
Clubbing
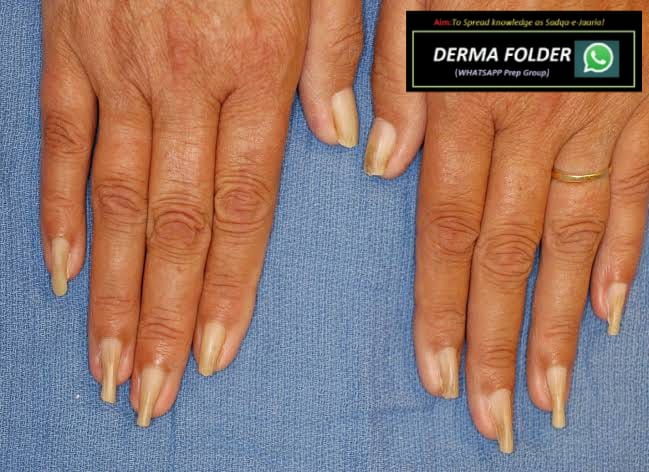
Koilonychia
Pincer nail
🔑 🗝 🔐 Pincer nails deformity
*hereditary disease*
▪️autosomal dominant Mendelian
▪️Clouston
*acquired pincer nails*
▪️gastrointestinal malignancies,
▪️renal failure,
▪️Kawasaki disease,
▪️amyotrophic lateral sclerosis, and
▪️systemic lupus erythematosus

Nail shedding

Onycholysis
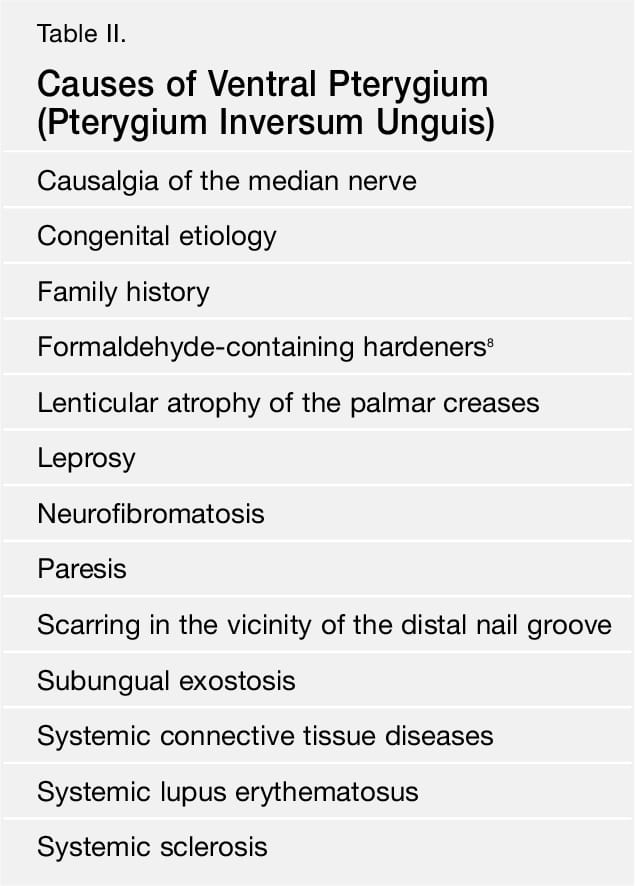
Pterygium

Longitudinal grooves👇🏻
Transverse grooves and beau’s lines

Trachyonychia

Onychoschizia/ lamellar dystrophy

Nail plate pigmentation
Subungual disturbances
Nail bed changes
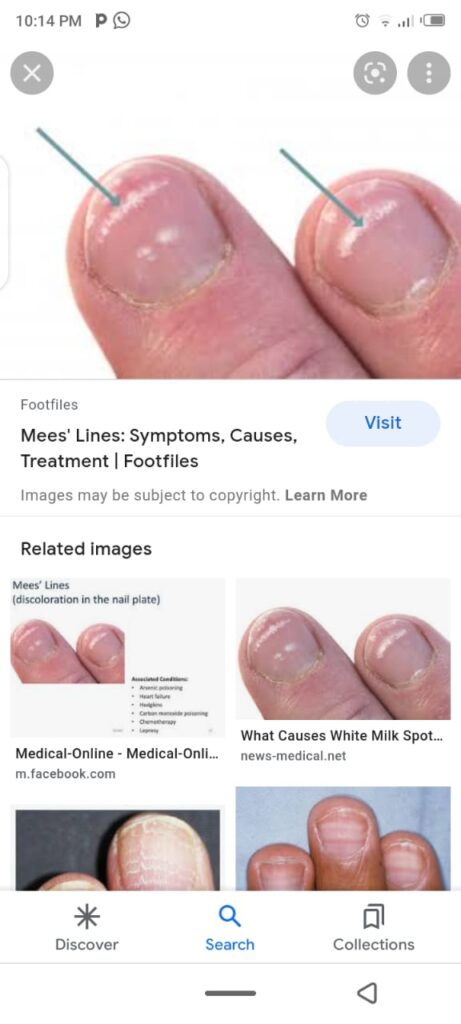
Leuconychia

Colour changes due to drugs and chemicals
YELLOW NAIL SYNDROME
Red lanulae
Longitudinal erythronychia
Splinter hemorrhage
🔰 *Causes of Splinter hemorrhage*
Liver disease
Endocarditis
Connective tissue disease
Meningococcal disease
Psittacosis
Disseminated histoplasmosis.
*Skin disease*
psoriatic nail disease
lichen planus
*Systemic diseases*
microemboli or injury to vessel walls associated with vasculitis
Primary antiphospholipid syndrome
Systemic lupus erythematosus
Raynaud disease
Behcet disease
Cutaneous vasculitis
Scurvy.
chronic kidney disease on haemodialysis or post-renal transplant
*Drugs*
Tyrosine kinase inhibitors (seen in 60–70% of patients taking sunitinib and sorafenib)
Nitrofurantoin
Ganciclovir
Terbinafine
Tetracyclines.












📝 Hutchinson eye sign …in herpes zoster ..
Hutchinson nail sign.. melanoma.. ( others are pseudo Hutchinson and micro Hutchinson)
Hutchinson triad in congenital syphilis ..
Hutchinson summer prurigo which is actinic prurigo.
Hutchinson malignant freckle which is lentigo maligna
What is the significance of this… Black streak…
*Melanonychia*
Here there can be the following *possibilities*
*1.functionsl melanonychia* ( melanocyte activation,common in dark individuals, can be due to trauma ,)
*2.melanocytic nevi*
*3.inflammatory skin conditions* like lp and other pigmentary disorders which can be correlated clinically)
The pigmentation varies from brown dark brown to black
Pseudo Hutchinson can be seen too.
Most commonly involves thumb but other nails can be involved as well
*_Mostly a naevi in matrix !*_
mostly these are *matrix naevi* leading to band, so focal matrix ablation might lead a nail plate dystophy lateron which might look uglier than this
Would the nail appearance be normal after this procedure and complete healing?
*Yes only the transverse lenght* *will be shortened* , rest it will be perfact
Grabbing this opportunity to revise *ABCDEFGHI* , to R/O *subungual melanoma* in such cases
*A: Age (* 50–70 years old); African, Japanese, Chinese, and Native American heritage
*B: Brown-black* pigmented band ≥3mm with blurred borders
*C: Change or lack of change* despite treatment in the nail band or nail morphology
*D: Digit most* commonly involved (thumb, big toe, or index finger)
*E: Extension* of pigment into the skin surrounding the nail (Hutchinson sign)
*F: Family or personal history* of melanoma or dysplastic nevus (atypical mole)
*G – Geometry* of lesion like triangular band
*H – Hyponychial involvement*
*I – irregular pigment pattern* (like different color bands) , irregular spaces , irregular thickness




🔰 Racquet nails
🟥 *causes?* 🔑
*Genetic disorders*
▪️Larsen syndrome,
▪️Brooke–Spiegler syndrome,
▪️Rubinstein–Taybi syndrome,
▪️Hajdu–Cheney syndrome,
▪️cartilage–hair hypoplasia,
▪️pycnodysostosis,
▪️acrodysostosis,
▪️brachydactyly type D.
*Acquired racquet nail*
associated with
▪️acroosteolysis and
▪️psoriatic arthropathy.
▪️diagnostic of bone resorption in hyperparathyroidism.

Anonychia


🔰 Important tip for this chap👇🏻
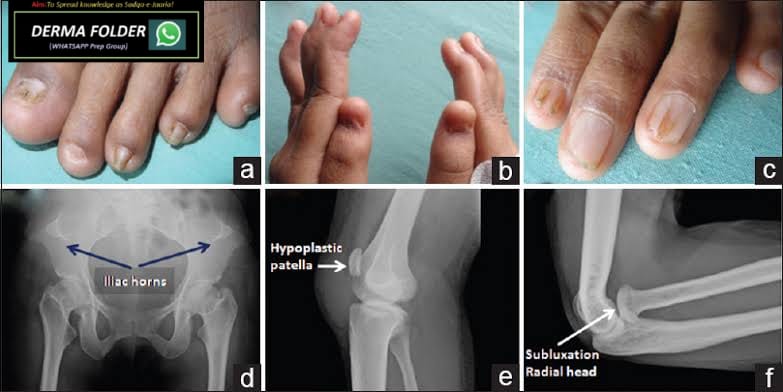
Leprosy
Joplings
Clinical features
- Indeterminate leprosy
- Tuberculoid leprosy👇🏻

- Borderline leprosy👇🏻


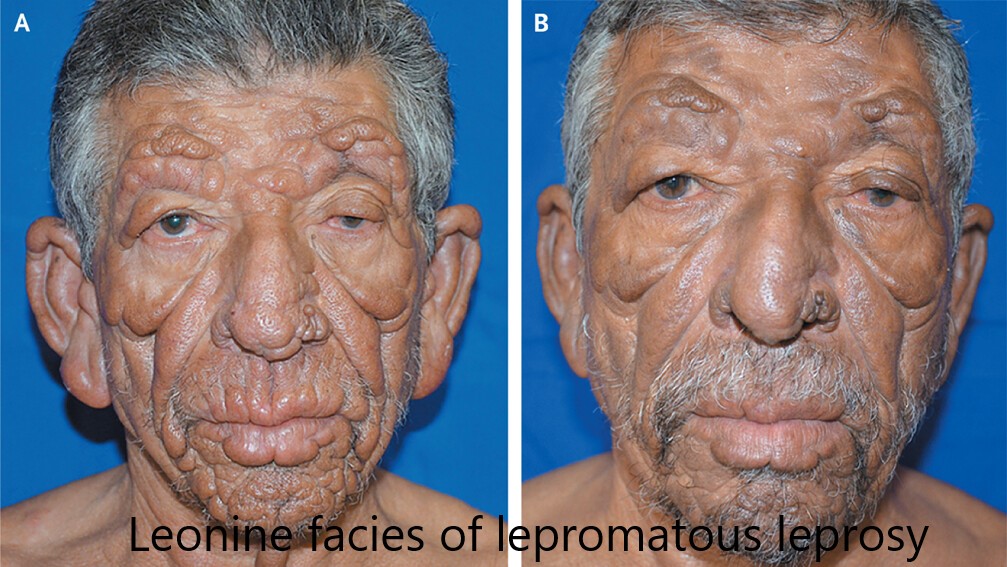
Lepromatous leprosy👇🏻
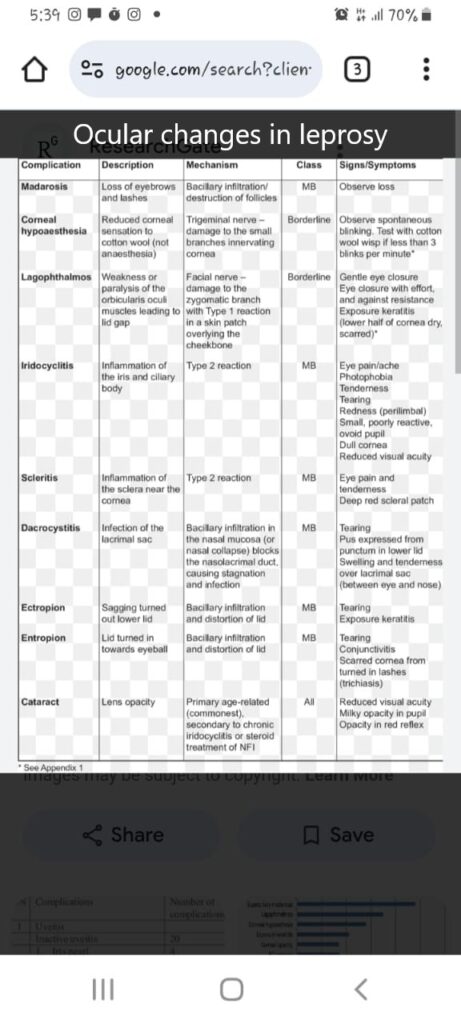
Nerve involvement in leprosy👇🏻
Systemic involvement👇🏻
Bone changes👇🏻
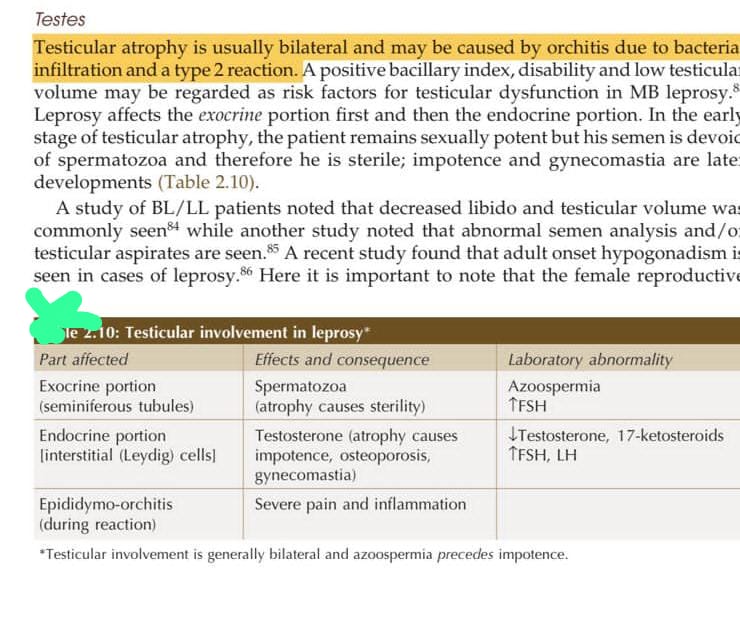
Testes changes👇🏻
Renal involvement👇🏻
Muscle and lymph node 👇🏻
Other systemic involvement in leprosy👇🏻
Cause of death in leprosy👇🏻
Uncommon presentations of MB leprosy👇🏻
🔰 Chap 2 Relapse, reactivation, reaction and reinfection 👇🏻👇🏻
Chap 2.3 LEPROSY IN CHILDREN
Chap 2.4 PURE NEURITIC LEPROSY👇🏻
Chap 2.5 SPECIAL SCENARIOS 👇🏻👇🏻
Chap 3.2 HISTOPATHOLOGY OF LEPROSY👇🏻👇🏻
Indeterminate leprosy👇🏻
Primary Tuberculoid leprosy👇🏻
Secondary Tuberculoid leprosy👇🏻
Borderline tuberculoid👇🏻
Borderline lepromatous leprosy👇🏻
Lepromatous leprosy👇🏻
Histo of Tuberculoid leprosy👆🏻
Histopathology of lepromatous leprosy👆🏻

🔰 REACTIONS IN LEPROSY
Chap 5 Reactions in leprosy👇🏻
Type 1 reaction👇🏻

Type 2 reaction👇🏻
Lucio phenomenon

Acute exacerbation 👇🏻
Diagnosis
Immunology👇🏻
Immunology👇🏻
Treatment👇🏻

🔰 Important note
This detailed explanation of leprosy is only for those who wanna go through joplings
Juz listen to these once.
For exam, only go through the voice notes of leprosy given in long case grp, go through the tables of jopling only and listen to dr Asher’s video on leprosy.
Tht wud be more than enough
INFLAMMATORY DERMATOSES:
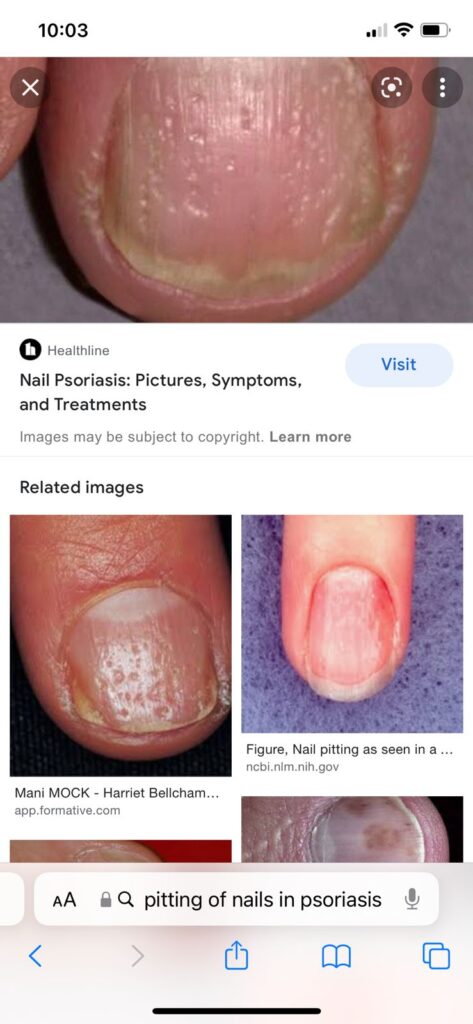
PSORIASIS
Pathogenesis of Psoriasis👇🏻

🔰 Pustular psoriasis
General discussion👇🏻
More detail👇🏻
PALMOPLANTAR PUSTULOSIS👇🏻
Acrodermatitis continua of Hallopeau👇🏻
🔰 PSORIATIC ARTHRITIS👇🏻
General discussion👇🏻


🔰 Imp for identification in toacs
Other specified forms of psoriasis
Classification of severity

https://youtu.be/a8FCOK_21Y8?si=niqKuu1nwERSkzWA
Modified napsi score 👇🏻
onycholysis or oil-drop dyschromia
0 No onycholysis or oil drop dyschromia present
1–10%
2 11–30%
3 > 30%
Pitting
0 0
1 1–10
2 11–49
3 > 50
Score Percent of nail with crumbling present
0 No crumbling
1 1–25%
2 26–50%
3 > 50%
Following findings can be graded as
0 absent
1 present
Leukonychia:
Splinter hemorrhages:
Red spots in the lunula:
Differential diagnosis of psoriasis
Complications and comorbidities👇🏻
Disease course and prognosis👇🏻
Investigations👇🏻

Management👇🏻
General discussion
More detail👇🏻




PHOTOTHERAPY

UVB PHOTOTHERAPY👇🏻


UVB combination therapies
Targeted phototherapy
Excimer laser

GRENZ RAY THERAPY
PUVA PHOTOCHEMOTHERAPY👇🏻
Summary of PUVA
Topical preparations for psoriasis👇🏻
Psoriatic ointment
Clobetasol 25%
Salicylic acid 3%
Liquor pices carbonis 5%
WSP 67%
Lassar paste
Zinc oxide 24%
Starch 24%
Salicylic acid 2%
WSP 50%
*Treatment of patients with TB along with psoriasis*
ATT give 1 month of ATT followed by both ATT and immunosuppressive therapy or biologics with close monitoring
Preferred treatment is
Phototherapy
Acitretin
Apremilast
Secukinumab
*Treatment options in patients of hiv with psoriasis..*
Antiretroviral therapy
Topical therapies with following
Retinoid
Phototherapy
Apremilast
Secukinumab
Less favourable options MTX, Cyclosperin, TNF inh and ustekinumab
*Treatment options in hep b/c patients with psoriasis*
Systemic therapy
Acitretin
Ciclosporin
Apremilast
Biologics esp etenercept
Ustekinumab, secukinumab, ixekizumab and brodalumab
*Do not prescribe MTX*
*Treatment of Psoriasis and malignancy*
TNF inh
Ustekinumab
Apremilast
Acitretin
*Treatment options in children*
Topical calcineurin inh for face and intertriginous areas
Vit D analogues +/- mid potency steroids
Mtx
Ciclosporin
Etanrecept greater then 5 yr children
Ustekinumab greater then 12 yr old child
*Treatment options in pregnancy*
NB UVB Phototherapy
Ciclosporin (Category C drug)
TNF inh (discontinue at 30 weeks of gestation).live vaccine to infant is postponed till 7th month of age
Topical agents
Systemic steroid only in pustular psoriasis
🔰 *IMPORTANT*👇🏻
Psoriasis is indeed the most important chap. U can never pass the exam without mastering this very disease.
For theory listen to above voice notes once to have the concept. If needed u may go through rooks after these.
Once done, practice by solving mcqs and revise psoriasis from long case grp which is focussed more on the management part of psoriasis which is most frequently asked in exams. Save time and energy.
Happy learning 😊
CUTANEOUS PHOTOSENSITIVITY DISEASES:

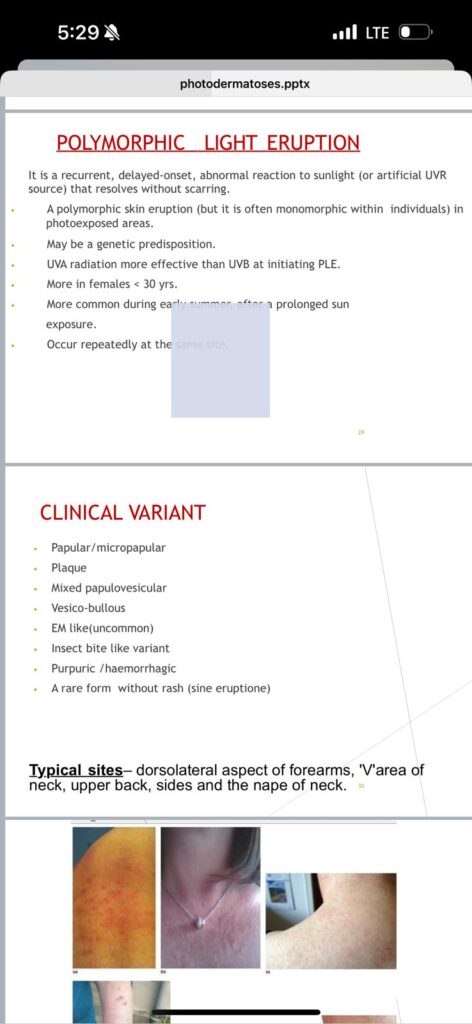
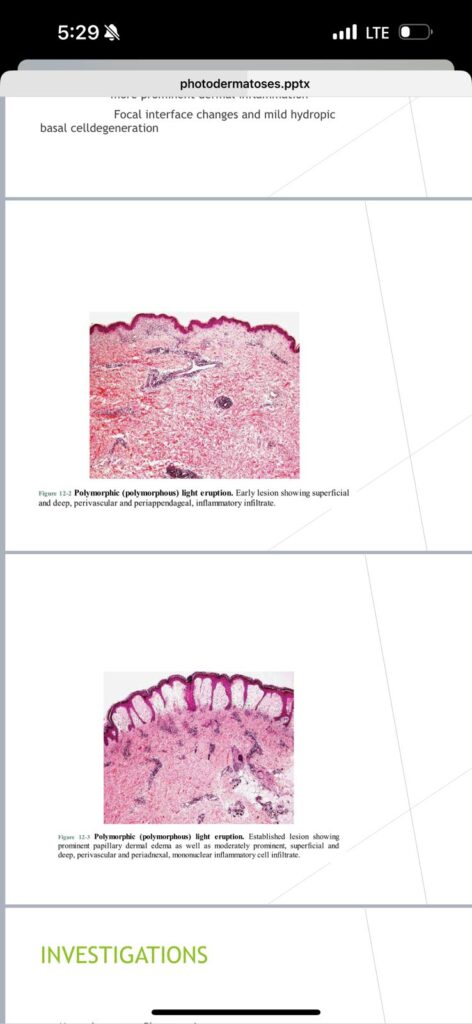
1️⃣ Polymorphic light eruption👇🏻
Predisposing factors👇🏻
Clinical presentation👇🏻



Differential diagnosis👇🏻
Disease course and prognosis👇🏻
Complications👇🏻
Investigations👇🏻
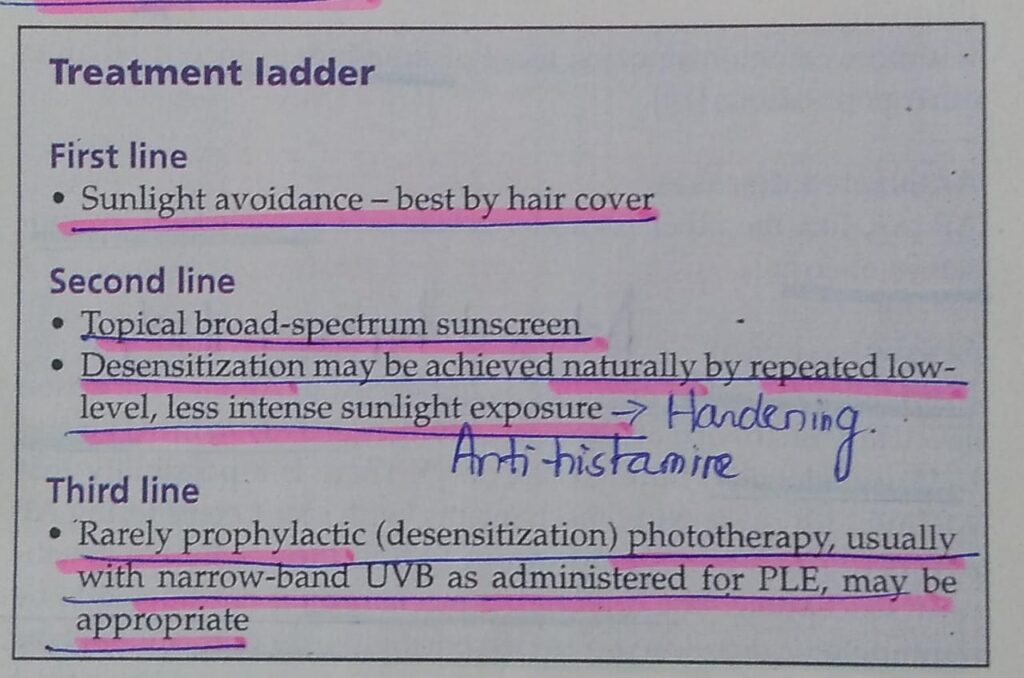
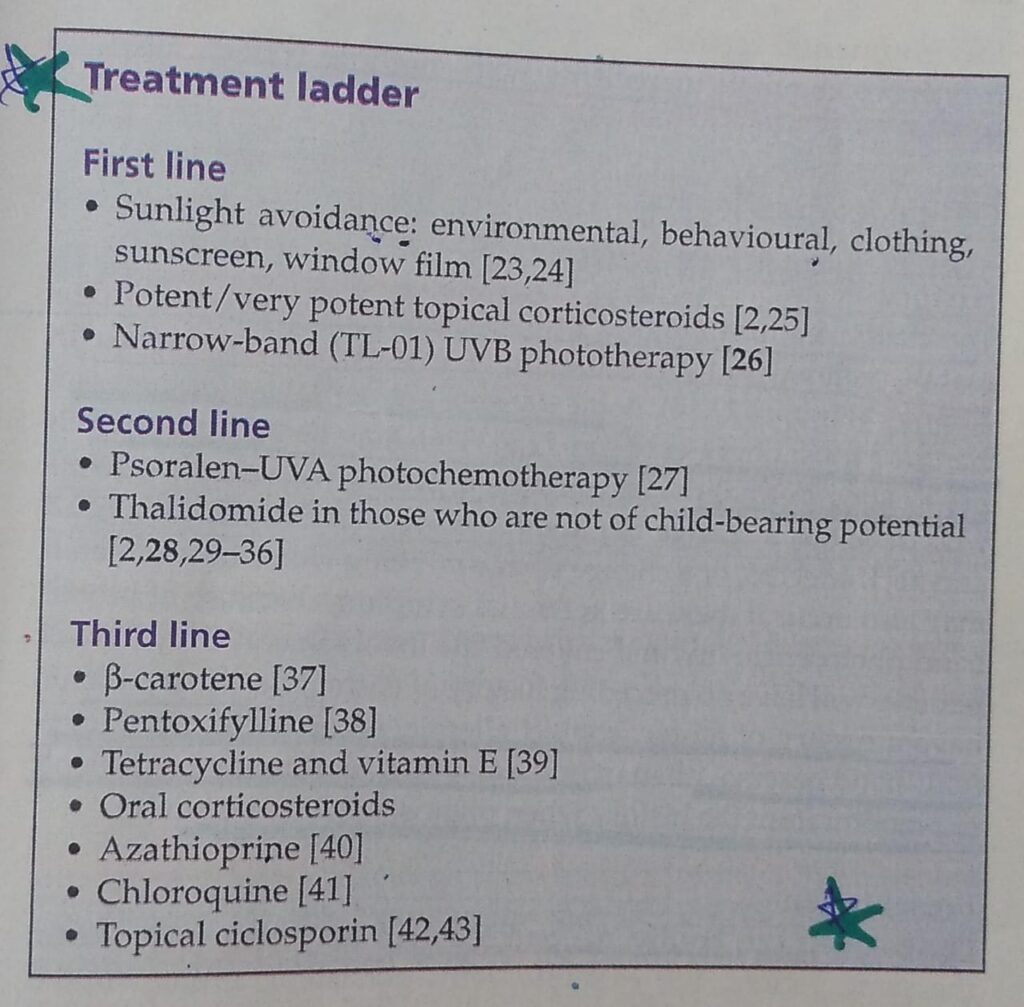
Management👇🏻
Juvenile springtime eruption:

Actinic prurigo:

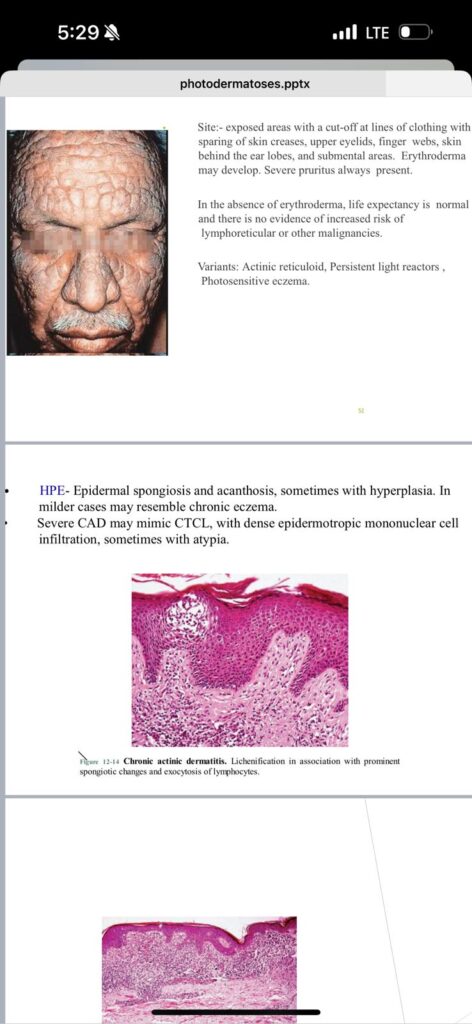
Chronic actinic dermatitis:




Solar urticaria:


Clinical variants👇🏻
Differential diagnosis👇🏻
Severity assessment, complications and disease course👇🏻
Investigations
Management
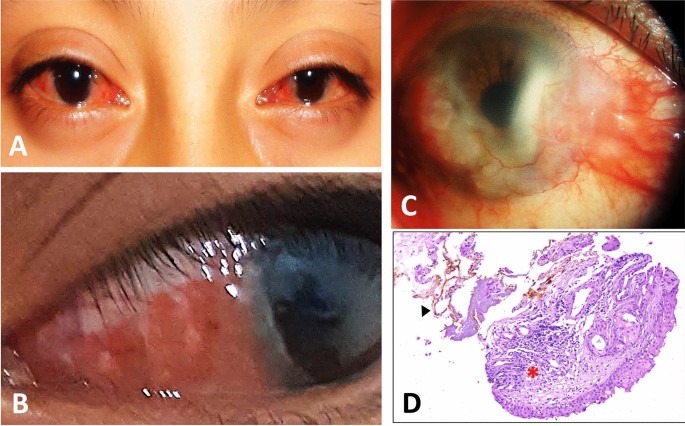
6️⃣ Hydroa vacciniforme👇🏻



Management
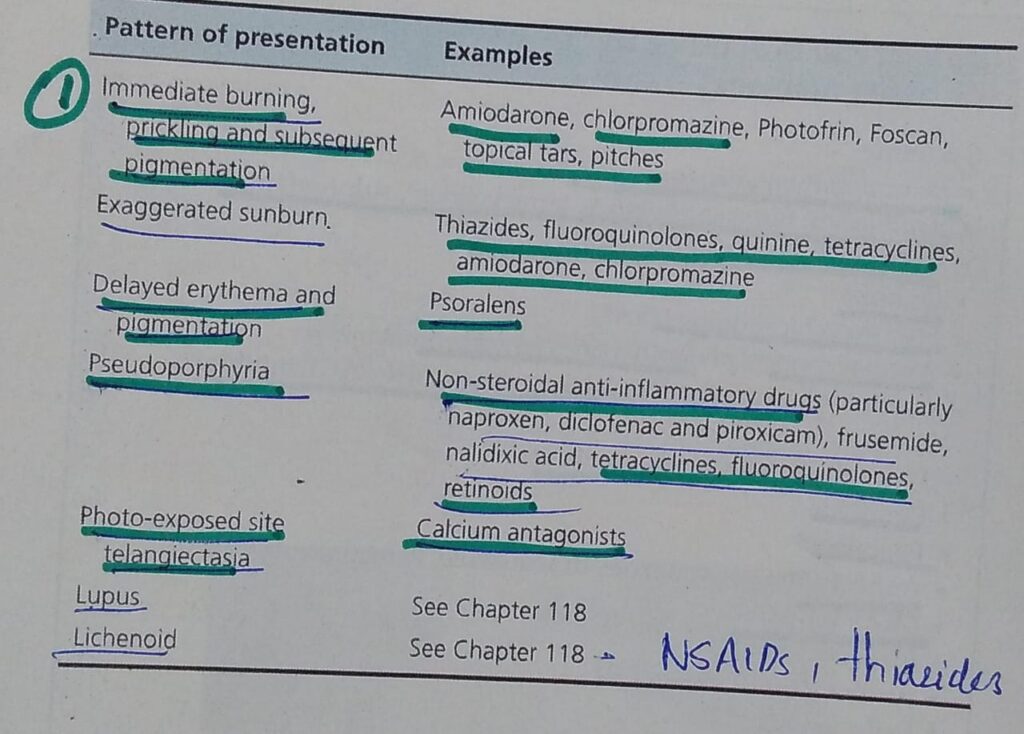
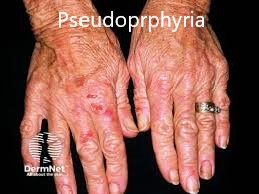
DRUG AND CHEMICAL INDUCED PHOTOSENSITIVITY:
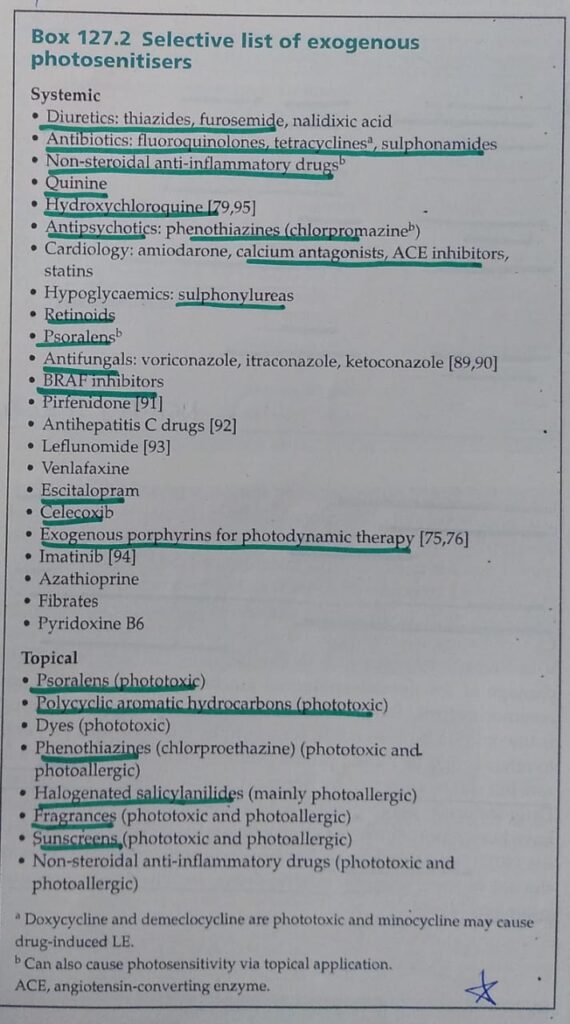
Clinical features


Complications, disease course and prognosis👇🏻
Management
General investigations done in acquired photodermatoses:
🔰 IMPORTANT TIP
The above voice notes have detailed discussion on idiopathic photodermatoses. Listen to them to get the concept and then practice from mcqs.
ETAS has given the best mcqs so far for this chap.
ACNE:
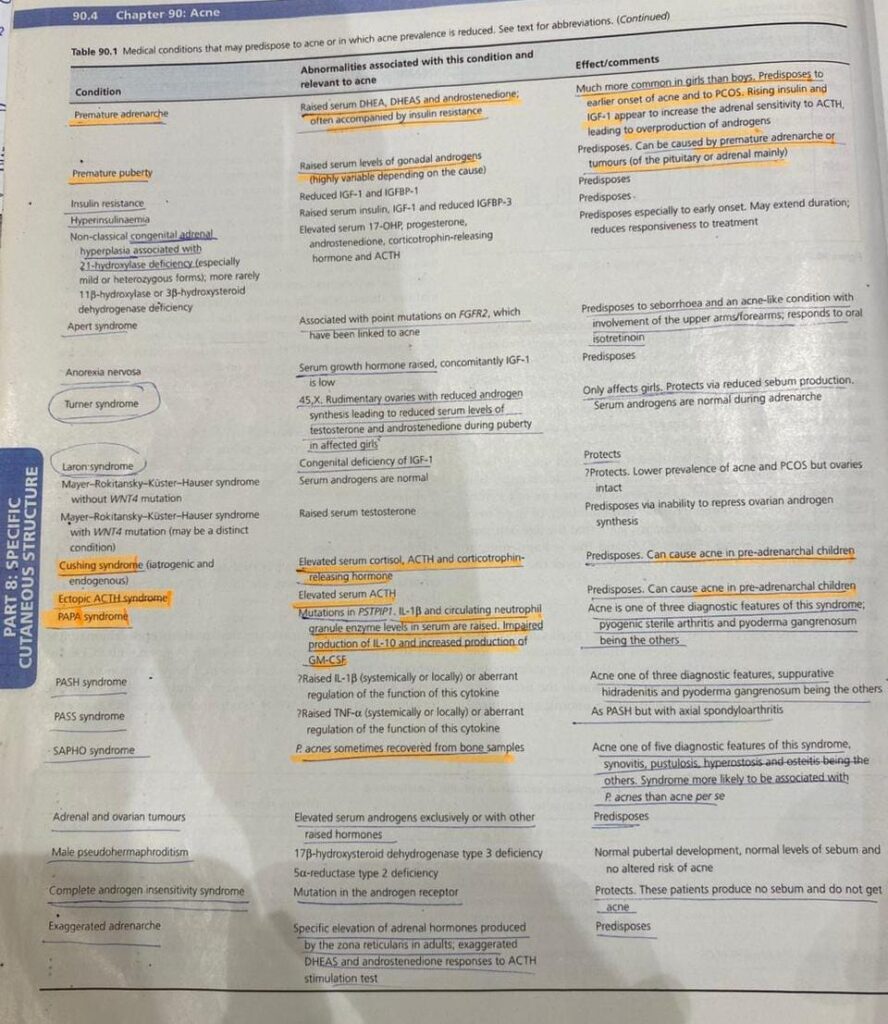
Associated diseases👇🏻
1️⃣ Polycystic ovarian syndrome
2️⃣ Late onset congenital adrenal hyperplasia / Non classical congenital adrenal hyperplasia
3️⃣ Cushing disease / Cushing syndrome
4️⃣ Acromegaly
5️⃣ SAPHO syndrome (Synovitis, acne, pustulosis, hyperostosis, Osteitis)
6️⃣ HAIR- AN syndrome (Hyperandrogenism, insulin resistance, acanthosis nigricans)
7️⃣ SAHA syndrome (Seborrhoea, acne, hirsutism, androgenetic alopecia)
8️⃣ PAPA syndrome (Pyogenic sterile arthritis, pyoderma gangrenosum, acne)
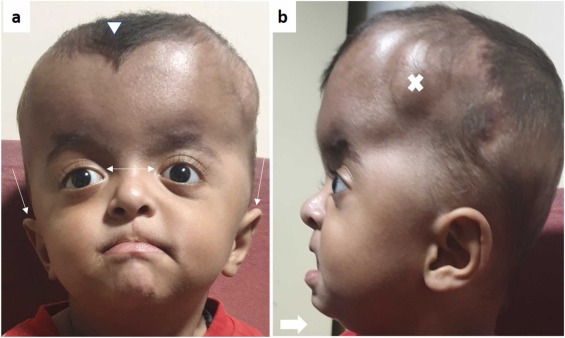
9️⃣ Apert syndrom

🔟 Premature adrenarche
🔰 Syndromes associated with protective effects against acne

🔰 Drug induced acne
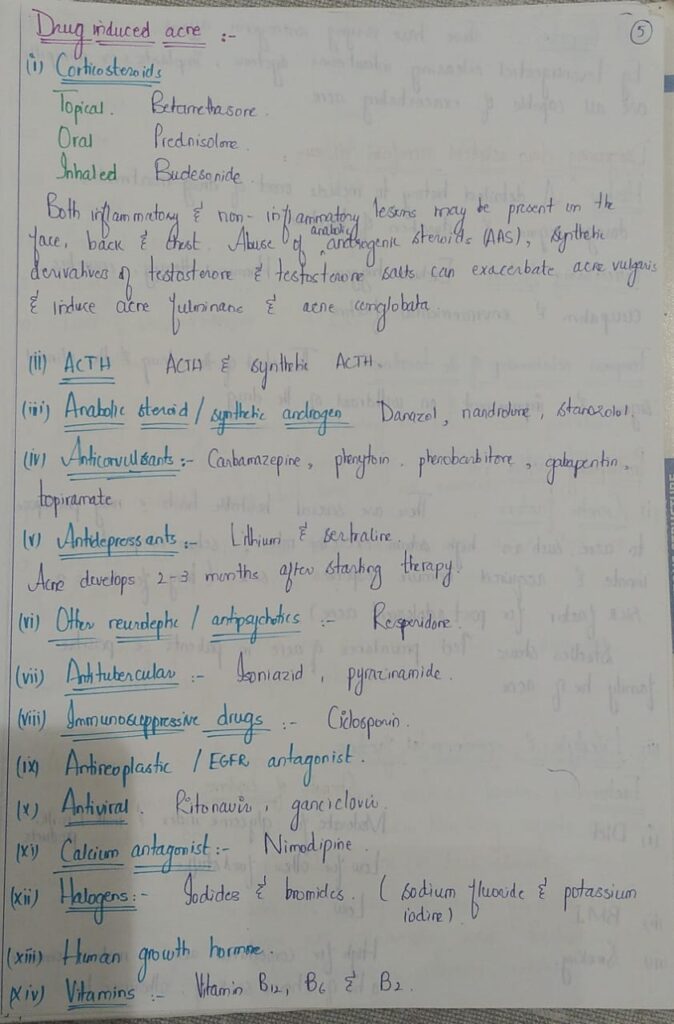

CHINa MTV is the mneumonic
🔰 Predisposing factors for acne
🔰 Pathophysiology
🔰 Clinical features




🔰 Variants of Acne
1️⃣ Acne associated with Psychological problems👇🏻
🔯 Acne excoriee

🔯 Other psychological disorders
2️⃣ Granulomatous acne
3️⃣ Acne mechanica
🔰 Differential diagnosis
🔰 Clinical severity
🔰 S/s tht may indicate an underlying endocrinopathy suggesting the need for investigation👇🏻

🔰Complications
🔰Management

1️⃣ Comedonal acne
2️⃣ Mild to moderate Papulopustular acne
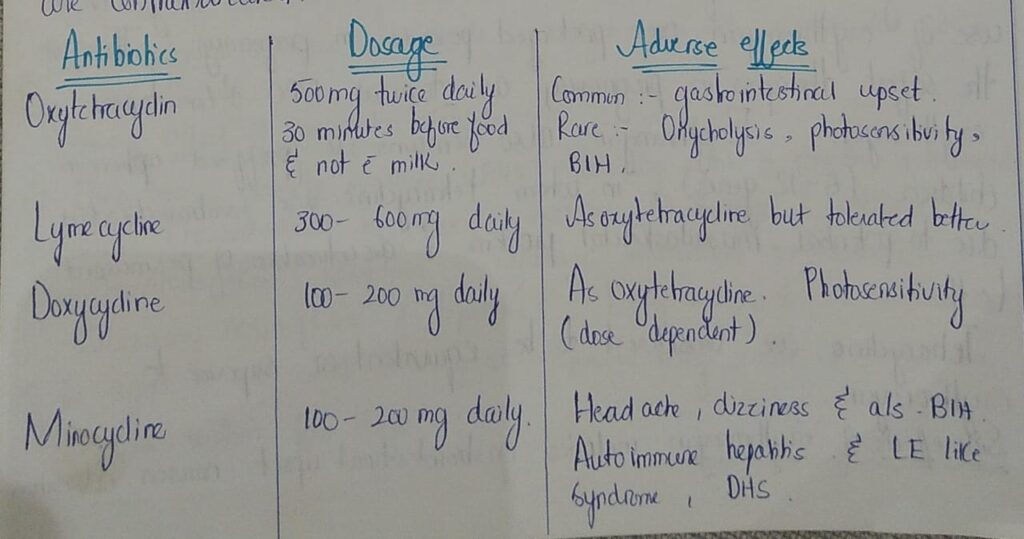
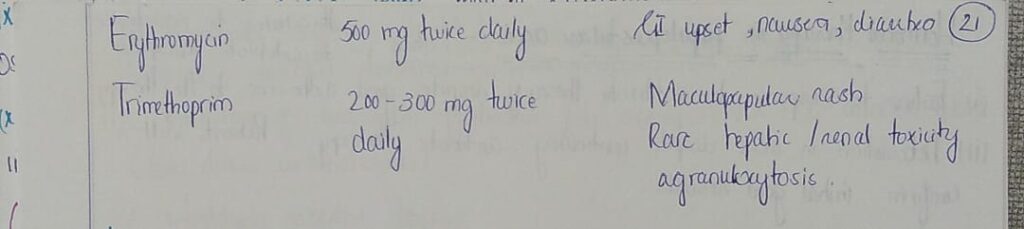
Systemic antibiotics
How to avoid bacterial resistance
How to suspect poor response to antibiotics
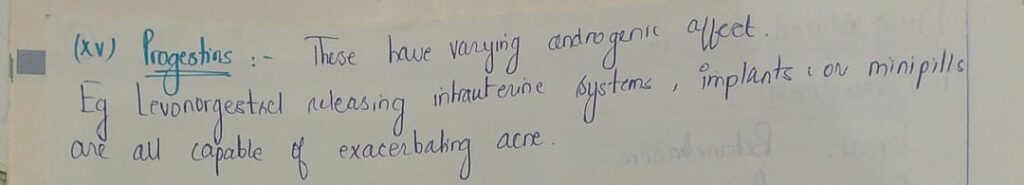
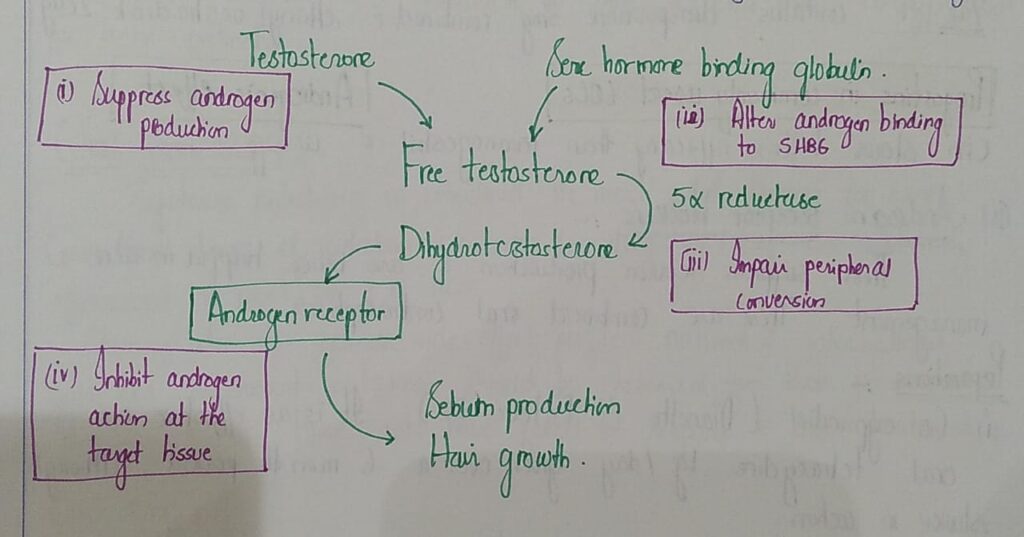
🔰 Hormonal therapy in papulopustular acne
1️⃣ Oral contraceptives
2️⃣ Androgen receptor blockers
3️⃣ Spironolactone
🔰 Severe acne
🔯 Oral Isotretinoin
Pharmacokinetics, adverse effects, contraindications and drug interaction has been covered in the drugs group
🔰 Other treatment modalities for acne
ACNE FULMINANS:

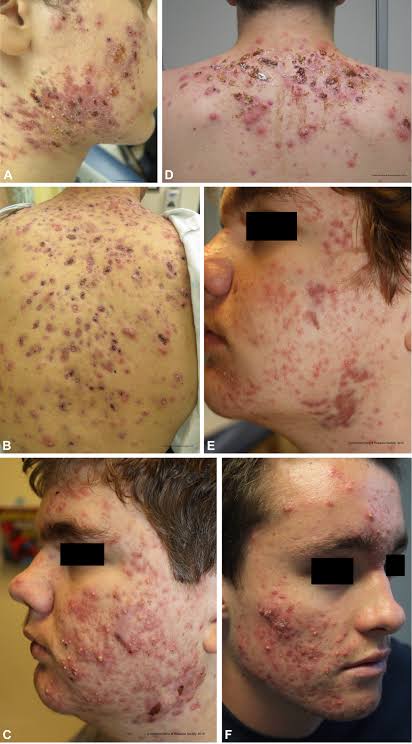
ACNE CONGLOBATA:
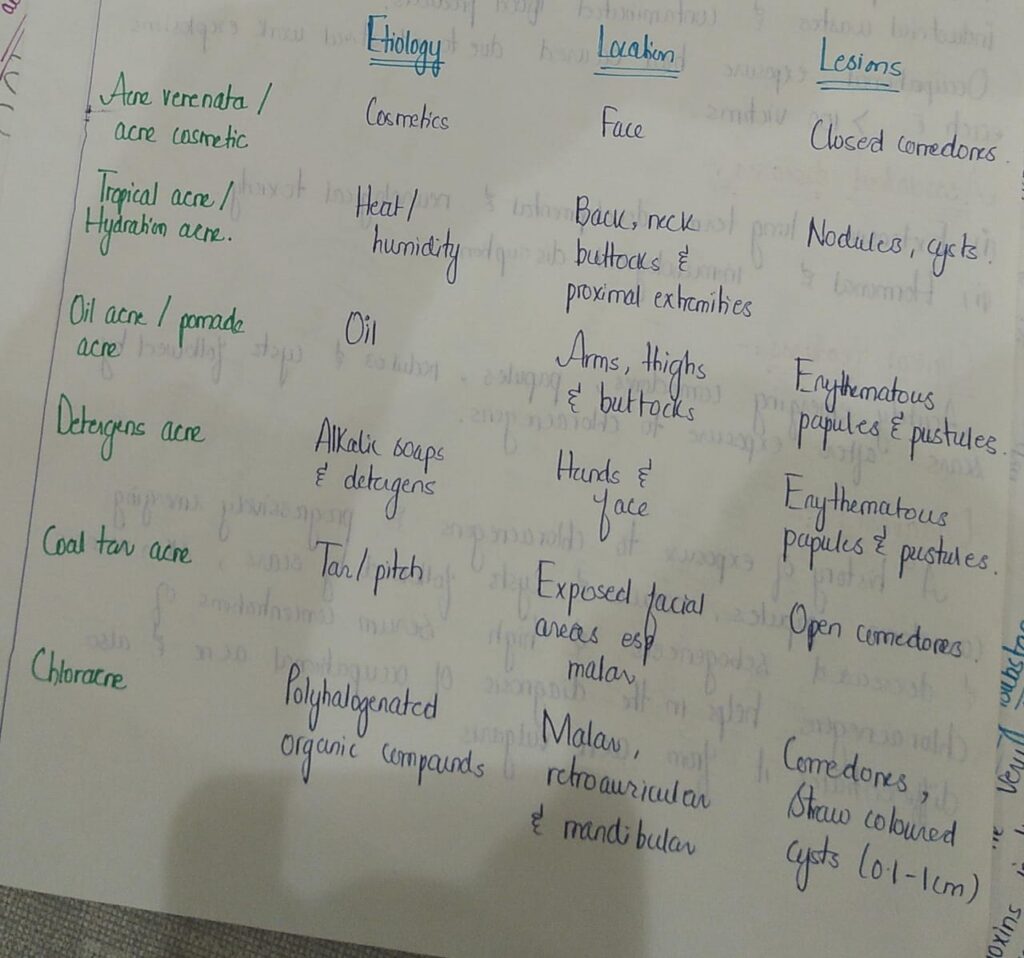
OCCUPATIONAL ACNE:
PRE-PUBERTAL ACNE:


🔰 Important note🔰
Cover this chap by listening to above voice notes and only solve n practice mcqs for exams.
U can safely skip reading this chap from rooks.
Test:
🔰 Imp for identification in toacs




